Abstract
Lamotrigine is an effective antiepileptic drug with few adverse effects. Nystagmus is one of the commonly observable signs of lamotrigine overdose, which may result from central nervous system involvement. However, the physiologic basis of lamotrigine-induced nystagmus is not fully understood. Here we report a patient who presented with lamotrigine-associated nystagmus that was probably related to cerebellar dysfunction.
Lamotrigine is an antiepileptic drug that has been used as an effective adjunctive treatment for refractory partial and generalized seizures. There is little published information on the effects of acute lamotrigine overdose. The reported acute neurological adverse effects of lamotrigine include two patients with downbeat nystagmus1 and one patient with ataxia and rotatory nystagmus.2 Here we describe a patient with reversible, downbeat, positional, and perverted head-shaking nystagmus (pHSN) and cerebellar dysfunction while being treated with lamotrigine for epileptic seizures. These oculomotor signs are thought to be attributable to an acute dysfunction of the vestibulocerebellum.
A 31-year-old woman reported dizziness, vomiting, unsteady gait, and frequent falling. She had a history of partial seizures with secondary generalization since 12 years of age, and was being treated with a combination of carbamazepine at 1200 mg/day, topiramate at 200 mg/day, and at lamotrigine 100 mg/day. The dosage of lamotrigine had been increased 5 weeks before this admission to 600 mg/day, after which this patient experienced intermittent dizziness, oscillopsia, and abdominal pain.
Several days prior to admission, our patient experienced dizziness, oscillopsia, nausea, and poor oral intake. Examination at that time revealed horizontal gaze-evoked nystagmus, positional downbeat nystagmus on straight-head hanging and on Dix-Hallpike maneuvers on both sides, and downbeat (perverted) nystagmus after about 30 s of horizontal head oscillations (see video recording).
On admission, the patient reported severe oscillopsia, dizziness, postural instability, and vomiting with abdominal pain. Examination with the aid of Frenzel goggles showed downbeat nystagmus in the primary position, which increased in downward and lateral gazes (see the video recording). Horizontal saccades and smooth pursuits were normal. However, downward smooth pursuit was mildly impaired. Rapid alternating movements of the hands and feet were slowed, and finger-to-nose and heel-to-shin tests showed mild dysmetria. Her gait was ataxic, and she could not walk unaided.
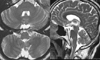
Her serum carbamazepine level was 9.4 µg/ml (normal range 8.12 µg/ml). A rotation test, as performed using the CHARTR® rotary vestibular test system (ICS Medical, IL, USA), showed normal gains and phases of the vestibuloocular reflex (VOR). Visual enhancement and visual cancellation of the VOR were within the normal ranges. During velocity-step rotation, the mean time constant and tilt suppression of the VOR were normal. Bithermal caloric tests showed symmetrical responses in both ears. Brainstem auditory evoked potentials were normal. An EEG acquired on the admission day did not show epileptiform discharges. MRI revealed no abnormal findings; there was no evidence of Arnold-Chiari malformation and nodular or floccular lesions (Fig. 1).
Following a diagnosis of lamotrigine toxicity, the patient's dose of lamotrigine was decreased to 100 mg/day; the doses of the other anticonvulsants that she was receiving were left unchanged. The patient's symptoms and signs were resolved in two subsequent examinations and did not recur during 6 months of follow-up.
Our patient developed downbeat, gaze-evoked, and positional pHSN, dysmetria, and ataxia after her lamotrigine dose had been increased to 600 mg/day. These signs immediately resolved upon decreasing lamotrigine back to 100 mg/day.
The spectrum of oculomotor abnormalities in our patient support the involvement of the vestibulocerebellum, especially the floccular lobe, which contains the gaze-velocity Purkinje cells with a downward on-direction for smooth pursuit, and participates in gaze holding.3
In primates, downbeat nystagmus in the primary position may be produced experimentally by flocculectomy, nodulectomy, midline section of the medulla, and pretectal lesions.4,5 The flocculus normally inhibits the central vestibular pathways from the anterior, but not from the posterior semicircular canals.7 Disinhibition of the anterior semicircular canal pathway due to floccular dysfunction would give rise to upward drift of the eyes during head oscillation and result in downbeat nystagmus.
Our patient also showed transient positional downbeat nystagmus, which is known to occur in posterior fossa lesions, particularly those in the vestibulocerebellum.4,5 In animal studies, floccular lesions cause constant downbeat nystagmus,4 and nodular lesions in cats also give rise to transient positional downbeat nystagmus.5 Downbeat nystagmus with floccular lesions is frequently associated with gaze-evoked and rebound nystagmus.3
pHSN is defined as nystagmus that develops in a plane other than that being stimulated by the head oscillation (i.e., downbeat or upbeat nystagmus after head shaking in the yaw plane). pHSN is explained by abnormal cross-coupling of vestibular responses,6 which has been attributed to lesions in the central vestibular pathway including the vestibulocerebellum. With regard to cerebellar lesions, pHSN may be ascribed to damage tothe central pathways from the anterior semicircular canals.
Most of the oculomotor disturbances in our patient could be explained by pharmacologically induced transient dysfunction of the vestibulocerebellum. Lamotrigine may thus give rise to reversible damage to the vestibulocerebellum.
Figures and Tables
References
1. Alkawi A, Kattah JC, Wyman K. Downbeat nystagmus as a result of lamotrigine toxicity. Epilepsy Res. 2005. 63:85–88.

2. O'Donnell J, Bateman DN. Lamotrigine overdose in an adult. J Toxicol Clin Toxicol. 2000. 38:659–660.
3. Leigh RJ, Zee DS. The Neurology of Eye Movements. 2006. 4th edn. New York: Oxford University Press;274–280.
4. Zee DS, Yamazaki A, Butler PH, Gucer G. Effects of ablation of flocculus and paraflocculus on eye movements in primate. J Neurophysiol. 1981. 46:878–899.

5. Fernandez C, Alzate R, Lindsay JR. Experimental observations on postural nystagmus. Lesions of the nodulus. Ann Otol Rhinol Laryngol. 1960. 69:94–114.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download