Abstract
Neurologic deficits resulting from stroke remain largely intractable, which has prompted thousands of studies aimed at developing methods for treating these neurologic sequelae. Endogenous neurogenesis is also known to occur after brain damage, including that due to cerebral infarction. Focusing on this process may provide a solution for treating neurologic deficits caused by cerebral infarction. The phosphatidylinositol-3-kinase (PI3K) pathway is known to play important roles in cell survival, and many studies have focused on use of the PI3K pathway to treat brain injury after stroke. Furthermore, since the PI3K pathway may also play key roles in the physiology of neural stem cells (NSCs), eliciting the appropriate activation of the PI3K pathway in NSCs may help to improve the sequelae of cerebral infarction. This review describes the PI3K pathway, its roles in the brain and NSCs after cerebral infarction, and the therapeutic possibility of activating the pathway to improve neurologic deficits after cerebral infarction.
Stroke is one of the most common diseases and can induce several debilitating sequelae such as hemiplegia, aphasia, and dementia. The most important treatment for stroke thus far is thrombolysis, ideally within the so-called golden hour during which treatment is most likely to be effective, or at least within around 4.5 hours of symptom onset of a cerebral infarction.1 However, not all patients with a cerebral infarction are candidates for thrombolysis. Due to the risk of hemorrhage, there are strict inclusion and exclusion criteria for thrombolytic therapy, and because of the nature of the disease and its treatment, many patients must unfortunately live with long-term neurologic deficits. Numerous clinical trials have tested diverse putative neuroprotective agents and stem cells as treatments for these deficits, but almost all of them have been found to be ineffective. Therefore, continued effort is necessary to develop new therapeutic strategies for treating cerebral infarctions.
Ways of reversing the sequelae of cerebral infarction have been investigated, and various molecular pathways have been found to play critical roles in the pathogenesis. Based on these findings, several methods for blocking the pathogenic mechanisms have been proposed and developed. One pathogenic mechanism is the pathway involving phosphatidylinositide 3-kinase (PI3K), which has been investigated intensively.234 Since this pathway is important in cell survival and is significantly affected by ischemia, many attempts have been made to modulate it for the treatment of cerebral infarction and to prevent the programmed cell death caused by ischemic strokes.
Endogenous neural stem cells (NSCs) are well known to exist in the subventricular zone of the ventricles and subgranular zone of the hippocampus.56 They can proliferate under appropriate stress and then differentiate into various neuronal cells. Several studies have found that mild-to-moderate ischemic strokes can induce endogenous neurogenesis, and this neurogenesis may function to reduce the severity of neurologic sequelae.789 Therefore, methods for increasing endogenous neurogenesis have been sought in numerous studies. It has been established that the role of the PI3K pathway is crucial in the function of NSCs; therefore, if the PI3K pathway can be activated in NSCs after cerebral infarction, it could contribute to the recovery of subsequent neurologic deficits.
This review describes the PI3K pathway itself, its roles in the brain and in the activity of NSCs after cerebral infarction, and the possibility of using methods for activating the PI3K pathway in NSCs for the treatment of cerebral infarction.
It is well known that the PI3Ks are involved in various cellular functions, such as cell proliferation, growth, differentiation, motility, survival, and intracellular trafficking. The PI3K pathway is necessary for the survival of both neurons and NSCs.1011 PI3K is not a single enzyme, but rather a family of many different subtypes. The PI3K family is divided into three different classes (Class I, Class II, and Class III) based on the primary structure, regulation, and in vitro lipid substrate specificity.12 Among these, the Class I PI3Ks are the best understood and can be divided into two groups: Class IA (p110α, p110β, and p110δ) and Class IB (p110γ).13 The PI3K pathway is known to interact with the insulin receptor substrate (IRS) and is closely linked with the tumor suppressor phosphatase and tensin homolog (PTEN), which inhibits PI3Ks. When the IRS is activated by insulin, it activates PI3Ks and then regulates glucose uptake through diverse phosphorylation events. In detail, activated PI3Ks phosphorylate the 3-position hydroxyl group of the inositol ring of phosphatidylinositol (Ptdlns) to produce phosphoinositide Ptdlns(3,4,5)P3 from Ptdlns(4,5)P2.1415 Ptdlns(3,4,5)P3 activates many different downstream effectors, the most well known of which is Akt (protein kinase B).16 Akt phosphorylated by PI3Ks (pAkt) affects many important downstream signals, including mouse double minute 2 homolog (MDM2), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB), endothelial nitric oxide synthase (eNOS), mammalian target of rapamycin (mTOR), and S6 kinase, and inhibits Forkhead box O (FOXO)s, BAD, and glycogen synthase kinase (GSK)-3β.1617 These effects contribute to growth, translation, and cell-cycle regulation, glucose metabolism, DNA repair, and inhibition of apoptosis (Fig. 1).1617
Many chemicals affecting the PI3K pathway have been developed and investigated for the possibility of clinical applications. In particular, PI3K inhibitors are being investigated for the treatment of various cancers such as breast cancer and colorectal cancer,18 and PI3K activators including an IRS-1 substrate and platelet-derived growth factor receptor 740Y-P (PDGFR740Y-P) have been produced and used to enhance neuronal cell survival and differentiation.192021
The protective role of the PI3K pathway in the brain after cerebral infarction has been emphasized. It has been reported that ischemia and reperfusion both inhibit the PI3K pathway and induce apoptosis.23 On the other hand, activation of the PI3K pathway after ischemic injury has also been reported.422 Considering our previous findings19 and those of other investigators,23422 this discrepancy may be attributable to (among other possibilities) differences in evaluation time after ischemia or reperfusion injury, ischemic duration, or the use of different cell types such as neurons or astrocytes. The level of pAkt has been found to decrease in the hyperacute phase (less than 2 or 3 hours) after ischemic events, is slightly increased in the acute phase (from 2 or 3 hours to several hours), and then decreases 6-12 hours after an ischemic event.1923 In summary, ischemia or reperfusion inhibits the PI3K pathway and then induces cell death after ischemic injury. Ischemia or reperfusion inhibits PI3K and then reduces the phosphorylation of Akt. Decreased pAkt cannot inhibit BAD, caspase-3, or GSK-3β, for example, and these changes are associated with cell death after ischemia (Fig. 2).
These findings have prompted many studies demonstrating that activation of the PI3K pathway can contribute to the protection of neurons and the brain from ischemic injury. For example, vascular endothelial growth factor protects the brain after focal cerebral ischemia through activation of the PI3K pathway;24 the Ang1-Tie2-PI3K (angiopoietin-1-tunica intima endothelial kinase-2-PI3K) axis initiates survival responses in neural progenitor cells after oxygen and glucose deprivation;25 and humanin enhances the PI3K pathway and then contributes to protecting the brain against cerebral ischischemia and reperfusion injury.26 Together these findings indicate that appropriate activation of the PI3K pathway may be useful for promoting brain cell survival and thus reducing cell death after stroke.
NSCs are very important in the regeneration of brain tissue that has been damaged by cerebral infarction. It has been established that endogenous NSCs are located in the subventricular zone of the lateral ventricles and the subgranular zone of the hippocampus, and that they contribute to neurogenesis.56 Endogenous NSCs can differentiate into neurons, astrocytes, and oligodendrocytes in the presence of exogenous stimuli from their environment.27 It has also been reported that the role of the PI3K pathway is very important for the activity of NSCs. The PI3K/Akt pathway controls the proliferation, differentiation, and migration of endogenous NSCs.28 For example, several kinds of neurotrophic factors such as brain-derived neurotrophic factor (BDNF),29 fibroblast growth factor (FGF),28 transforming growth factor β (TGF-β),30 insulin-like growth factor-1 (IGF1),28 and C-X-C motif chemokine 12; also known as stromal-cell-derived factor 1α (SDF-1α) (CXCL12)31 activate the PI3K pathway, and activated PI3K/Akt affects mTORC1,32 Ras-related C3 botulinum toxin substrate 1 (Rac1),33 and Rho-kinase (ROCK)34 in NSCs.
In more detail, SDF-1α binds to C-X-C chemokine receptor type 4 (CXCR4) and activates PI3K, which in turn increases the phosphorylation of Akt-1.31 pAkt-1 induces the phosphorylation of the transcription factor FOXO3a,31 which contributes to the proliferation of NSCs.31 It has also been reported that activation of the PI3K and extracellular-signal-regulated kinase (ERK) pathways markedly enhances the brain-ischemia-induced proliferation of NSCs.35 A link between Akt and cAMP response-element-binding protein (CREB) also plays important roles in the proliferation of NSCs.28
The role of Akt in NSC differentiation remains a matter of controversy. Wang et al.36 and Zhang et al.37 reported that Akt mediates proneuronal basic-loop-helix transcription factor neurogenin 1 and another transcription factor, Brn-4, and that these factors regulate neuronal differentiation and neurite outgrowth. However, Jin et al.38 and Chan et al.39 suggested that the PI3K pathway is not required for the differentiation of NSCs. Therefore, further study is required to define the exact role of the PI3K pathway in the differentiation of NSCs.
Moreover, migration is one of the most important characteristics of NSCs. Activation of the receptor tyrosine kinase ErbB4 leads to activation of PI3K, and in turn increases the migration of NSCs.40 Li et al.41 showed that up-regulation of CXCR4 activates the PI3K pathways and then enhances the migration of NSCs toward SDF-1α.
Based on all of the above findings, it can be concluded that the PI3K pathway plays important roles in the proliferation, differentiation, and migration of NSCs (Fig. 3). In addition, there is indirect evidence supporting the importance of the role of the PI3K pathway in NSC activity. Groszer et al.42 reported that PTEN deletion directly induces activation of the PI3K pathway, thus increasing the proliferation of NSCs and decreasing their death in the subventricular zone. Thus, ultimately, the PI3K pathway plays key roles in the proliferation, differentiation, migration, and survival of NSCs.
It is clear that ischemia induces neuronal cell death in the brain via diverse mechanisms.43444546 However, it is interesting to note that a small amount of ischemia, such as that resulting from a transient cerebral ischemic attack, is also capable of inducing neurogenesis.4748 Ischemia transiently increases BDNF and nerve growth factor (NGF) in the brain.49 Based on the findings that epidermal growth factor (EGF), FGF-2, and BDNF augment the proliferation of NSCs and their differentiation to mature neurons in the brain,505152 it was thought that ischemia could transiently increase the expression of neurotrophic factors in the brain and then induce neurogenesis via the activation of endogenous NSCs. This hypothesis was indirectly supported by the finding that intraventricular injection of FGF-2 or EGF after brain ischemia increased the number of NSCs in the hippocampus.5354 However, it has not yet been established how these factors enhance neurogenesis in brain tissue that has been damaged by ischemia.
As described in the sections above, those neurotrophic factors secreted in response to ischemia strongly stimulate receptor tyrosine kinases and then activate PI3K/Akt. Activated Akt plays several crucial roles in the stimulation of adult neurogenesis from NSCs. This is supported by the findings that PI3K inhibitors such as LY294002, wortmannin, and PD98059 block DNA synthesis in NSCs and inhibit their proliferation.1155
In addition, the migration of NSCs to the lesion after ischemia is important for the regeneration of the damaged brain tissue. The PI3K pathway plays a critical role during the process of migration. PI3K/Akt activated by erythropoietin enhances the secretion of matrix metalloproteinase (MMP)-2 and MMP-9, which are very important in the migration of NSCs.56 This was reconfirmed by the finding that MMP inhibitors significantly reduce the migration of neuroblasts in the brain damaged by transient focal cerebral ischemia.57
A small degree of ischemia, such as that resulting from a transient cerebral ischemia, may potentiate NSC proliferation, differentiation, and migration. However, severe ischemia induces endogenous NSC damage, and a recent study showed that the clinical improvement after treatment with mesenchymal stem cells (MSCs) was associated with the degree of involvement of the subventricular zone of the lateral ventricle, which is well known to have a relatively high concentration of NSCs. This suggests that the treatment effect of MSCs is accentuated due to a smaller contribution to the repair by damaged endogenous NSCs.58 Given that prolonged and severe hypoxia inhibits the PI3K pathway, it is possible that large and severe infarcts inhibit the pathway in NSCs and then induce the NSC death.
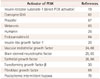
The findings described so far suggest that the PI3K pathway plays several crucial roles in neurogenesis by activating the proliferation, migration, and differentiation of NSCs. Recent studies have shown that the PI3K pathway mediates neurogenesis of NSCs via various downstream activators.596061 In detail, PI3K activates mTORC2 in NSCs and then enhances their survival, proliferation, and neurogenesis.59 Inactivation of GSK-3 directly by PI3K induces mothers against decapentaplegic homolog 1 of Sma (SMAD-1) and then contributes to axonal regeneration after axotomy.6061 In addition, several chemicals, drugs, and neurotrophic factors have been reported to activate PI3K (Table 1).62 636465666768
It is possible that appropriate activation of the PI3K pathway and enhanced endogenous neurogenesis with these activators may help the regeneration of brain tissue damaged by an ischemic stroke and the recovery of neurobehavioral functions impaired by cerebral infarction. There is a significant body of evidence indirectly supporting this hypothesis. For example, repetitive ischemic preconditioning inhibits brain damage after focal cerebral ischemia via activation of the PI3K pathway,69 heme oxygenase-1 (HO-1) protects hippocampal neurons from ischemic stroke via activation of the PI3K pathway,70 and formononetin activates the PI3K pathway and prevents ischemia or reperfusion injury of the brain.71
These findings suggest that direct activation of PI3K can contribute to protecting the brain after cerebral infarction and that NSCs play an important role in this protection, although there is no direct supporting evidence for this yet. From the therapeutic perspective, early activation of the PI3K pathway might be useful for protecting the brain in the hyperacute and acute stages of ischemic stroke, and its delayed activation would be helpful for restoring the ischemia-damaged brain in the subacute and early chronic stages. Further studies demonstrating the relationship between direct activation of the PI3K pathway, the protection of the brain after cerebral infarction, and regeneration by NSCs are necessary to confirm these hypotheses.
The PI3K signaling pathway plays several crucial roles in the survival, proliferation, differentiation, and migration of NSCs. This pathway also contributes to the protecting the brain after cerebral infarction following stroke. Further investigation into methods for enhancing endogenous neurogenesis via activation of the PI3K pathway is warranted.
Figures and Tables
Fig. 1
Role of the phosphatidylinositol-3-kinase (PI3K) pathway in cells. Akt: protein kinase B, BAD: Bcl-2-associated death promoter, FOXO1: forkhead box protein O1, GSK3β: glycogen synthase kinase 3β, MDM2: mouse double minute 2 homolog, mTOR: mammalian target of rapamycin, NF-kB: nuclear factor kappa-light-chain enhancer of activated B cells, PKC: protein kinase C, Ptdlns: phosphatidylinositol, PTEN: phosphatase and tensin homolog, RAC1: Ras-related C3 botulinum toxin substrate 1, SGK: serine/threonine-protein kinase, S6K: ribosomal protein S6 kinase.

Fig. 2
Alteration of the PI3K pathway after ischemia and reperfusion. Cas-3: caspase-3, Cyto C: cytochrome C, JNK: c-Jun N-terminal kinases.

Fig. 3
Molecular events in the PI3K pathway. CXCR4: C-X-C chemokine receptor type 4, EGFR: epidermal growth factor receptor, ERK: extracellular-signal-regulated kinase, FGFR: fibroblast growth factor receptor, Fkhr: forkhead transcription factor Foxo1, IR: insulin receptor, NGFR: nerve growth factor receptor, PDGFR: platelet-derived growth factor receptor, VEGFR: vascular endothelial growth factor receptor, XIAP: X-linked inhibitor of apoptosis protein.

Table 1
Chemicals, neurotrophic factors, and other activators of the PI3K pathway
| Activator of PI3K | References |
|---|---|
| Insulin receptor substrate-1 (direct PI3K activator) | 19 |
| Coenzyme Q10 | 62 |
| Propofol | 67 |
| Melatonin | 63 |
| Humanin | 26 |
| Endocannabinoid | 64 |
| Insulin-like growth factor-1 | 20 |
| Vascular endothelial growth factor | 24, 68 |
| Brain-derived neurotrophic factor | 29, 65 |
| Epithelial growth factor | 28, 66 |
| Transforming growth factor β | 30 |
| Fibroblast growth factor | 69 |
| Postischemic intermittent hypoxia | 70 |
Acknowledgements
This work was supported by a grant from the Korea Research Foundation (no. 2012R1A1B3000473), and a grant from the NanoBio R&D Program of the Korea Science and Engineering Foundation, funded by the Ministry of Education, Science and Technology (no. 2007-04717).
References
1. Del Zoppo GJ, Saver JL, Jauch EC, Adams HP Jr. American Heart Association Stroke Council. Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009; 40:2945–2948.

2. Zhao H. Ischemic postconditioning as a novel avenue to protect against brain injury after stroke. J Cereb Blood Flow Metab. 2009; 29:873–885.

3. Chalecka-Franaszek E, Chuang DM. Lithium activates the serine/threonine kinase Akt-1 and suppresses glutamate-induced inhibition of Akt-1 activity in neurons. Proc Natl Acad Sci U S A. 1999; 96:8745–8750.

4. Miyawaki T, Ofengeim D, Noh KM, Latuszek-Barrantes A, Hemmings BA, Follenzi A, et al. The endogenous inhibitor of Akt, CTMP, is critical to ischemia-induced neuronal death. Nat Neurosci. 2009; 12:618–626.

5. Temple S. Division and differentiation of isolated CNS blast cells in microculture. Nature. 1989; 340:471–473.

7. Yagita Y, Kitagawa K, Ohtsuki T, Takasawa Ki, Miyata T, Okano H, et al. Neurogenesis by progenitor cells in the ischemic adult rat hippocampus. Stroke. 2001; 32:1890–1896.

8. Parent JM, Vexler ZS, Gong C, Derugin N, Ferriero DM. Rat forebrain neurogenesis and striatal neuron replacement after focal stroke. Ann Neurol. 2002; 52:802–813.

9. Thored P, Arvidsson A, Cacci E, Ahlenius H, Kallur T, Darsalia V, et al. Persistent production of neurons from adult brain stem cells during recovery after stroke. Stem Cells. 2006; 24:739–747.

10. Crowder RJ, Freeman RS. Phosphatidylinositol 3-kinase and Akt protein kinase are necessary and sufficient for the survival of nerve growth factor-dependent sympathetic neurons. J Neurosci. 1998; 18:2933–2943.

11. Li BS, Ma W, Zhang L, Barker JL, Stenger DA, Pant HC. Activation of phosphatidylinositol-3 kinase (PI-3K) and extracellular regulated kinases (Erk1/2) is involved in muscarinic receptor-mediated DNA synthesis in neural progenitor cells. J Neurosci. 2001; 21:1569–1579.

12. Leevers SJ, Vanhaesebroeck B, Waterfield MD. Signalling through phosphoinositide 3-kinases: the lipids take centre stage. Curr Opin Cell Biol. 1999; 11:219–225.

13. Vanhaesebroeck B, Guillermet-Guibert J, Graupera M, Bilanges B. The emerging mechanisms of isoform-specific PI3K signalling. Nat Rev Mol Cell Biol. 2010; 11:329–341.

14. Knight ZA, Gonzalez B, Feldman ME, Zunder ER, Goldenberg DD, Williams O, et al. A pharmacological map of the PI3-K family defines a role for p110alpha in insulin signaling. Cell. 2006; 125:733–747.

15. Auger KR, Serunian LA, Soltoff SP, Libby P, Cantley LC. PDGF-dependent tyrosine phosphorylation stimulates production of novel polyphosphoinositides in intact cells. Cell. 1989; 57:167–175.

16. Liu P, Cheng H, Roberts TM, Zhao JJ. Targeting the phosphoinositide 3-kinase pathway in cancer. Nat Rev Drug Discov. 2009; 8:627–644.

17. Vivanco I, Sawyers CL. The phosphatidylinositol 3-Kinase AKT pathway in human cancer. Nat Rev Cancer. 2002; 2:489–501.

18. Mahadevan D, Chiorean EG, Harris WB, Von Hoff DD, Stejskal-Barnett A, Qi W, et al. Phase I pharmacokinetic and pharmacodynamic study of the pan-PI3K/mTORC vascular targeted pro-drug SF1126 in patients with advanced solid tumours and B-cell malignancies. Eur J Cancer. 2012; 48:3319–3327.

19. Noh MY, Kim YS, Lee KY, Lee YJ, Kim SH, Yu HJ, et al. The early activation of PI3K strongly enhances the resistance of cortical neurons to hypoxic injury via the activation of downstream targets of the PI3K pathway and the normalization of the levels of PARP activity, ATP, and NAD+. Mol Neurobiol. 2013; 47:757–769.

20. Laurino L, Wang XX, de la Houssaye BA, Sosa L, Dupraz S, Cáceres A, et al. PI3K activation by IGF-1 is essential for the regulation of membrane expansion at the nerve growth cone. J Cell Sci. 2005; 118(Pt 16):3653–3662.

21. Cuesto G, Enriquez-Barreto L, Caramés C, Cantarero M, Gasull X, Sandi C, et al. Phosphoinositide-3-kinase activation controls synaptogenesis and spinogenesis in hippocampal neurons. J Neurosci. 2011; 31:2721–2733.

22. Hasegawa Y, Suzuki H, Altay O, Zhang JH. Preservation of tropomyosin-related kinase B (TrkB) signaling by sodium orthovanadate attenuates early brain injury after subarachnoid hemorrhage in rats. Stroke. 2011; 42:477–483.

23. Noshita N, Sugawara T, Lewén A, Hayashi T, Chan PH. Copper-zinc superoxide dismutase affects Akt activation after transient focal cerebral ischemia in mice. Stroke. 2003; 34:1513–1518.

24. Kilic E, Kilic U, Wang Y, Bassetti CL, Marti HH, Hermann DM. The phosphatidylinositol-3 kinase/Akt pathway mediates VEGF's neuroprotective activity and induces blood brain barrier permeability after focal cerebral ischemia. FASEB J. 2006; 20:1185–1187.

25. Bai Y, Meng Z, Cui M, Zhang X, Chen F, Xiao J, et al. An Ang1-Tie2-PI3K axis in neural progenitor cells initiates survival responses against oxygen and glucose deprivation. Neuroscience. 2009; 160:371–381.

26. Xu X, Chua CC, Gao J, Chua KW, Wang H, Hamdy RC, et al. Neuroprotective effect of humanin on cerebral ischemia/reperfusion injury is mediated by a PI3K/Akt pathway. Brain Res. 2008; 1227:12–18.

27. Clarke DL, Johansson CB, Wilbertz J, Veress B, Nilsson E, Karlström H, et al. Generalized potential of adult neural stem cells. Science. 2000; 288:1660–1663.

28. Peltier J, O'Neill A, Schaffer DV. PI3K/Akt and CREB regulate adult neural hippocampal progenitor proliferation and differentiation. Dev Neurobiol. 2007; 67:1348–1361.

29. Nguyen N, Lee SB, Lee YS, Lee KH, Ahn JY. Neuroprotection by NGF and BDNF against neurotoxin-exerted apoptotic death in neural stem cells are mediated through Trk receptors, activating PI3-kinase and MAPK pathways. Neurochem Res. 2009; 34:942–951.

30. Park SM, Jung JS, Jang MS, Kang KS, Kang SK. Transforming growth factor-beta1 regulates the fate of cultured spinal cord-derived neural progenitor cells. Cell Prolif. 2008; 41:248–264.

31. Wu Y, Peng H, Cui M, Whitney NP, Huang Y, Zheng JC. CXCL12 increases human neural progenitor cell proliferation through Akt-1/FOXO3a signaling pathway. J Neurochem. 2009; 109:1157–1167.

32. Sato A, Sunayama J, Matsuda K, Tachibana K, Sakurada K, Tomiyama A, et al. Regulation of neural stem/progenitor cell maintenance by PI3K and mTOR. Neurosci Lett. 2010; 470:115–120.

33. Kendall SE, Najbauer J, Johnston HF, Metz MZ, Li S, Bowers M. Neural stem cell targeting of glioma is dependent on phosphoinositide 3-kinase signaling. Stem Cells. 2008; 26:1575–1586.

34. Leong SY, Faux CH, Turbic A, Dixon KJ, Turnley AM. The Rho kinase pathway regulates mouse adult neural precursor cell migration. Stem Cells. 2011; 29:332–343.

35. Shioda N, Han F, Fukunaga K. Role of Akt and ERK signaling in the neurogenesis following brain ischemia. Int Rev Neurobiol. 2009; 85:375–387.
36. Wang L, Zhang ZG, Zhang RL, Jiao ZX, Wang Y, Pourabdollah-Nejad DS, et al. Neurogenin 1 mediates erythropoietin enhanced differentiation of adult neural progenitor cells. J Cereb Blood Flow Metab. 2006; 26:556–564.

37. Zhang X, Zhang L, Cheng X, Guo Y, Sun X, Chen G, et al. IGF-1 promotes Brn-4 expression and neuronal differentiation of neural stem cells via the PI3K/Akt pathway. PLoS One. 2014; 9:e113801.

38. Jin L, Hu X, Feng L. NT3 inhibits FGF2-induced neural progenitor cell proliferation via the PI3K/GSK3 pathway. J Neurochem. 2005; 93:1251–1261.

39. Chan WS, Sideris A, Sutachan JJ, Montoya G JV, Blanck TJ, Recio-Pinto E. Differential regulation of proliferation and neuronal differentiation in adult rat spinal cord neural stem/progenitors by ERK1/2, Akt, and PLCγ. Front Mol Neurosci. 2013; 6:23.

40. Gambarotta G, Garzotto D, Destro E, Mautino B, Giampietro C, Cutrupi S, et al. ErbB4 expression in neural progenitor cells (ST14A) is necessary to mediate neuregulin-1beta1-induced migration. J Biol Chem. 2004; 279:48808–48816.

41. Li S, Deng L, Gong L, Bian H, Dai Y, Wang Y. Upregulation of CXCR4 favoring neural-like cells migration via AKT activation. Neurosci Res. 2010; 67:293–299.

42. Groszer M, Erickson R, Scripture-Adams DD, Lesche R, Trumpp A, Zack JA, et al. Negative regulation of neural stem/progenitor cell proliferation by the Pten tumor suppressor gene in vivo. Science. 2001; 294:2186–2189.

43. Garcia JH, Lossinsky AS, Kauffman FC, Conger KA. Neuronal ischemic injury: light microscopy, ultrastructure and biochemistry. Acta Neuropathol. 1978; 43:85–95.

44. Rothman S. Synaptic release of excitatory amino acid neurotransmitter mediates anoxic neuronal death. J Neurosci. 1984; 4:1884–1891.

45. Deshpande JK, Siesjö BK, Wieloch T. Calcium accumulation and neuronal damage in the rat hippocampus following cerebral ischemia. J Cereb Blood Flow Metab. 1987; 7:89–95.

46. Chen YH, Chiang YH, Ma HI. Analysis of spatial and temporal protein expression in the cerebral cortex after ischemia-reperfusion injury. J Clin Neurol. 2014; 10:84–93.

47. Endoh M, Pulsinelli WA, Wagner JA. Transient global ischemia induces dynamic changes in the expression of bFGF and the FGF receptor. Brain Res Mol Brain Res. 1994; 22:76–88.

48. Zhang RL, Chopp M, Roberts C, Liu X, Wei M, Nejad-Davarani SP, et al. Stroke increases neural stem cells and angiogenesis in the neurogenic niche of the adult mouse. PLoS One. 2014; 9:e113972.

49. Lindvall O, Ernfors P, Bengzon J, Kokaia Z, Smith ML, Siesjö BK, et al. Differential regulation of mRNAs for nerve growth factor, brain-derived neurotrophic factor, and neurotrophin 3 in the adult rat brain following cerebral ischemia and hypoglycemic coma. Proc Natl Acad Sci U S A. 1992; 89:648–652.

50. Craig CG, Tropepe V, Morshead CM, Reynolds BA, Weiss S, van der Kooy D. In vivo growth factor expansion of endogenous subependymal neural precursor cell populations in the adult mouse brain. J Neurosci. 1996; 16:2649–2658.

51. Kuhn HG, Winkler J, Kempermann G, Thal LJ, Gage FH. Epidermal growth factor and fibroblast growth factor-2 have different effects on neural progenitors in the adult rat brain. J Neurosci. 1997; 17:5820–5829.

52. Pencea V, Bingaman KD, Wiegand SJ, Luskin MB. Infusion of brain-derived neurotrophic factor into the lateral ventricle of the adult rat leads to new neurons in the parenchyma of the striatum, septum, thalamus, and hypothalamus. J Neurosci. 2001; 21:6706–6717.

53. Nakatomi H, Kuriu T, Okabe S, Yamamoto S, Hatano O, Kawahara N, et al. Regeneration of hippocampal pyramidal neurons after ischemic brain injury by recruitment of endogenous neural progenitors. Cell. 2002; 110:429–441.

54. Teramoto T, Qiu J, Plumier JC, Moskowitz MA. EGF amplifies the replacement of parvalbumin-expressing striatal interneurons after ischemia. J Clin Invest. 2003; 111:1125–1132.

55. Jin K, Mao XO, Del Rio, Jin L, Greenberg DA. Heparin-binding epidermal growth factor-like growth factor stimulates cell proliferation in cerebral cortical cultures through phosphatidylinositol 3'-kinase and mitogen-activated protein kinase. J Neurosci Res. 2005; 81:497–505.

56. Wang L, Zhang ZG, Zhang RL, Gregg SR, Hozeska-Solgot A, LeTourneau Y, et al. Matrix metalloproteinase 2 (MMP2) and MMP9 secreted by erythropoietin-activated endothelial cells promote neural progenitor cell migration. J Neurosci. 2006; 26:5996–6003.

57. Lee SR, Kim HY, Rogowska J, Zhao BQ, Bhide P, Parent JM, et al. Involvement of matrix metalloproteinase in neuroblast cell migration from the subventricular zone after stroke. J Neurosci. 2006; 26:3491–3495.

58. Lee JS, Hong JM, Moon GJ, Lee PH, Ahn YH, Bang OY. STARTING collaborators. A long-term follow-up study of intravenous autologous mesenchymal stem cell transplantation in patients with ischemic stroke. Stem Cells. 2010; 28:1099–1106.

59. Wahane SD, Hellbach N, Prentzell MT, Weise SC, Vezzali R, Kreutz C, et al. PI3K-p110-alpha-subtype signalling mediates survival, proliferation and neurogenesis of cortical progenitor cells via activation of mTORC2. J Neurochem. 2014; 130:255–267.

60. Zhang BY, Saijilafu , Liu CM, Wang RY, Zhu Q, Jiao Z, et al. Akt-independent GSK3 inactivation downstream of PI3K signaling regulates mammalian axon regeneration. Biochem Biophys Res Commun. 2014; 443:743–748.

61. Saijilafu , Hur EM, Liu CM, Jiao Z, Xu WL, Zhou FQ. PI3K-GSK3 signalling regulates mammalian axon regeneration by inducing the expression of Smad1. Nat Commun. 2013; 4:2690.

62. Choi H, Park HH, Lee KY, Choi NY, Yu HJ, Lee YJ, et al. Coenzyme Q10 restores amyloid beta-inhibited proliferation of neural stem cells by activating the PI3K pathway. Stem Cells Dev. 2013; 22:2112–2120.

63. Song J, Kang SM, Lee KM, Lee JE. The protective effect of melatonin on neural stem cell against LPS-induced inflammation. Biomed Res Int. 2015; 2015:854359.

64. Sütterlin P, Williams EJ, Chambers D, Saraf K, von Schack D, Reisenberg M, et al. The molecular basis of the cooperation between EGF, FGF and eCB receptors in the regulation of neural stem cell function. Mol Cell Neurosci. 2013; 52:20–30.

65. Dolcet X, Egea J, Soler RM, Martin-Zanca D, Comella JX. Activation of phosphatidylinositol 3-kinase, but not extracellular-regulated kinases, is necessary to mediate brain-derived neurotrophic factor-induced motoneuron survival. J Neurochem. 1999; 73:521–531.

66. Tsai YW, Yang YR, Sun SH, Liang KC, Wang RY. Post ischemia intermittent hypoxia induces hippocampal neurogenesis and synaptic alterations and alleviates long-term memory impairment. J Cereb Blood Flow Metab. 2013; 33:764–773.

67. Wang H, Wang G, Wang C, Wei Y, Wen Z, Wang C, et al. The early stage formation of PI3K-AMPAR GluR2 subunit complex facilitates the long term neuroprotection induced by propofol post-conditioning in rats. PLoS One. 2013; 8:e65187.

68. Zhu Y, Jin K, Mao XO, Greenberg DA. Vascular endothelial growth factor promotes proliferation of cortical neuron precursors by regulating E2F expression. FASEB J. 2003; 17:186–193.

69. Tu XK, Yang WZ, Chen JP, Chen Y, Chen Q, Chen PP, et al. Repetitive ischemic preconditioning attenuates inflammatory reaction and brain damage after focal cerebral ischemia in rats: involvement of PI3K/Akt and ERK1/2 signaling pathway. J Mol Neurosci. 2015; 55:912–922.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download