Abstract
Objective
The purpose of this study was to compare the skeletal, dental, and soft-tissue treatment effects of nonextraction therapy using the modified C-palatal plate (MCPP) to those of premolar extraction (PE) treatment in adult patients with Class II malocclusion.
Methods
Pretreatment and posttreatment lateral cephalographs of 40 adult patients with Class II malocclusion were retrospectively analyzed. The MCPP group comprised 20 patients treated with total arch distalization of the maxillary arch while the PE group comprised 20 patients treated with four PE. Fifty-eight linear and angular measurements were analyzed to assess the changes before and after treatment. Descriptive statistics, paired t-test, and multivariate analysis of variance were performed to evaluate the treatment effects within and between the two groups.
Results
The MCPP group presented 3.4 mm of retraction, 1.0 mm of extrusion, and 7.3° lingual inclination of the maxillary central incisor. In comparison, the PE group displayed greater amount of maxillary central incisor retraction and retroclination, mandibular incisor retraction, and upper lip retraction (5.3 mm, 14.8°, 5.1 mm, and 2.0 mm, respectively; p < 0.001 for all). In addition, the MCPP group showed 4.0 mm of distalization and 1.3 mm of intrusion with 2.9° distal tipping of the maxillary first molars.
Conclusions
These findings suggest the MCPP is an effective distalization appliance in the maxillary arch. The amount of incisor retraction, however, was significantly higher in the PE group. Therefore, four PE may be recommended when greater improvement of incisor position and soft-tissue profile is required.
The characteristics of patients undergoing orthodontic treatment tend to change over time, and the number of adults seeking active orthodontic treatment has been increasing over the past several decades.1 Older patients tend to show a greater demand for esthetic considerations during and after active treatment.2 Also, the preservation of existing dentoalveolar structures becomes a more critical issue in their treatment, and this mandates vigilant monitoring of the periodontal and occlusal statuses throughout the course of tooth movement.3
Usually, their demand can be resolved by various treatment options, which may include conventional premolar extractions or nonextraction approaches through space-gaining mechanics. When used with sound application of orthodontic mechanotherapy, premolar extraction therapy allows for the relief of crowding and improvement of the soft-tissue profile. However, it may also result in unexpected complications such as injury to the adjacent alveolar structures and occlusal disturbances.45 Moreover, the extraction space may relapse to open during the retention period, which may further jeopardize the stability of treatment outcome and lead to periodontal deterioration via local food impaction.6
Nowadays, the tendency towards choosing nonextraction approaches has been increasing because of the availability of effective and minimally invasive treatment modalities. Several strategies have been introduced to address the arch length discrepancy by gaining space through enamel stripping, arch expansion, and distalization of dentition. Moreover, the introduction of temporary anchorage devices (TADs) has enhanced the efficiency of nonextraction therapies via improved anchorage management.789101112
Among the array of various types of TADs, the miniscrew has gained popularity owing to its simplicity and noninvasive clinical application. However, the miniscrew also poses significant disadvantages such as a risk of contacting the roots of adjacent teeth and a limited range of action from the narrow interradicular space. A recent study suggested that the opportunities for successful nonextraction treatment could be further expanded if orthodontic miniscrews were used with interproximal reduction (IPR).13 This retrospective analysis of Class I malocclusion treatment demonstrated that distalization using buccal miniscrews coupled with IPR could resolve 3.6 mm of crowding in the maxillary dentition.13 However, considering that IPR should be performed at less than 50% of the enamel thickness, patients with moderate to severe crowding should be cautioned against opting for this treatment.14
In the search for more desirable TAD placement sites, the palate has been explored as an alternative for various appliance designs.151617181920 Interestingly, Lee21 have recently reported that the modified C-palatal plate (MCPP) resulted in a greater amount of distalization than did buccally positioned miniscrews. Also, it has been demonstrated that MCPPs could be effectively used for up to 4 mm of distalization of the maxillary first molars in adults.22 This finding may imply that the application of MCPPs could preclude IPR and possibly the extraction of premolars in cases in which these were previously required. Since only the residual space after resolving the arch-length discrepancy may be utilized to improve the molar relationships, the requirement for the amount of molar retraction may be more stringent in correcting Class II malocclusion rather than Class I malocclusion.
Presently, however, no study in the literature has analyzed the differences in the treatment effects between extraction and nonextraction treatments aided by the MCPP in Class II malocclusion. Therefore, the present study aimed to evaluate the skeletal, dental, and soft-tissue changes after four premolar extraction and total arch distalization facilitated by the MCPP in adult patients with Class II malocclusion, and to compare the treatment outcomes of the two different approaches.
The sample consisted of lateral cephalographs of 40 patients with Class II division 1 malocclusion. Twenty patients were treated with MCPP appliances via a nonextraction approach (MCPP group) and the remaining 20 patients were treated with four premolar extraction (PE group) at the Department of Orthodontics, Seoul St. Mary's Hospital, The Catholic University of Korea. Approval was obtained from the institutional review board of the Catholic University of Korea (No. MC17RES1005) and informed consent was obtained according to the tenets of the Declaration of Helsinki.
The inclusion criteria were as follows: adult status as evidenced by cervical vertebral maturation stage V23 at the time of treatment initiation, Class II molar and canine relationship, crowding less than 5 mm, positive overbite, overjet greater than 4 mm, no previous orthodontic treatment, no dental impaction or craniofacial anomaly, exclusive use of MCPP for distalization mechanics in the nonextraction group, and absence of adjunctive appliances such as headgear, functional appliance, and palatal expander during the active treatment period.
The MCPPs were installed using three 8-mm-length and 2.0-mm-diameter miniscrews (Jeil Medical Co., Seoul, Korea) in the paramedian area of the midpalatal suture. A palatal bar with two hooks extending along the palatal gingival margins of the teeth was banded to the maxillary first molars. Distalization was initiated by engaging elastomeric chains between the notches on the MCPP arm and the hooks on the palatal bar with approximately 300 g of force per side. During the same visit, fixed appliances with 0.022-inch slot brackets and bands (Tomy, Tokyo, Japan) were delivered on the maxillary and mandibular arches including the second molars. The patient appointment interval was kept between 3 to 4 weeks.
In the PE group, the maxillary first premolars were extracted. In the mandibular arch, however, the decision to extract either the first or second premolar was based on the amount of crowding and severity of Class II malocclusion. In addition, miniscrews (Jeil Medical Co.) were inserted mesial to the first molars as a supplemental anchorage when it was deemed necessary as judged by the orthodontist on the basis of the treatment goals in individual cases. Overall, seven patients in the PE group were treated with miniscrews in both the maxillary and mandibular arches during space closure. In both the arches, the anterior teeth were retracted en masse with sliding mechanics using elastomeric chains. The working wire used during retraction was made of 0.018 × 0.025-inch stainless steel or heavier wires. When necessary, interarch elastics were judiciously used throughout the treatment in both groups.
The pretreatment (T1) and posttreatment (T2) lateral cephalographs were digitized using an imaging software, V-Ceph 5.5 (Cybermed, Seoul, Korea), which was also used to calculate the linear and angular dimensions on the basis of the landmarks according to the definitions given in Figures 1, 2, and 3.
The horizontal reference line (HRL) was the Frankfort horizontal plane, and the vertical reference line (VRL) was a perpendicular line passing through the pterygoid point. In order to evaluate the movement of mandibular dentition within the mandible itself, the variables pertaining to the mandibular incisors and molars were re-analyzed in reference to the mandibular plane as a new mandibular HRL (mHRL: MeGo), and the line perpendicular to the mHRL and passing through the pogonion as a new mandibular VRL (mVRL: Perp to MeGo).
Fifty-eight linear and angular measurements were made by one examiner (HJL), and the variables at T1 and T2, and the differences between T1 and T2, were calculated. In order to access the accuracy and reliability of the measurements, 10 cases were randomly selected from each group for re-digitization and reanalysis at an interval of at least 2 weeks between the two measurements by the same examiner. Intraexaminer reliability was evaluated using the intraclass correlation coefficient, which was greater than 0.90 for all variables.
Statistical evaluation was performed using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA). Once the normal distribution of the measurements was confirmed using the Kolmogorov–Smirnov method, a paired t-test was used to evaluate the skeletal, dental, and soft-tissue changes from T1 to T2 within each group. A multivariate analysis of variance was performed to evaluate the differences between the groups at T1 and T2, and changes from T1 to T2 (T2–T1). Statistical significance level was initially set at 0.05 and, after Bonferroni correction, it became 0.001.
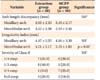
The MCPP group comprised 20 patients (4 men and 16 women) with a mean age of 22.4 ± 6.3 years while the PE group included 20 patients (1 man and 19 women) with a mean age of 24.6 ± 7.6 years. The mean treatment duration was 25.8 ± 10.8 months in the MCPP group and 28.3 ± 7.3 months in the PE group. Before treatment, no significant intergroup difference was observed in arch length discrepancies or severity of Class II malocclusion as assessed by the first molar key relationship (Table 1). The pretreatment irregularity index showed no significant intergroup difference in the maxillary arch, but it decreased more in the mandibular arch of the MCPP group than in the PE group.
In the MCPP group, 3.3 mm and 2.9 mm of crowding in the maxillary and mandibular arches were resolved, respectively. Similarly, in the PE group, 2.7 mm and 3.2 mm of crowding in the maxillary and mandibular arches were relieved, respectively. To illustrate the device used and typical treatment changes associated with the two treatment approaches, the intraoral appliances as well as the pretreatment and posttreatment lateral cephalographs are depicted in Figures 4 and 5, respectively.
When comparing the pretreatment variables between the groups, no significant main effect was observed (Table 2). Moreover, the results of univariate comparisons displayed no significant differences either.
The main effect of the multivariate analysis of the posttreatment variables, however, showed the presence of significant differences (Table 3, p = 0.020). Further, 11 variables showed significant differences in the univariate analysis, including the angulation and sagittal position of the maxillary and mandibular molars. Except for those variables, no significant differences were observed with regard to the skeletal, soft-tissue, and central incisor positions after treatment.
A similar trend was observed in the treatment changes between the two groups (Table 4). While no significant difference existed in the main effects, the univariate analysis presented significant differences in 18 variables related to the maxillary and mandibular molar positions between the two groups. Moreover, a significant intergroup difference in the treatment effects existed in the amount of retraction and lingual inclination changes in the maxillary and mandibular incisors (p < 0.001).
In addition, the treatment effect of intragroup analysis demonstrated a wider range of dentoskeletal changes (Table 4). SNA was the only skeletal variable of which decrease reached a statistically significant level in both groups (p < 0.001).
Regarding the maxillary central incisors, the MCPP group presented 3.35 mm of retraction, 1.03 mm of extrusion, and 7.25° lingual inclination; the corresponding values in the PE group were 5.34 mm, 0.91 mm, and 14.86°, respectively (p < 0.001). As for the mandibular central incisors, the MCPP group showed 1.66 mm of retraction, 1.05 mm of intrusion, and 3.30° lingual inclination in reference to the HRL and VRL. The PE group presented significantly greater retraction, intrusion, and lingual inclination of the mandibular central incisors (5.08 mm, 1.25 mm, and 10.56°, respectively; p < 0.001).
The maxillary first molars in the MCPP group showed distalization, intrusion, and distal tipping (3.97 mm, 1.31 mm, and 2.93°, respectively; p < 0.001), while those in the PE group showed protraction, extrusion, and mesial tipping (2.22 mm, 0.91 mm, and 3.33°, respectively; p < 0.001). Similarly, the mandibular first molars in the MCPP group displayed retraction and distal tipping (1.37 mm and 2.78°, respectively; p < 0.001) while those in the PE group showed protraction, extrusion, and mesial tipping (2.38 mm, 0.68 mm, and 3.29°, respectively; p < 0.001). The maxillary and mandibular second molars displayed similar movements as the first molars, but to a smaller magnitude.
In the area of soft-tissue change, no significant differences were found between the groups except in upper lip retraction (Table 4; p < 0.001). In contrast, the treatment changes within each group showed a significant increase in the nasolabial angle and retraction of both the upper and lower lips (p < 0.001).
This study aimed to compare the effects of MCPP and PE treatments on dentoskeletal structures and soft-tissue profile changes in adult patients with Class II malocclusion. Both approaches resulted in a significant improvement in overjet reduction, maxillary and mandibular incisor retraction, increase of nasolabial angle, and decrease of lip protrusion within each group. While the maxillary and mandibular molars showed significant distalization with distal tipping in the MCPP group, they showed the opposite movement in the PE group. In addition, four premolar extraction demonstrated a greater amount of maxillary and mandibular incisor distalization with increased retraction of the upper lip than did the nonextraction treatment.
Since the assimilation of premolar extraction into mainstream orthodontics, the decision to extract has remained one of the most critical clinical judgments in treatment planning. The space gained by extractions may be used for alleviating arch length discrepancy, correcting the molar relationship, and improving the patient profile. Ironically, although premolar extraction was initially promoted to increase the stability of treatment results by uprighting the incisors over the basal bone,24 maintaining the closed extraction space created another challenge to overcome during the retention period.
Garib et al.6 reported that the prevalence of reopening of extraction sites was 13.7%, and it was experienced by 30.2% of patients who had received four premolar extraction. This relapse tendency was greatest during the first year after appliance removal, and slowly decreased thereafter until the fifth year after treatment.6 Interestingly, the predisposition for the space to reopen was strengthened by the reduced amount of initial mandibular crowding and increased amount of mandibular incisor retraction during treatment. It may be suggested that the susceptibility of relapse may be attenuated by careful evaluation of arch length discrepancy before the extraction decision as well as by keeping the extent of incisor movement moderate during space closure.
The PE group in this study showed 5.34 mm of maxillary and 5.08 mm of mandibular incisor retraction after relieving 2.7 mm and 3.2 mm of crowding in the respective arches. In contrast, the MCPP group presented more moderate changes, which were 3.35 mm of maxillary and 1.66 mm of mandibular incisor retraction after resolving 3.3 mm of crowding in the maxillary and 2.9 mm in the mandibular arches. This significant difference between the groups may have been reflected as a difference in the soft-tissue changes, wherein greater upper lip retraction was observed in the PE group.
Previous studies have reported varying degrees of incisor retraction after premolar extractions.13252627 Unfortunately, meaningful comparisons between these studies were difficult because of the presence of numerous uncontrolled factors, such as differences in patient age, orthodontic technique used, and unexplained amounts of arch length discrepancies prior to treatments. Our results on maxillary and mandibular retractions, 5.34 mm and 5.08 mm, respectively, were greater than the 3.3 mm and 3.2 mm reported by Jung,13 whose patients received second premolar extractions for correcting Class I malocclusion. These differences may be explained by the facts that our patients received first premolar extractions, that seven patients in the PE group of our study received miniscrews as supplemental anchorage, and that our treatment may have required a greater degree of retraction to achieve the desired improvement in interarch relationship as well as soft-tissue profile.
The efficiency of TADs to distalize the whole dentition has been well characterized in the literature.8910111315161718192021222829 Reportedly, the amount of maxillary incisor retraction varied from the stationary position to 3.3 mm, mostly falling in the range near 2 to 3 mm. A few studies have even reported mild labial movement of the maxillary incisors after the use of TADs, such as miniscrew-supported skeletal distal jet.9 The significant maxillary incisor retraction of 3.35 mm in the MCPP group of our study was in accordance with that described in previous investigations, thus validating the effectiveness of MCPPs in distalizing movement in the anterior regions of the face. Notably, although no separate retraction appliance was used in the mandibular arch, the mandibular incisors moved lingually because of the combined use of the MCPP and Class III elastics. The magnitude of mandibular incisor retraction, which was 1.66 mm from the VRL, was statistically significant and, if 2.93 mm of mean crowding prior to treatment is considered, its significance is further strengthened. This finding attests the proficiency of the MCPP as an indirect anchor for distalizing the mandibular arch while simultaneously functioning as a direct anchor in the opposite arch.
The maxillary incisor in the MCPP group was vertically extruded by 1.03 mm and the mandibular incisor was vertically intruded by 1.11 mm from the HRL, with a net result of 0.64 mm of overbite reduction. This extrusion of the maxillary incisor was consistently described as one of the effects of the MCPP,202122 and this may suggest that, in challenging deep bite cases, the MCPP should be used with additional bite-opening mechanics, such as intrusion arches or miniscrews, for better vertical control. On the other hand, such movement may serve as an additional advantage when the treatment goal is to increase the amount of overbite or display of maxillary incisors in relation to the upper lip line.
In addition to the lingual movement of the incisors, the extent of molar retraction may present a useful clinical picture to estimate the efficiency of various distalization appliances since it is less affected by factors such as pretreatment arch length discrepancies or space gained through arch expansion during treatment. In this study, the maxillary first molar of the MCPP group was distalized by 3.97 mm, which was in accordance with that reported in previous investigations.202122 While the retraction amount described by most studies fell in the range of 2 mm to 4 mm, Kircelli et al.18 showed that their bone-anchored pendulum appliance successfully distalized the maxillary first molars by 6.4 mm in adolescent patients. In contrast, Oh et al.29 reported 1.5 mm of molar retraction assisted by buccal miniscrews in adults. It is unclear whether these differences stem from variations in appliance design, patient age, or unparalleled end points of individual treatment objectives. Nevertheless, it is evident that those with increased amount of distalization also tend to display greater degrees of distal tipping associated with the maxillary molars.1819
One of the merits of TAD-assisted distalization mechanics has been described as improved control over the vertical position of the maxillary posterior dentition.202122 The maxillary molars in the present study showed 1.0 to 1.3 mm of intrusion, which was congruous with that reported in previous investigations, which found stagnant to mildly intruded vertical positions of the maxillary molars after similar treatment mechanics. It is noteworthy that the design of the MCPP allows different treatment effects on the maxillary molars in the vertical plane as clinicians may take advantage of different force vectors by selecting one of three notches on the wing of the plate. This versatility of changing the direction of the force applied to the molars has been described as a merit of the MCPP along with the simplicity in placement and adjustment procedures.
In the area of soft-tissue improvement, our findings were congruent with those of other studies, which reported a similar range of soft-tissue response.71320212229 While both the PE and MCPP groups demonstrated marked reduction in nasolabial angle as well as the upper and lower lip positions within each group, the magnitude of change was overall greater in the PE group. Perhaps, this difference could be attributed to the fact that, in the mandible of the MCPP group, no rigorous space-gaining mechanics such as IPR or extraction was used except for Class III elastics anchored by the MCPP in the opposite arch. From a treatment mechanics perspective, it could be speculated that, if more aggressive distalization steps were taken in the mandible by using miniscrews or similar TADs, the MCPP could have functioned to move the maxillary incisors further to the point of intended overjet with a net result of greater retraction of the soft-tissue profile.
Over the past decades, the boundaries of nonextraction approaches have been widely expanded as more TADs have been integrated into clinical orthodontics. Moreover, space-gaining procedures such as IPR and arch development have been advocated as ways to expand the envelop of nonextraction treatment. In the presence of transverse discrepancy, palatal expansion therapies may be instituted to gain additional space in the maxillary arch while harmonizing the basal bone relationships. The excess space harvested by such supplemental procedures could be used to enhance the cogency of nonextraction therapies with greater impact on the treatment outcome.
This investigation was based on lateral cephalographs with inherent susceptibility to magnification, projection, and superimposition. When interpreting the results of the present study, it should be noted that the subjects were adults; the treatment response may differ in adolescents because their growth may moderate the treatment effects. Finally, as the impact of MCPP treatment in the anterior part of the face seemed to be bound by limited retraction of the mandibular incisors, it may be worthwhile to explore its distalization efficiency more thoroughly in conjunction with mandibular retraction modalities such as buccal miniscrews or miniplates in the future.
In the correction of Class II malocclusion in adults, the MCPP group displayed significant distalization of the incisors and molars in both the arches, with a reduction in the nasolabial angle as well as lip protrusion. The results of this study support the effectiveness of the MCPP as a direct anchor in the maxillary arch as well as an indirect anchor in the mandibular arch.
In addition, the present study found that significant difference in treatment effects existed in the area of the incisor and molar positions between the MCPP and PE groups, with consistently greater amount of incisor retraction in the PE group. To take advantage of the full retraction capacity of the MCPP, additional distalization modalities may be beneficial in the mandibular arch. Therefore, although the MCPP may be an effective appliance for total arch distalization, four premolar extraction treatment may be recommended when greater improvement of incisor retraction and soft-tissue profile is required in adult patients with Class II malocclusion.
Figures and Tables
Figure 1
Linear cephalometric variables used for analyzing the effects of four premolar extraction or the modified C-palatal plate.
Pt, Pterygoid; Or, orbitale; U, upper; L, lower; UL, upper lip; LL, lower lip; FH, Frankfort horizontal plane; HRL, horizontal reference line; VRL, vertical reference line; TVL, true vertical line; MeGo, menton to gonion line; Perp to MeGo, perpendicular line to MeGo passing the pogonion; 1, U1 crown to HRL; 2, U1 crown to VRL; 3, U1 apex to HRL; 4, U1 apex to VRL; 5, U6 crown to HRL; 6, U6 crown to VRL; 7, U6 apex to HRL; 8, U6 apex to VRL; 9, U7 crown to HRL; 10, U7 crown to VRL; 11, U7 apex to HRL; 12, U7 apex to VRL; 13, L1 crown to HRL; 14, L1 crown to VRL; 15, L1 apex to HRL; 16, L1 apex to VRL; 17, L6 crown to HRL; 18, L6 crown to VRL; 19, L6 apex to HRL; 20, L6 apex to VRL; 21, L7 crown to HRL; 22, L7 crown to VRL; 23, L7 apex to HRL; 24, L7 apex to VRL; 25, overjet; 26, overbite; 27, UL to TVL; 28, LL to TVL; 29, soft tissue A point to VRL; 30, soft tissue B point to VRL.

Figure 2
Angular cephalometric variables used for analyzing the effects of four premolar extraction or the modified C-palatal plate.
SN, Sella-nasion; FH, Frankfort horizontal plane; Go, gonion; Me, menton; U, upper; L, lower; 1, SNA; 2, ANB; 3, occlusal plane angle; 4, SN to mandibular plane angle; 5, U1 to FH angle; 6, U6 to FH angle; 7, U7 to FH angle; 8, L1 to FH angle; 9, L6 to FH angle; 10, L7 to FH angle; 11, nasolabial angle; 12, mentolabial angle.

Figure 3
Linear and angular cephalometric variables in reference to the mandible for analyzing the effects of four premolar extraction or the modified C-palatal plate.
Go, Gonion; Me, menton; mVRL, mandibular vertical reference line; Perp to, perpendicular to; L, lower; 1, L1 crown to mVRL; 2, L1 crown to GoMe; 3, L1 apex to mVRL; 4, L1 apex to GoMe; 5, L6 crown to mVRL; 6, L1 crown to GoMe; 7, L6 apex to mVRL; 8, L6 apex to GoMe; 9, L7 crown to mVRL; 10, L7 crown to GoMe; 11, L7 apex to mVRL; 12, L7 apex to GoMe; 13, L1 to GoMe angle; 14, L6 to GoMe angle; 15, L7 to GoMe angle.

Figure 4
Mid-treatment oral photographs in the premolar extraction and nonextraction (modified C-palatal plate) groups. A, Extraction treatment; B, Nonextraction treatment.

Figure 5
Representative changes in the lower third of the face based on the pretreatment (left) and posttreatment (right) lateral cephalographs in the premolar extraction and nonextraction groups. A, Extraction treatment; B, Nonextraction treatment.
Table 1
Distribution of arch length discrepancies, irregularity index scores, and severity of Class II malocclusion
References
1. Piao Y, Kim SJ, Yu HS, Cha JY, Baik HS. Five-year investigation of a large orthodontic patient population at a dental hospital in South Korea. Korean J Orthod. 2016; 46:137–145.

2. Fritz U, Diedrich P, Wiechmann D. Lingual technique--patients' characteristics, motivation and acceptance. Interpretation of a retrospective survey. J Orofac Orthop. 2002; 63:227–233.

3. Cardaropoli D, Gaveglio L, Abou-Arraj RV. Orthodontic movement and periodontal bone defects: Rationale, timing, and clinical implications. Semin Orthod. 2014; 20:177–187.

4. Peterson LJ, Ellis EE, Hupp JR, Tucker MR. Contemporary oral and maxillofacial surgery. 3rd ed. St. Louis, MO: Mosby;1998. p. 259–263.
5. Crossman IG, Reed RT. Long term results of premolar extractions in orthodontic treatment. Br J Orthod. 1978; 5:61–66.

6. Garib DG, Bressane LB, Janson G, Gribel BF. Stability of extraction space closure. Am J Orthod Dentofacial Orthop. 2016; 149:24–30.

7. Cope JB. Temporary anchorage devices in orthodontics: A paradigm shift. Semin Orthod. 2005; 11:3–9.

8. Choi YJ, Lee JS, Cha JY, Park YC. Total distalization of the maxillary arch in a patient with skeletal Class II malocclusion. Am J Orthod Dentofacial Orthop. 2011; 139:823–833.

9. Kinzinger GS, Gülden N, Yildizhan F, Diedrich PR. Efficiency of a skeletonized distal jet appliance supported by miniscrew anchorage for noncompliance maxillary molar distalization. Am J Orthod Dentofacial Orthop. 2009; 136:578–586.

10. Bechtold TE, Kim JW, Choi TH, Park YC, Lee KJ. Distalization pattern of the maxillary arch depending on the number of orthodontic miniscrews. Angle Orthod. 2013; 83:266–273.

11. Sugawara J, Kanzaki R, Takahashi I, Nagasaka H, Nanda R. Distal movement of maxillary molars in nongrowing patients with the skeletal anchorage system. Am J Orthod Dentofacial Orthop. 2006; 129:723–733.

12. Mah SJ, Kim JE, Ahn EJ, Nam JH, Kim JY, Kang YG. Analysis of midpalatal miniscrew-assisted maxillary molar distalization patterns with simultaneous use of fixed appliances: A preliminary study. Korean J Orthod. 2016; 46:55–61.

13. Jung MH. A comparison of second premolar extraction and mini-implant total arch distalization with interproximal stripping. Angle Orthod. 2013; 83:680–685.

14. Sheridan JJ. Air-rotor stripping update. J Clin Orthod. 1987; 21:781–788.
15. Sar C, Kaya B, Ozsoy O, Özcirpici AA. Comparison of two implant-supported molar distalization systems. Angle Orthod. 2013; 83:460–467.

16. Wilmes B, Nanda R, Nienkemper M, Ludwig B, Drescher D. Correction of upper-arch asymmetries using the Mesial-Distalslider. J Clin Orthod. 2013; 47:648–655.
17. Papadopoulos MA. Orthodontic treatment of Class II malocclusion with miniscrew implants. Am J Orthod Dentofacial Orthop. 2008; 134:604.e1–604.e16.

18. Kircelli BH, Pektaş ZO, Kircelli C. Maxillary molar distalization with a bone-anchored pendulum appliance. Angle Orthod. 2006; 76:650–659.
19. Escobar SA, Tellez PA, Moncada CA, Villegas CA, Latorre CM, Oberti G. Distalization of maxillary molars with the bone-supported pendulum: a clinical study. Am J Orthod Dentofacial Orthop. 2007; 131:545–549.

20. Kook YA, Kim SH, Chung KR. A modified palatal anchorage plate for simple and efficient distalization. J Clin Orthod. 2010; 44:719–730.
21. Lee SK. Comparison of treatment effect between the MPAP and buccally miniscrew groups in nonextraction case [Master's thesis]. Seoul: The Catholic University of Korea;2016.
22. Park CO, Sa'aed NL, Bayome M, Park JH, Kook YA, Park YS, et al. Comparison of treatment effects between the modified C-palatal plate and cervical pull headgear for total arch distalization in adults. Korean J Orthod. 2017; 47:375–383.

23. Grave K, Townsend G. Cervical vertebral maturation as a predictor of the adolescent growth spurt. Aust Orthod J. 2003; 19:25–32.
24. Tweed CH. Indications for the extraction of teeth in orthodontic procedure. Am J Orthod Oral Surg. 1944–1945; 42:22–45.

25. Basciftci FA, Usumez S. Effects of extraction and nonextraction treatment on class I and class II subjects. Angle Orthod. 2003; 73:36–42.
26. Saelens NA, De Smit AA. Therapeutic changes in extraction versus non-extraction orthodontic treatment. Eur J Orthod. 1998; 20:225–236.

27. Steyn CL, du Preez RJ, Harris AM. Differential premolar extractions. Am J Orthod Dentofacial Orthop. 1997; 112:480–486.





 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download