Abstract
Animal models are essential to studies of infectious diseases. The use of mice to test bacterial infection has been extensively reported. However, methods applied to clinical isolates, particularly for carbapenem-resistant bacteria, must be tailored according to the infection models and bacteria used. In this study, we infected 6-week-old female BALB/c mice intraperitoneally with different strains of resistant bacteria plus 3% hog gastric mucin. This method was found to be efficient and readily applicable for investigation of carbapenem-resisant Gram-negative pathogens (e.g., Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, and Acinetobacter baumannii) detected in Korea.
Increasing antimicrobial resistance can threaten public health, which leads to make a global action plan by world health organization (WHO), in order to strengthen the knowledge and evidence to reduce the incidence of drug resistant bacterial infection through research, and to optimize the use of antimicrobial agents [1]. The emergence of carbapenem-resistant bacteria in the clinical setting has become a major public health concern also in Korea. In particular, spread of carbapenem-resistant Gram-negative bacteria in healthcare environment has been focused due to the higher mortality and lack of optimal treatment [234]. To overcome this, researchers have developed several approaches to combat carbapenem-resistant bacteria, and animal models have been established to evaluate the efficacies of new antibiotics, antimicrobial agent combinations, proper route of antimicrobial administration, or in vivo pharmacokinetics/pharmacodynamics study.
Several animal infection models for carbapenem-resistant Gram-negative bacteria of clinical isolates have been reported [567891011], each of these models involved different methods and diverse mouse strains. BALB/c, C57BL/6, Swiss-Webster, and C3 mice have been used, and the site of bacterial administration has varied (e.g., intranasal, intratracheal, intraperitoneal, and intravenous). Diabetic and neutropenic models using BALB/c, ICR or A/J mice have been also developed [12]. Accordingly, the aim of this study was to design a murine peritonitis model using carbapenem-resistant Gram-negative bacteria that were clinical isolates from Korea.
The four bacterial strains used in this study were clinical isolates of carbapenem-resistant Gram-negative bacteria. Escherichia coli (EC-1), Klebsiella pneumoniae (KP-4), and Pseudomonas aeruginosa (PA-3) were obtained from the Korea Centers for Disease Control and Prevention. Acinetobacter baumannii (Aci_100087) was selected from the clinical isolate collections of hospitals affiliated with the Catholic University of Korea. Each bacterial strain was grown at 37°C on blood agar (Hanil Komed, Co., Seongnam, Korea) and Mueller-Hinton broth (Becton Dickinson, Sparks, MD, USA) was used for antimicrobial susceptibility testing and the animal infection model. The minimum inhibitory concentrations (MICs) of ciprofloxacin (CIP), ceftazidime (CAZ), imipenem (IPM), colistin (CST), ampicillin (AMP), amoxicillin-clavulanic acid (AMC), gentamicin (GEN), and trimethoprim-sulfamethoxazole (TMP/SMX) for the four isolates were determined by the broth microdilution method, in accordance with the Clinical and Laboratory Standards Institute (2015) recommendations [13]. All antimicrobials were obtained from Sigma-Aldrich Korea (Seoul, Korea). All carbapenem resistant Gram-negative bacteria were screened for the presence of blaNDM-1, blaVIM, blaAmpC, and blaKPC by polymerase chain reaction (PCR) and blaOXA by multiplex PCR using previously described primers. The primer sequences of the genes used in this study were described previously by Kim et al. [14].
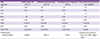
The MIC ranges of four carbapenem-resistant Gram-negative strains are presented in Table 1 with the genetic characteristics of antimicrobial resistance of the bacterial strains. E. coli, K. pneumoniae, and P. aeruginosa carried blaNDM-1, blaKPC, and blaVIM, respectively. Two distinct blaOXA-like genes, blaOXA-23-like and blaOXA-51-like, as well as blaAmpC were identified for A. baumannii by multiplex PCR [14].
Six-week-old specific-pathogen-free, female ICR/Swiss and BALB/c mice weighing 23–27 g (Orient Bio, Sungnam, Korea) were used in this study. All animal experiments and animal care were carried out in accordance with the criteria of the Laboratory Animals Welfare Act, the Guide for the Care and Use of Laboratory Animals, and the Guidelines and Policies for Rodent Survival Surgery provided by the Institutional Animal Care and Use Committee (IACUC) of the College of Medicine, The Catholic University of Korea (approval no. CUMC-2015-0002-04). This study was also exempted from judges of Institutional Review Board, Seoul St. Mary's Hospital as we used stock strains (KC15SISI0111). Mice were housed in rooms with controlled temperature (18–25°C) and humidity (40–70%). Broth cultures of freshly plated bacteria were grown to logarithmic phase overnight to an absorbance at 600 nm of 0.04–0.05 (SpectraMAX190; Molecular Devices, Sunnyvale, CA, USA), corresponding to 1 × 108 CFU/mL. Hog gastric mucin (Sigma-Aldrich, St. Louis, MO, USA) was used as a virulence-enhancing factor for bacteria. Bacterial cells were adjusted to 108 CFU/mL with phosphate-buffered saline. The challenge dose, 107 CFU, was prepared by mixing an equal volume of 6% hog mucin (dissolved in phosphate-buffered saline) with an equal volume of the bacterial suspension immediately before experiments. Infections by each of the isolates and inocula were produced by intraperitoneal injection of 0.2 mL of each inoculum into isoflurane-anesthetized (JW Pharmaceutical, Hwasung, Korea) mice. Mice were observed until they were fully recovered from anesthesia and showed no signs of sudden death from mistakenly placed injections into a site other than the peritoneal cavity for 10 min. Each experimental group consisted of three mice, and the tests were repeated twice for each condition to confirm reproducibility. The survival rates of mice were monitored for up to 24 h at 0, 12, and 24 h after the intraperitoneal bacterial injection. Mice that survived the experiments were sacrificed by CO2 asphyxiation after completion of experiments.
We compared the lethality of each murine model at 24 h; 1) peritonitis model without hog gastric mucin vs. with hog gastric mucin, regardless of mice species 2) peritonitis model using ICR mice vs. BALB/c mice, 3) peritonitis model with mucin using ICR mice vs. BALB/c. The categorical variables were compared using the Fisher's exact test or Chi-square analysis. All statistical analyses were done using SPSS software version 24.0 (SPSS Korea, Seoul, Korea). A P value of ≤0.05 was considered statistically significant.
Comparison of survival rates of several murine peritonitis model by each carbapenem-resistant Gram-negative strains were shown in Figure 1. E. coli (EC-1) with 3% hog gastric mucin failed to infect ICR mice but completely killed BALB/c mice at 24 h after injection. For K. pneumoniae (KP-4) and P. aeruginosa (PA-3) infections, both ICR (45% vs 100% in K. pneumoniae [P = 0.036], 45% vs 100% in P. aeruginosa [P = 0.036]) and BALB/c (17% vs 100% in K. pneumoniae [P = 0.001], 34% vs 100% in P. aeruginosa [P = 0.009]) mice treated with mucin showed significantly higher mortality. For A. baumannii (Aci_100087), both ICR (11% vs 100%, P = 0.015) and BALB/c (34% vs 100%, P = 0.009) mice treated with mucin exhibited higher lethality than those without mucin treatment. Although ICR mice exhibited higher mortality than BALB/c mice, there were no significant differences in lethality in both mouse strains.
Taken together, these findings demonstrated that the use of 3% hog gastric mucin could increase infection rates in mice. However, there were no significant differences in fatalities between ICR and BALB/c mice infected with any of the bacterial strains, with the exception of E. coli (EC-1, P <0.001).
In this study, we infected ICR mice since this strain is known to have good reproductive performance and has been used extensively in animal experiments. BALB/c mice, which are frequently used for a variety of immunological studies, including vaccine development, and in studies of infectious diseases [15], were also evaluated. Based on the result of our previous research, in which injection of 105 CFU virulent pneumococcus without mucin completely killed both ICR and BALB/c mice, we established our first experimental conditions that did not use hog gastric mucin. However, we failed to induce infection with clinical isolates of carbapenem-resistant Gram-negative E. coli (EC-1), K. pneumoniae (KP-4), P. aeruginosa (PA-3), and A. baumannii (Aci_100087) in both mouse strains. Several reports have described the use of hog gastric mucin as a virulence-enhancing factor. Mucin is the macromolecular component of mammalian mucus, and hog gastric mucin is purified from the hog gastric mucosa of healthy pigs. In 1932, researchers found that the pathogenicity of bacteria was increased by admixture with hog gastric mucin, whereas mucin alone did not cause death in mice if injected into the peritoneal cavity [16]. Although the exact pathophysiological mechanism through which mucin increases bacterial virulence is still uncertain, after numerous hypotheses and observations, researchers have concluded that intraperitoneal infection with mucin can be attributed to its coating effect on bacteria. Keefer et al. showed that administration of mucin profoundly lowered the levels of the normal serum bactericidin, properdin, resulting in enhanced virulence of the bacteria [17]. In another study mucin was employed to replenish nutrition for Enterococci just before infecting mice [18]. To determine the bacterial inoculum in this study, we referred to a journal of Fattom et al. [19], whose group also used mucin to induce peritonitis. According to their method, we infected ICR and BALB/c with 105-107 CFU of carbapenem-resistant Gram-negative bacteria using mucin.As a result, mice showed lethal effect with inoculum 10
7 CFU. Given this information, we designed our intraperitoneal infection model with inoculum 107 CFU plus 3% hog gastric mucin for the second trial. Finally, our research results demonstrated that carbapenem-resistant K. pneumoniae (KP-4), P. aeruginosa (PA-3), and A. baumannii (Aci_100087) could successfully infect both ICR and BALB/c mice when mucin was added. The differences in lethality between ICR and BALB/c for the three bacterial strains were statistically insignificant. However, the carbapenem-resistant E. coli (EC-1) could infect only BALB/c mice even with mucin treatment, showing statistically significant difference between ICR and BABL/c mice. It is unclear whether there is a significant relation between murine species and bacterial pathogens, which needs to be further studied in the future. Hence, when testing carbapenem-resistant strains including E. coli, intraperitoneal injection of the bacterial strains with 3% hog gastric mucin to BALB/c mice would be suitable. Furthermore, the animal model developed in this study could be widely and easily applied to investigate the pathophysiology of carbapenem-resistant Gram-negative bacteria detected in Korea and to determine the usefulness of testing when aiming to cure infectious diseases caused by these bacterial strains.
Figures and Tables
Figure 1
Carbapenem-resistant Escherichia coli (EC-1), Klebsiella pneumoniae (KP-4), Pseudomonas aeruginosa (PA-3) and Acinetobacter baumannii (Aci_100087) with or without 3% hog gastric mucin. Results show that animals inoculated with strains without mucin treatment failed in infection for both mice species, whereas with mucin, infection was successfully induced 24 h after the experiment except for E. coli infection of ICR mice. 3% hog gastric mucin dissolved in phosphate-buffered saline was used as a negative control for each experimental group.
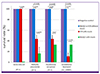
Table 1
MICs and genetic characteristics of carbapenem-resistant Gram-negative strains used in this study.
Acknowledgements
This research was supported by a grant from the Korea Health Technology R&D Project (grant number: HI14C2658) through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea.
References
1. World health organization (WHO). Global action plan on antimicrobial resistance. Accessed 14 October 2016. Available at: http://www.who.int/antimicrobial-resistance/global-action-plan/en/.
2. Lee CS, Doi Y. Therapy of infections due to carbapenem-resistant Gram-negative pathogens. Infect Chemother. 2014; 46:149–164.

3. van Duin D, Kaye KS, Neuner EA, Bonomo RA. Carbapenem-resistant Enterobacteriaceae: a review of treatment and outcomes. Diagn Microbiol Infect Dis. 2013; 75:115–120.

4. Lee HJ, Choi JK, Cho SY, Kim SH, Park SH, Choi SM, Lee DG, Choi JH, Yoo JH. Carbapenem-resistant Enterobacteriaceae: prevalence and risk factors in a single community-based hospital in Korea. Infect Chemother. 2016; 48:166–173.

5. Pan CY, Chen JC, Chen TL, Wu JL, Hui CF, Chen JY. Piscidin is highly active against carbapenem-resistant Acinetobacter baumannii and NDM-1-producing Klebsiella pneumoniae in a systemic septicaemia infection mouse model. Mar Drugs. 2015; 13:2287–2305.

6. Cao F, Wang X, Wang L, Li Z, Che J, Wang L, Li X, Cao Z, Zhang J, Jin L, Xu Y. Evaluation of the efficacy of a bacteriophage in the treatment of pneumonia induced by multidrug resistance Klebsiella pneumoniae in mice. Biomed Res Int. 2015; 2015:752930.
7. Aoki N, Tateba K, Kikuchi Y, Kimura S, Miyazaki C, Ishii Y, Tanabe Y, Gejyo F, Yamaguchi K. Efficacy of colistin combination therapy in a mouse model of pneumonia caused by multidrug-resistant Pseudomonas aeruginosa
. J Antimicrob Chemother. 2009; 63:534–542.

8. Pan CY, Chen JC, Sheen JF, Lin TL, Chen JY. Epinecidin-1 has immunomodulatory effects, facilitating its therapeutic use in a mouse model of Pseudomonas aeruginosa sepsis. Antimicrob Agents Chemother. 2014; 58:4264–4274.

9. Harris G, Kuo Lee R, Lam CK, Kanzaki G, Patel GB, Xu HH, Chen W. A mouse model of Acinetobacter baumannii–associated pneumonia using a clinically isolated hypervirulent strain. Antimicrob Agents Chemother. 2013; 57:3601–3613.

10. Rosen DA, Hilliard JK, Tiemann KM, Todd EM, Morley SC, Hunstad DA.
Klebsiella pneumoniae FimK promotes virulence in murine pneumonia. J Infect Dis. 2016; 213:649–658.
11. He S, He H, Chen Y, Wang W, Yu D.
In vitro and in vivo analysis of antimicrobial agents alone and in combination against multi-drug resistant Acinetobacter baumannii
. Front Microbiol. 2015; 6:507.
12. Luo G, Spellberg B, Gebremariam T, Bolaris M, Lee H, Fu Y, French SW, Ibrahim AS. Diabetic murine models for Acinetobacter baumannii infection. J Antimicrob Chemother. 2012; 67:1439–1445.
13. Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial susceptibility testing: Twenty-fifth informational supplement M100-S25. Wayne, PA: CLSI;2015.
14. Kim SH, Park C, Chun HS, Lee DG, Choi JK, Lee HJ, Cho SY, Park SH, Choi SM, Choi JH, Yoo JH. Pilot screening to determine antimicrobial synergies in a multidrug-resistant bacterial strain library. Microb Drug Resist. 2016; 22:372–378.

15. Division of laboratory animal resources (DLAR). Commonoly used mouse strains. Accessed 26 August 2016. Available at: https://www.research.uky.edu/dlar/documents/CommonMouseResearchModels.pdf.
17. Dewitt CW. Differential effect of hog gastric mucin on properdin and host resistance to infection. J Bacteriol. 1958; 76:631–639.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download