Abstract
Background and Purpose
Valproate is used as a prophylactic drug for migraine, but it is not be effective in all patients. We used medical records to investigate which clinical factors affected the response to valproate in patients with migraine as an original headache, and established a scoring system for predicting the clinical response to prophylactic therapy.
Methods
We investigated clinical factors from the medical records of 95 consistent responders (CRs) and 24 inconsistent responders (IRs) to valproate.
Results
Multivariate stepwise logistic regression analysis revealed that a history of hyperlipidemia and hay fever and the complication of depression or other psychiatric disorder were significant factors that independently contributed to a negative response, with odds ratios of 6.024 [no vs. yes; 95% confidence interval (CI)=1.616–22.222], 2.825 (no vs. yes; 95% CI=1.046–7.634), and 2.825 (no vs. yes; 95% CI=1.052–7.576), respectively. A predictive index (PI) of the clinical response to valproate in patients with migraine was calculated using the regression coefficients of these three factors as an integer, and the index was significantly higher for IRs than for CRs (1.46±1.10 vs. 0.69±0.74, mean±SD, p<0.001).
Migraine is the most common neurovascular headache, and is experienced by approximately 8.4% of the general population in Japan.1 Migraines are typically characterized by severe unilateral or bilateral head pain and occasional vision disturbance.1234 Migraines often cause significant disability and impaired quality of life, adversely affecting the activities of daily living and work-related productivity in many patients.1234
Drug therapies for migraine fall into acute and prophylactic categories. Acute therapy employs triptans for treating moderate-to-severe migraine attacks,5 while prophylactic therapy should be considered when such attacks are frequent or severe and when acute medication with triptans or nonsteroidal anti-inflammatory drugs is ineffective.5
Valproate is well established in the treatment of epilepsy, and it is thought to act by mimicking γ-aminobutyric acid. There is also evidence that valproate prevents migraine attacks, and it is already widely used for migraine management in the US and European countries.567 Hering and Kuritzky8 reported that valproate was effective in preventing migraine or reducing the frequency, severity, and duration of attacks in 86.2% patients over a 8-week period. Mathew et al.9 found that 48% of patients treated with divalproex experienced a ≥50% reduction in the frequency of migraine relative to baseline over 12 weeks. Shaygannejad et al.10 further suggested that treatment with valproate significantly decreases the duration, monthly frequency, and intensity of migraine after 8 weeks. Takeshima et al.11 reported that the efficacy of valproate was 59.7% at 2 months after commencing treatment. These findings together indicate that some patients with migraine do not respond well to treatment with valproate. If prophylactic treatment with a particular drug is unsuccessful, it can be substituted by a different prophylactic drug.12 Since changing the drug can initiate a therapeutic effect in some patients, it is possible that different factors are involved in the clinical responses to valproate and other prophylactic drugs.
Valproate was approved for migraine prophylaxis in Japan in October 2011, and it is now widely used there for migraine management. However, the factors that contribute to the clinical response of patients to valproate remain unknown. The ability to predict the response to valproate is particularly likely to improve the treatment of inconsistent responders (IRs).
The aim of this study was to identify significant predictive factors using clinical data associated with the response to valproate prophylactic therapy in patients with migraine as an original headache.
In total, 189 patients with migraine as original headache, who were prescribed prophylactic valproate by specialists, were admitted to the outpatient clinics of the Department of Neurology at Showa University Hospital and the Department of Neurology at Showa University East Hospital, Tokyo between September 2005 and June 2012. Headache was diagnosed according to the International Classification of Headache Disorders, Second Edition (ICHD-II)13 or the revised ICHD-II criteria.14 Patients with medication-overuse headache (MOH) or chronic migraine (CM) were asked about their original headache by specialists, who also confirmed the original headache and type of episodic migraine after curing the patients of MOH or CM. Patients with both CM and MOH were included if they had migraine as the original headache. The study cohort included not only patients with migraine but also those with both migraine and tension-type headaches, but excluded patients with only tension-type headache. Depression and other psychiatric disorders were diagnosed based on criteria in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.15
According to their clinical responses to valproate-containing drugs that are commercially available in Japan (Depaken, Kyowa Hakko Kirin, Tokyo, Japan; or Selenica, Kowa Pharmaceutical, Tokyo, Japan), patients were divided into consistent responder (CR) and IR groups, and they were asked whether their headaches were diminished by prophylactic therapy. The CRs were defined as those with a >50% decrease in the frequency of headaches (quantified in episode-days per month) at 3 months after initiating valproate treatment.16 We enrolled 119 of the 189 patients who were evaluated; the 70 patients were excluded for the following reasons: not revisiting the outpatient clinics (n=21), no records of the frequency of headache in medical records (n=24), compliance failure (n=7), and already using valproate before visiting our outpatient clinics (n=18).
The clinical responses to triptans were determined according to the responses of the responders and nonresponders. Responders treated with triptans were defined as those with diminished pain reported as either "mild" (within 4 h of oral or nasal administration) or "none" (within 2 h of oral or nasal administration) in at least two-thirds of attacks.317 Patients whose pain was not alleviated in three consecutively treated migraine attacks were defined as nonresponders.
This study was approved by the Institutional Ethics Committee of Showa University (Approval No. 148).
The medical examination of each patient involved using a headache diary and/or a headache questionnaire to obtain information about the pain location, frequency, and symptoms associated with the headache, and this was confirmed in an interview. In the case of MOH or CM, we confirmed the original headache and the type of episodic migraine after curing the patient of MOH or CM.
The following data were collected from all patients: age, sex, type of headache treated with valproate, original headache, type of episodic migraine, complication of depression or other psychiatric disorder, and medical history before commencing valproate treatment. We also collected data on the frequency, pain location, and symptoms associated with headache before applying the treatment. We investigated the valproate dosage, use of prophylactic drugs other than valproate, alleviation of headache symptoms, and use of triptans for 3 months after commencing valproate treatment.
A power analysis was performed using a publically available tool (http://www.dssresearch.com/toolkit/spcalc/power_a1.asp). In this power analysis we applied Cohen's criteria to categorize the effect sizes as follows (with alpha=5%): small (≥0.2 and <0.5), moderate (≥0.5 and <0.8), and large (≥0.8).18 We conducted univariate analysis using an unpaired Student's t-test for continuous variables and the χ2 test or Fisher's exact test for categorical variables. Multivariate stepwise logistic regression analysis was then conducted to identify independent factors associated with the clinical response to valproate. Variables with probability values of p<0.1 in the univariate analysis were included in the multivariate model.341719 The odds ratio (OR) and 95% confidence interval (CI) were calculated to evaluate the effects of each evaluated factor. A probability value of p<0.05 was considered to be indicative of statistical significance. Analyses were performed using SPSS 11.0 J for Windows (SPSS Japan, Tokyo, Japan).
The predictive index (PI)PI for the clinical response to prophylactic therapy using valproate was calculated for all patients by combining the factors selected according to the results of the multivariate stepwise logistic analysis. The values of the regression coefficient (β) of the selected factors were compared and scored as integers.3417 We defined the PI as the sum of all of these scores for each patient.
The study population consisted of 119 patients with migraine as their original headache (age, 37.4±12.9 years, mean±SD), comprising 11 (15%) men and 108 (85%) women. The 119 individuals suffered from migraine with the following characteristics: with an aura [migraine with aura (MA), n=8], without an aura [migraine without aura (MO), n=99], and combined type (MA+MO, n=12) (Table 1). The daily dosage of valproate was 100 mg (n=10), 200 mg (n=33), or 400 mg (n=76), and the efficacy of valproate (quantified as the proportion of CRs) was 79.8% (n=95) for the 119 patients (Table 1).
The type of headache that was treated with valproate did not differ between the CR and IR groups (p=0.329) (Table 1). The frequencies of a history of hyperlipidemia (p=0.013) and hay fever (p=0.048) differed significantly between the CR and IR groups (Table 1). The frequency of depression and other psychiatric disorders (panic disorder and personality disorder) also did not differ significantly between the CR and IR groups (29.5% vs. 50.0%, p=0.057), nor did the dose of valproate (p=0.985) (Table 1). Significant intergroup differences were found in allodynia of associated symptoms (p=0.035) (Table 2). There was also no intergroup difference detected in the use and efficacy of triptans (Table 3).
The results of the logistic multivariate analysis of allodynia of associated symptoms, a history of hyperlipidemia and hay fever, and the complication of depression or other psychiatric disorder are listed in Table 4. Logistic stepwise regression analysis identified hyperlipidemia, hay fever, and the complication of depression or other psychiatric disorder as significant factors that independently contributed to the response to valproate in patients with migraine, with ORs of 6.024 (95% CI=1.616–22.222), 2.825 (95% CI=1.046–7.634), and 2.825 (95% CI=1.052–7.576), respectively.
The PI was calculated using three factors that were selected according to the results of the logistic stepwise multivariate analysis. Scores were assigned using each β score and using the half-adjusted rules as follows: hyperlipidemia (yes), 2 points; hay fever (yes), 1 point; and complication of depression or other psychiatric disorder (yes), 1 point (Table 5). This resulted in the PI values ranging from 0 to 4; for example, PI=3 for a patient with hyperlipidemia and hay fever.
The PI—the sum of the scores of three factors—was calculated for each patient. The index was significantly higher for IRs (1.46±1.10) than for CRs (0.69±0.74, p<0.001). The distribution of the PI values of the patients is shown in Fig. 1. The patients were divided into three groups according to their PI values as follows: low (PI=0; CR:IR=44:5), moderate (PI=1; CR:IR=37:8), and high (PI≥2; CR:IR=14:11). The groups with low, moderate, and high indexes included 10.2%, 17.8%, and 44.0% of the IRs, respectively (Fig. 1, Table 6). The sensitivity and specificity for the high-index group (PI≥2) were 45.8% and 85.3%, respectively; the corresponding values for the low-index group (PI=0) were 79.2% and 46.3%, respectively (Table 6).
Using an alpha error of 5%, a post-hoc analysis for hyperlipidemia, hay fever, and the complication of depression or other psychiatric disorder revealed statistical powers of 0.65 (moderate), 0.50 (moderate), and 0.48 (low), respectively, based on the present sample size.
On the basis of multivariate stepwise logistic regression analysis and calculations of the PI, we found that a history of hyperlipidemia [including hypertriglyceridemia, hypercholesterolemia, and abnormally level of low-density lipoprotein (LDL) cholesterol] and hay fever and the complication of depression or other psychiatric disorder influenced the clinical response to valproate in patients with migraine. In addition, we demonstrated that patients with a high PI had a high risk of inconsistent responses to prophylactic valproate therapy.
Valproate is widely used for migraine prophylaxis567 and is considered an option in patients experiencing frequent attacks.16 The efficacy of valproate was found to be 59.7% in Japan at 2 months after commencing treatment.11 Although the efficacy of valproate (quantified as the proportion of CRs) was 79.8% in the present study, 72.6% of CR patients used lomerizine, which is another first-line prophylactic treatment for migraine administered in Japan. Moreover, we previously reported that the efficacy of lomerizine in combination with valproate was 89% in 53 patients with migraine.17 In contrast, the efficacy was 66.7% (CR, n=12; IR, n=6) for patients treated with valproate alone in the present study. Although a high proportion of the patients received combination therapy, no intergroup differences were found for the proportion receiving monotherapy.
The daily dose of valproate used in migraine prophylaxis typically ranges from 500 to 1,500 mg/day.20 In contrast, Kinze et al.21 recommended a serum level of valproate of <50 µg/mL for the prophylaxis of migraine because they found that the headache frequency was significantly lower even when patients were administered valproate at lower concentrations (21–50 µg/mL). Moreover, they recommended daily valproate doses of 500 to 600 mg because higher doses provided no additional benefit.21 The recommended dosage of valproate for migraine prophylaxis in Japan is 400–600 mg/day, and dosages of 100–400 mg/day were used in the present study. Furthermore, although the serum levels of valproate were not measured in all of the patients, the value measured in 12 patients in the IR group met the above-mentioned recommendation (45.3±13.3 µg/mL). Moreover, Takeshima et al.11 used 100–600 mg/day. Therefore, the dose of valproate administered in the present study was consistent with those that are generally applied in Japan.
Hyperlipidemia is a risk factor for CM but not for other types of migraine or the nonmigraine population.22 Tana et al.23 reported that the levels of total and LDL cholesterol were significantly higher in migraine patients with a high frequency and intensity of attacks than in those with a low frequency and intensity.23 Hyperlipidemia may act via the induction of platelet aggregation,24 since this induces changes in serum and platelet serotonin levels,25 and these changes might lead to vasodilation and subsequent migraine headache. A particularly interesting finding was a recent study showing that the administration of statins might be beneficial in migraine patients with a high vitamin D level.26 In the present study, although four patients with hyperlipidemia had started receiving treatment with statins prior to being treated with valproate, no differences between CR and IR groups were observed. The inclusion of only 13 patients with hyperlipidemia made it impossible to determine whether the effects of statins were involved in the prophylactic effects of valproate.
Patients with migraine are particularly prone to developing MOH.14 We previously reported that MOH patients have a higher incidence of depression than migraine patients.4 Depression and anxiety are risk factors for CM.22 In the present study, although the type of headache treated with valproate did not differ significantly between the IR and CR groups, the proportion of patients with depression or other psychiatric disorder (i.e., panic disorder or personality disorder) was higher in the IR group.
The mechanism of migraine is currently described by the trigeminovascular theory.27 The second branch of the trigeminal nerve terminates in a sinus, such as the ethmoid and sphenoid sinuses. Since the nasal symptoms associated with hay fever are known to be involved in sinus inflammation,28 it is possible that the inflammatory response in the sinus is related to the induction of migraine via stimulation of the trigeminal nerve in patients with hay fever. This is consistent with Aamodt et al.29 reporting that hay fever is associated with an increased frequency of migraine headaches. We found that hyperlipidemia and hay fever and the complication of depression or other psychiatric disorder, which are known to be risk factors for worse headache,123522232627 are risk factors for a negative response to valproate in migraine patients receiving prophylactic therapy. Since these factors did not contribute to the clinical response to lomerizine, which is another type of prophylactic drug used for migraine,17 these factors might be specific factors influencing the clinical response to valproate. However, we could not identify possible mechanisms underlying a negative response to valproate.
The sample size is a limitation of this study, as are the retrospective design, combined use of prophylactic drugs, and the lack of a long-term follow-up. Nevertheless, we established a PI using the factors of a history of hyperlipidemia and hay fever and the complication of depression or other psychiatric disorder. Patients with a PI of 0 should be treated with valproate because 89.8% of such patients responded positively to valproate in the present study. In contrast, it is likely that patients with a PI of ≥2 will not respond to valproate. Therefore, if an incomplete response to valproate prophylaxis is predicted when using this PI scoring system, other interventions should be considered in order to provide a better treatment outcome for patients with migraine. Future studies involving larger samples are required to improve the accuracy of the PI.
Figures and Tables
Fig. 1
Distribution of patients according to the predictive index (PI) for the response to valproate in patients with migraine. The PI for the clinical response to valproate was calculated as follows: PI=2×hyperlipidemia (yes)+1×hay fever (yes)+1×depression or other psychiatric disorder (yes). The index was significantly higher for inconsistent responders (IRs) than for consistent responders (CRs; 1.46±1.10 vs. 0.69±0.74, p<0.001).

Table 1
Backgrounds of patients

Table 2
The feature of headache in patients

Table 3
Use of triptans
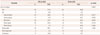
Table 4
Multivariate analysis of predictive factors of response to valproate

Table 5
Scoring system for response to valproate

| Variable | Score* |
|---|---|
| Past history of hyperlipidemia | |
| Yes | 2 |
| No | 0 |
| Past history of hay fever | |
| Yes | 1 |
| No | 0 |
| Complication of depression and other psychiatric disorder | |
| Yes | 1 |
| No | 0 |
References
1. Sakai F, Igarashi H. Prevalence of migraine in Japan: a nationwide survey. Cephalalgia. 1997; 17:15–22.
2. Takeshima T, Ishizaki K, Fukuhara Y, Ijiri T, Kusumi M, Wakutani Y, et al. Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache. 2004; 44:8–19.

3. Ishii M, Sakairi Y, Hara H, Imagawa A, Shimizu S, Takahashi J, et al. Negative predictors of clinical response to triptans in patients with migraine. Neurol Sci. 2012; 33:453–461.

4. Onaya T, Ishii M, Katoh H, Shimizu S, Kasai H, Kawamura M, et al. Predictive index for the onset of medication overuse headache in migraine patients. Neurol Sci. 2013; 34:85–92.

5. Holland S, Silberstein SD, Freitag F, Dodick DW, Argoff C, Ashman E. Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: NSAIDs and other complementary treatments for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78:1346–1353.

6. Silberstein SD, Holland S, Freitag F, Dodick DW, Argoff C, Ashman E. Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Evidence-based guideline update: pharmacologic treatment for episodic migraine prevention in adults: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Headache Society. Neurology. 2012; 78:1337–1345.

7. Evers S, Afra J, Frese A, Goadsby PJ, Linde M, May A, et al. EFNS guideline on the drug treatment of migraine--revised report of an EFNS task force. Eur J Neurol. 2009; 16:968–981.

8. Hering R, Kuritzky A. Sodium valproate in the prophylactic treatment of migraine: a double-blind study versus placebo. Cephalalgia. 1992; 12:81–84.

9. Mathew NT, Saper JR, Silberstein SD, Rankin L, Markley HG, Solomon S, et al. Migraine prophylaxis with divalproex. Arch Neurol. 1995; 52:281–286.

10. Shaygannejad V, Janghorbani M, Ghorbani A, Ashtary F, Zakizade N, Nasr V. Comparison of the effect of topiramate and sodium valporate in migraine prevention: a randomized blinded crossover study. Headache. 2006; 46:642–648.

11. Takeshima T, Nishikawa W, Yoneda H, Kanki R, Yamashita S, Kikui S. Efficacy and safety of valproate in a series of Japanese migraine sufferers (in Japanese). Japanese J Headache. 2013; 39:306–311.
12. Géraud G, Lantéri-Minet M, Lucas C, Valade D. French Society for the Study of Migraine Headache (SFEMC). French guidelines for the diagnosis and management of migraine in adults and children. Clin Ther. 2004; 26:1305–1318.

13. Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders: 2nd edition. Cephalalgia. 2004; 24:Suppl 1. 9–160.
14. Headache Classification Committee. Olesen J, Bousser MG, Diener HC, Dodick D, First M, et al. New appendix criteria open for a broader concept of chronic migraine. Cephalalgia. 2006; 26:742–746.

15. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV. 4th ed. Washington, DC: American Psychiatric Association;1994.
16. Erdemoglu AK, Ozbakir S. Valproic acid in prophylaxis of refractory migraine. Acta Neurol Scand. 2000; 102:354–358.

17. Ishii M, Katoh H, Kurihara T, Kawamura M, Shimizu S. Characteristics of inconsistent responders to prophylaxis therapy with lomerizine in patients with migraine: a retrospective study in Japan. J Neurol Sci. 2013; 335:118–123.

18. Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Hillsdale, NJ: Lawrence Erlbaum Associates;1988.
19. Ishii M, Shimizu S, Sakairi Y, Nagamine A, Naito Y, Hosaka Y, et al. MAOA, MTHFR, and TNF-β genes polymorphisms and personality traits in the pathogenesis of migraine. Mol Cell Biochem. 2012; 363:357–366.

21. Kinze S, Clauss M, Reuter U, Wolf T, Dreier JP, Einhäupl KM, et al. Valproic acid is effective in migraine prophylaxis at low serum levels: a prospective open-label study. Headache. 2001; 41:774–778.

22. Chen YC, Tang CH, Ng K, Wang SJ. Comorbidity profiles of chronic migraine sufferers in a national database in Taiwan. J Headache Pain. 2012; 13:311–319.

23. Tana C, Santilli F, Martelletti P, di Vincenzo A, Cipollone F, Davì G, et al. Correlation between migraine severity and cholesterol levels. Pain Pract. 2015; 15:662–670.

24. Sener A, Ozsavci D, Oba R, Demirel GY, Uras F, Yardimci KT. Do platelet apoptosis, activation, aggregation, lipid peroxidation and platelet-leukocyte aggregate formation occur simultaneously in hyperlipidemia? Clin Biochem. 2005; 38:1081–1087.

26. Buettner C, Burstein R. Association of statin use and risk for severe headache or migraine by serum vitamin D status: a cross-sectional population-based study. Cephalalgia. 2015; 35:757–766.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download