Abstract
Background and Purpose
Non-motor symptoms are common in Parkinson's disease (PD), and are the primary cause of disability in many PD patients. Our aim in this study was to translate the origin non-motor symptoms scale for PD (NMSS), which was written in English, into Korean (K-NMSS), and to evaluate its reliability and validity for use with Korean-speaking patients with PD.
Methods
In total, 102 patients with PD from 9 movement disorders sections of university teaching hospitals in Korea were enrolled in this study. They were assessed using the K-NMSS, the Unified Parkinson's Disease Rating Scale (UPDRS), the Korean version of the Mini-Mental Status Examination (K-MMSE), the Korean version of the Montgomery-Asberg Depression Rating Scale (K-MADS), the Epworth Sleepiness Scale (ESS), and Parkinson's Disease Questionnaire 39 (PDQ39). Test-retest reliability was assessed over a time interval of 10-14 days in all but one patient.
Results
The K-NMSS was administered to 102 patients with PD. The internal consistency and reliability of this tool was 0.742 (mean Cronbach's α-coefficient). The test-retest correlation reliability was 0.941 (Guttman split-half coefficient). There was a moderate correlation between the total K-NMSS score and the scores for UPDRS part I [Spearman's rank correlation coefficient, (rS)=0.521, p<0.001] and UPDRS part II (rS=0.464, p=0.001), but there was only a weak correlation between the total K-NMSS score and the UPDRS part III score (rS=0.288, p=0.003). The total K-NMSS score was significantly correlated with the K-MADS (rS=0.594, p<0.001), K-MMSE (rS=-0.291, p=0.003), and ESS (rS=0.348, p<0.001). The total K-NMSS score was also significantly and positively correlated with the PDQ39 score (rS=0.814, p<0.001).
Interest in non-motor symptoms in Parkinson's disease (PD) has increased in recently. Prominent among the non-motor symptoms of PD are cognitive disorder and dementia, dysautonomia, sleep disorders, and sensory disorders, including hyposmia.1 However, the non-motor symptoms of PD remain under recognized and under treated, despite being the main cause of disability in many PD patients. The recognition and proper management of non-motor symptoms are vitally important for delivering modern and comprehensive healthcare to PD patients. Moreover, non-motor symptoms strongly affect the quality of life of PD patients.2 The assessment of non-motor symptoms in patients with PD is therefore essential and has become an important approach for evaluating outcomes.
The original non-motor symptoms scale for PD (NMSS), which was written in English, was developed and validated to evaluate and quantify non-motor symptoms by addressing individual aspects such as cardiovascular function, sleep/fatigue, mood, perceptual problems, attention/memory, gastrointestinal function, urinary function, sexual function, and other miscellaneous items.3
In the present study, we translated the NMSS into Korean and evaluated its reliability and validity for use with Korean-speaking patients with PD. We also assessed its usefulness as a diagnostic measure for nonmotor symptoms in Korean patients with PD.
We recruited patients with PD from nine movement disorder centers of university-affiliated hospitals in Korea. PD was defined according to the clinical diagnostic criteria of the United Kingdom Parkinson's Disease Society Brain Bank.4 Written informed consent to participate was obtained from all patients. The Institutional Review Board of each participating hospital approved this study.
The following steps were used to translate the original English-language version of the NMSS into the final Korean version of the NMSS (K-NMSS), forward translation and backward translation, expert committee review, and pretesting of the penultimate version.
First, two independent bilingual translators translated the English version of the NMSS into Korean literally. A panel consisting of three authors (S.B. Koh, D.Y. Kwon, and J.S. Baik) reviewed the translations to form a single forward translation. Another bilingual translator translated the draft version of the K-NMSS back into English. The backwards-translated English version was also reviewed by the panel. Next, discrepancies between the original English version and the first-draft Korean translation were evaluated by the panel. Four patients were then interviewed to evaluate how they interpreted the translation. These processes resulted in the final K-NMSS (see Appendix).
The K-NMSS comprises 30 items covering 9 aspects: cardiovascular function, sleep/fatigue, mood/cognition, perceptual problems/hallucinations, attention/memory, gastrointestinal tract, urinary function, sexual function, and miscellaneous other nonmotor symptoms. The assessment period was "the past 1-month". The score for each domain is based on multiple levels of severity (from 0 to 3) and frequency scores (from 1 to 4). The total K-NMSS score ranges from 0 to 360.
Movement disorder specialists (all authors of this paper) applied the following battery of standard assessment measures: standard demographic forms, levodopa equivalent dose (LED),5 modified Hoehn and Yahr Scale (HYS),6 the Unified Parkinson's Disease Rating Scales (UPDRS) parts I, II, and III,7 and various other measures including the Korean version of the Mini-Mental Status Examination (K-MMSE)8 to measure cognitive function, the Korean version Montgomery-Asberg Depression Scale (K-MADS)9 to assess mood disorders, the Epworth Sleepiness Scale (ESS)10 to measure somnolence, the long-form Parkinson's Disease Questionnaires (PDQ39)11 to measure disease-specific health-related quality of life, and the K-NMSS. To evaluate test-retest reliability, the patients took the K-NMSS twice at times separated by an interval that was sufficiently long to minimize any memory of the test and practice efforts. The test-retest reliability was assessed over a time interval of 10-14 days.
Reliability was tested for both internal consistency and the stability of measures. Internal consistency was assessed by Cronbach's α-coefficient. The criterion value for α was ≥0.70. Test-retest reliability was assessed by the Guttman split-half coefficient (GSHC), for which values higher than 0.70 were considered acceptable. Spearman's rank correlation coefficients were used to identify associations with other variables as well as to analyze convergent validity with other scales. Logistic regression analysis was used to assess the relative contribution of clinical variables to the total K-NMSS score. SPSS 15.0 (SPSS, Chicago, IL, USA) was used for all statistical analyses.
Of the 102 Korean patients who were recruited, 52 were men and 50 were women. 101 of these patients completed the K-NMSS test twice. The age of the patients ranged from 43 to 84 years (65.03±9.55 years, mean±SD), and the duration of PD ranged from 1 to 276 months (43.64±48.17 months). Based on the modified HYS, there were 32 patients at stage 1, 12 at stage 1.5, 31 at stage 2, 17 at stage 2.5, 9 at stage 3, and 1 at stage 4. The LED was 397.19±329.97 mg/day.
The total K-NMSS score was 43.87±42.34 (range, 0-194) out of a possible maximum of 360 (Table 1). We compared our findings with data from the study of Chaudhuri et al.3 and a Chinese study (Fig. 1).12 Cronbach's α-coefficient for the K-NMSS was 0.742. All of the K-NMSS domains gave Cronbach's α coefficients of ≥0.70. Furthermore, the correlations between each domain with the total score were statistically significant [Spearman's rank correlation coefficient, (rS)=0.376-0.806, p<0.001)] (Table 1). The GSHC of the total K-NMSS scores of the 101 patients who performed the test twice was 0.941, and the test-retest reliabilities of the K-NMSS were between 0.705 and 0.965 (Table 2).
In this study, the total K-NMSS score was not significantly associated with age or disease duration, but was significantly associated with HYS (rS=0.231, p<0.05) and LED (rS=0.225, p<0.05; Table 3). There were significant correlations between the total K-NMSS score and the scores for UPDRS part I (rS=0.518, p<0.001), UPDRS part II (rS=0.330, p=0.001), and UPDRS part III (rS=0.288, p=0.003). There were also significant correlations between the domains of the K-NMSS (except for cardiovascular and sexual functions) and UPDRS part I scores and between the domains of the K-NMSS (except for perceptual problems) and UPDRS part II scores (Table 3). The mood/cognition, attention/memory, gastrointestinal, and urinary domains of the K-NMSS were significantly correlated with UPDRS part III (Table 3). In the miscellaneous domain, only excessive sweating was significantly correlated with disease duration, LED, HYS, and scores for UPDRS parts I, II, and III. The logistic regression analysis results are summarized in Table 4. Disease duration, LED, and HYS were not independent predictors of the total K-NMSS score. The total K-NMSS score was significantly correlated with K-MADS (rS=0.594, p<0.001), K-MMSE (rS=-0.291, p=0.003), and ESS (rS=0.348, p<0.001) scores. There were significant positive correlations between all domains of the K-NMSS (except for perceptual problems and sexual function), and K-MADS score (Table 5). The sleep/fatigue (rS=-0.218, p=0.028), attention/memory (rS=-0.371, p<0.001), gastrointestinal (rS=-0.293, p<0.001), and urinary (rS=-0.318, p=0.001) domains of the K-NMSS were significantly and negatively correlated with the K-MMSE score (Table 5). The cardiovascular function, sleep/fatigue, mood, attention/memory, and gastrointestinal domains of K-NMSS were significantly correlated with the ESS findings (Table 5).
The total K-NMSS score was significantly and positively correlated with the PDQ39 score (rS=0.814, p<0.001) (Fig. 2). All domains of the K-NMSS (except for sexual function), were significantly correlated with the PDQ39 score, and a higher mood/cognition domain score was associated with a worse PDQ39 score (rS=0.655, p<0.001) (Table 6).
Scales that can be used to evaluate and quantify the severity of nonmotor symptoms in patients with PD are fundamentally important for patient management. We translated the NMSS into Korean and evaluated its reliability and validity for use with Korean-speaking patients with PD. In our present study, nonmotor symptoms, as measured by the K-NMSS, were less severe those reported by Chaudhuri et al.3 The K-NMSS score in our study was 43.87±42.34, whereas the score of the NMSS used by Chaudhuri et al. was 56.46±40.66. The subject populations differed between these two studies; for example, our study subjects had a shorter disease duration (3.7 years vs. 6.4 years). However, the mean K-NMSS score was higher in our present study than that found using the NMSS in Chinese study.12 The mean K-NMSS domain scores in our study were similar to those found using the NMSS in the two aforementioned studies.
Cronbach's α-coefficient is a frequently used statistic in empirical research involving various domains. It estimates the reliability of a scale by determining the internal consistency of the test or the average correlation of domains within the test.13 It ranges in value from 0 to 1, with a higher score indicating that the generated scale is more reliable. A coefficient of 0.7 is considered to indicate acceptable reliability.14 The internal consistency reliability of the K-NMSS was satisfactory (Cronbach's α-coefficient=0.742), as was the test-retest reliability for the total K-NMSS score (GSHC=0.941). The test-retest reliabilities of all domains of NMSS were satisfactory, with GSHC between 0.705 and 0.965.
In our study, the K-NMSS score was not significantly correlated with age or disease duration. Nonmotor symptoms are heterogeneous and the domains of the NMSS are diverse. Furthermore, some nonmotor symptoms may emerge secondary to the underlying pathogenesis of the disease, while others are recognized side-effects of treatment. In addition, nonmotor symptoms may appear before the onset of motor symptoms. These factors may explain the low correlation between K-NMSS score and disease duration in our study.
The K-NMSS score was significantly correlated with LED, which can be explained by several factors. Many nonmotor fluctuations additional to classic motor fluctuations, may occur in PD.15,16 Nonmotor symptoms can be prominent during the "off" state, and patients in the "wearing off" state usually take a high dose of levodopa.15,16 A relationship between the "wearing off" phenomenon of nonmotor symptoms and levodopa dosage is one potential reason why the K-NMSS score was significantly correlated with LED. In addition, LED could be an indicator of the severity of PD, and nonmotor symptoms might emerge as a side-effect of dopaminergic treatment.
The K-NMSS score was significantly associated with measures related to PD (HYS and UPDRS), similar to what was found in the original study. These findings suggest that the severity of motor signs is associated with the burden of nonmotor symptoms.
The correlation between the K-NMSS score and UPDRS part I (mentation, behavior, and mood) and UPDRS part II scores (activities of daily living; rS=0.330-0.518, p<0.001) were higher than that between HYS and UPDRS part III scores (motor examination; rS=0.231-0.238, p<0.05). These results demonstrate that the K-NMSS is a useful tool for assessing the nonmotor symptoms of PD.
The K-NMSS score exhibited a significant positive correlation with K-MADS and ESS scores (rS=0.348-0.594, p<0.001). There was also a significant negative correlation between the K-NMSS and K-MMSE scores (rS=-0.291, p<0.05). The NMSS domains of mood/cognition, attention/memory, and sleep/fatigue were significantly correlated with K-MADS, K-MMSE, and ESS scores, respectively. These findings demonstrate that the domains of NMSS are adequate for assessing various nonmotor symptoms in PD patients.
There was a significant positive correlation between the total K-NMSS and PDQ39 scores (rS=0.814, p<0.001), and each K-NMSS domain was also significantly associated with the PDQ39 score (rS=0.302-0.655). These findings indicate that nonmotor symptoms, especially mood/cognition, attention/memory, and sleep/fatigue, are strongly associated with health-related quality of life in patients with PD.
In conclusion, our results demonstrate that the K-NMSS is a well-translated and validated version of the original NMSS, and hence is a useful instrument for the assessment of non-motor symptoms in Korean PD patients.
Figures and Tables
Fig. 1
Comparison of the mean score for each domain of NMSS between the current study, the original study, and the Chinese study. CV: cardiovascular, GI: gastrointestinal, NMSS: non-motor symptoms scale for Parkinson's disease.

Fig. 2
Correlation between the NMSS score and PDQ39. NMSS: non-motor symptoms scale for Parkinson's disease, PDQ-Sumi: Parkinson's disease questionnaires 39_summary index.
Table 1
Score for each NMSS domain and correlations between the domain scores and the total NMSS score
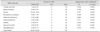
Table 2
Test-retest Gutmann Split-Half coefficient and correlation reliability for the Korean version non-motor symptoms scale for Parkinson's disease
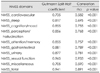
Table 4
Factors significantly associated with the each domain and total score of the Korean version non-motor symptoms scale: logistic regression model

Table 6
Correlation between NMSS and the summary index of PDQ39

*Spearman's rank correlation test, p<0.05, †Spearman's rank correlation test, p<0.001.
ADL: activities of daily living, Bodily: bodily discomfort, Cogn: cognitions, Comm: communication, Emot: emotional well-being, NMSS: non-motor symptoms scale for Parkinson's disease, PDQ39: Parkinson's Disease Questionnaires, Soc supp: social support.
Acknowledgements
We thank Dr. Chaudhuri for his permission to translate and use the NMSS in this research. This work was supported by grants from Sandoz Korea.
References
1. Chaudhuri KR, Odin P. The challenge of non-motor symptoms in Parkinson's disease. Prog Brain Res. 2010. 184:325–341.

2. Martinez-Martin P, Rodriguez-Blazquez C, Kurtis MM, Chaudhuri KR. NMSS Validation Group. The impact of non-motor symptoms on health-related quality of life of patients with Parkinson's disease. Mov Disord. 2011. 26:399–406.

3. Chaudhuri KR, Martinez-Martin P, Brown RG, Sethi K, Stocchi F, Odin P, et al. The metric properties of a novel non-motor symptoms scale for Parkinson's disease: Results from an international pilot study. Mov Disord. 2007. 22:1901–1911.

4. Hughes AJ, Daniel SE, Lees AJ. The clinical features of Parkinson's disease in 100 histologically proven cases. Adv Neurol. 1993. 60:595–599.
5. Langston JW, Widner H, Goetz CG, Brooks D, Fahn S, Freeman T, et al. Core assessment program for intracerebral transplantations (CAPIT). Mov Disord. 1992. 7:2–13.

7. Movement Disorder Society Task Force on Rating Scales for Parkinson's Disease. The Unified Parkinson's Disease Rating Scale (UPDRS): status and recommendations. Mov Disord. 2003. 18:738–750.
8. Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997. 15:300–308.
9. Ahn YM, Lee KY, Yi JS, Kang MH, Kim DH, Kim JL, et al. A validation study of the Korean-version of the Montgomery-Asberg depression rating scale. J Korean Neuropsychiatr Assoc. 2005. 44:466–476.
10. Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991. 14:540–545.

11. Peto V, Jenkinson C, Fitzpatrick R, Greenhall R. The development and validation of a short measure of functioning and well being for individuals with Parkinson's disease. Qual Life Res. 1995. 4:241–248.

12. Wang G, Hong Z, Cheng Q, Xiao Q, Wang Y, Zhang J, et al. Validation of the Chinese non-motor symptoms scale for Parkinson's disease: results from a Chinese pilot study. Clin Neurol Neurosurg. 2009. 111:523–526.

13. Santos JR. Cronbach's alpha: a tool for assessing the reliability of scales. J Ext. 1999. 37:2TOT3.
14. Assessing health status and quality-of-life instruments: attributes and review criteria. Qual Life Res. 2002. 11:193–205.
15. Bayulkem K, Lopez G. Nonmotor fluctuations in Parkinson's disease: clinical spectrum and classification. J Neurol Sci. 2010. 289:89–92.

16. Poewe W, Antonini A, Zijlmans JC, Burkhard PR, Vingerhoets F. Levodopa in the treatment of Parkinson's disease: an old drug still going strong. Clin Interv Aging. 2010. 5:229–238.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download