Abstract
Background
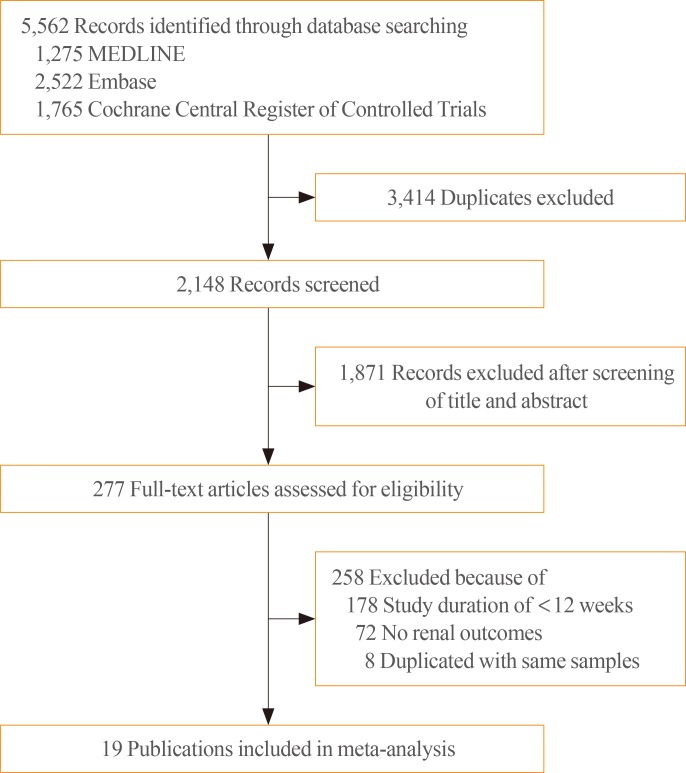
Methods
Results
ACKNOWLEDGMENTS
Notes
AUTHOR CONTRIBUTIONS:
Conception or design: J.H.B., S.K., E.G.P., S.G.K., S.H., N.H.K.
Acquisition, analysis, or interpretation of data: J.H.B., S.K., E.G.P., S.H., N.H.K.
Drafting the work or revising: J.H.B., S.K., S.H., N.H.K.
Final approval of the manuscript: J.H.B., S.K., E.G.P., S.G.K., S.H., N.H.K.
Obtained funding, statistical analysis: S.K., S.H., N.H.K.
Appendix
Appendix 1. Study protocol
-
1) Study characteristics
(1) Population: patients with T2D
(2) Intervention: DPP-4 inhibitors
(3) Comparison: placebo or other antidiabetic agents
-
(4) Outcomes of interests
① Changes in urine albumin-to-creatinine ratio (UACR) from baseline
② Changes in estimated glomerular filtration rate (eGFR) from baseline
③ Development of microalbuminuria
④ Development of macroalbuminuria
⑤ Regression of albuminuria, defined as the development of normoalbuminuria from microalbuminuria or macroalbuminuria; development of microalbuminuria from macroalbuminuria
⑥ Development of end-stage renal disease (ESRD), defined as initiation of renal replacement therapy, renal transplantation, serum creatinine levels >6.0 mg/dL, or renal failure
(5) Study design: randomized controlled trials (RCTs)
(6) Length of follow-up: at least 12 weeks of study duration
-
2) Report characteristics
-
3) Inclusion and exclusion criteria
(1) The study population was men and women with T2D.
(2) We only included RCTs comparing efficacy or safety of DPP-4 inhibitors with those of placebo or other antidiabetic agents in patients with T2D.
(3) Any concurrent use of antidiabetic agents other than glucagon-like peptide-1 receptor agonists was allowed.
(4) Only RCTs with a study duration of 12 weeks or more were included.
(5) We only included RCTs reporting at least one renal outcome including UACR, eGFR, microalbuminuria, macroalbuminuria, doubling of serum creatinine levels, renal failure, ESRD, renal replacement therapy, dialysis, and kidney transplantation.
(6) In case of duplicates or extensions, we only included a study with the longer duration or more information about renal outcomes.
(7) Pooled analysis or secondary analysis was included only when it provided more information about renal outcomes than original publications.
(8) There is no restriction of language.
(9) We included full-text articles with no restriction of publication status.
1) MEDLINE: DPP-4 inhibitor OR DPP4 inhibitor OR alogliptin OR anagliptin OR evogliptin OR gemigliptin OR linagliptin OR omarigliptin OR saxagliptin OR sitagliptin OR teneligliptin OR trelagliptin OR vildagliptin
2) Embase: DPP-4 inhibitor OR DPP4 inhibitor OR alogliptin OR anagliptin OR evogliptin OR gemigliptin OR linagliptin OR omarigliptin OR saxagliptin OR sitagliptin OR teneligliptin OR trelagliptin OR vildagliptin
3) The Cochrane Central Register of Controlled Trials: DPP-4 inhibitor OR DPP4 inhibitor OR alogliptin OR anagliptin OR evogliptin OR gemigliptin OR linagliptin OR omarigliptin OR saxagliptin OR sitagliptin OR teneligliptin OR trelagliptin OR vildagliptin
1) First author
2) Publication year
3) Number of randomized participants
4) Mean age of randomized participants, years
5) Study duration, weeks
6) Intervention including names and doses of DPP-4 inhibitors
7) Comparison including placebo or names and doses of other antidiabetic agents
8) Background antidiabetic agents
9) Baseline eGFR, mL/min/1.73 m2
10) Mean changes in UACR with their standard deviation, mg/g
11) Mean changes in eGFR with their standard deviation, mL/min/1.73 m2
12) Number of participants reporting the development of microalbuminuria
13) Number of participants reporting the development of macroalbuminuria
14) Number of participants reporting regression of albuminuria
15) Number of participants reporting the development of ESRD
1) Statistical analysis: We calculated standard mean differences for UACR, weighted mean differences (WMDs) for eGFR with 95% confidence intervals (CIs), and calculate relative risks (RRs) with 95% CI for dichotomous variables. In meta-analysis, we used a random-effects model to evaluate WMDs, RRs, and their 95% CIs.
2) Subgroup analysis: We performed a subgroup analysis for evaluating changes in UACR according to sodium-glucose cotransporter 2 (SGLT2) inhibitors versus non-SGLT2 inhibitors in the control group.
3) Identifying and measuring statistical heterogeneity: We used Cochran's Q test for testing statistical heterogeneity and the I2 statistic for measuring the degree of heterogeneity.
References
SUPPLEMENTARY MATERIALS
Supplemental Fig. S2
Supplemental Fig. S3
Fig. 2
Standardized mean differences in changes in urine albumin-to-creatinine ratio (UACR) from baseline (mg/g) for dipeptidyl peptidase-4 (DPP-4) inhibitors versus placebo or other antidiabetic agents, according to non-sodium-glucose cotransporter 2 inhibitors and sodium-glucose cotransporter 2 inhibitors in the control group. Trt, treatment group; Con, control group; SD, standard deviation; ES, effect size; CI, confidence interval; SGLT2, sodium-glucose cotransporter 2; OHA, oral hypoglycemic agent; NR, not reported.
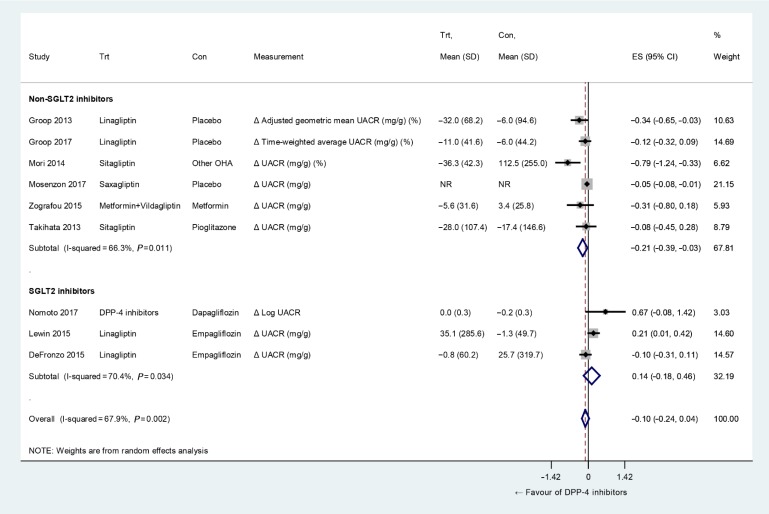
Fig. 3
Weighted mean differences in changes in estimated glomerular filtration rate from baseline (mL/min/1.73 m2) for dipeptidyl peptidase-4 (DPP-4) inhibitors versus placebo or other antidiabetic agents. Trt, treatment group; Con, control group; SD, standard deviation; ES, effect size; CI, confidence interval; NR, not reported.
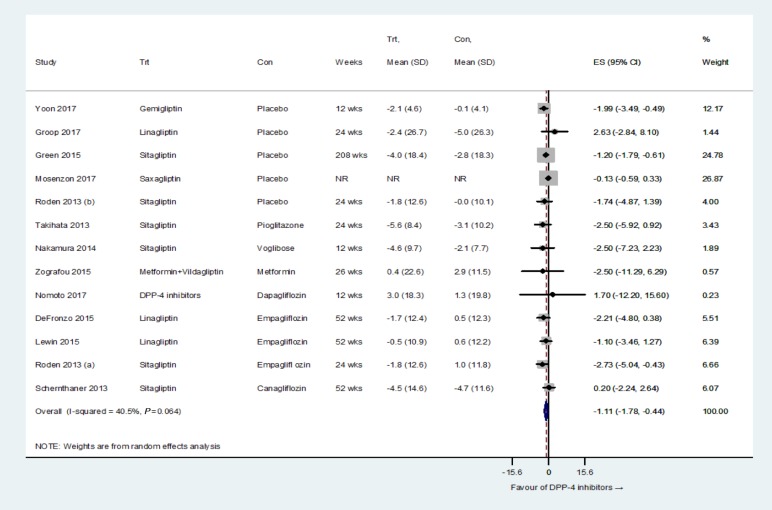
Fig. 4
Relative risks of incident albuminuria, regression of albuminuria, and end-stage renal disease for dipeptidyl peptidase-4 (DPP-4) inhibitors versus placebo or other antidiabetic agents. (A) Microalbuminuria, (B) macroalbuminuria, (C) regression of albuminuria, and (D) end-stage renal disease. Trt, treatment group; Con, control group; RR, relative risk; CI, confidence interval.
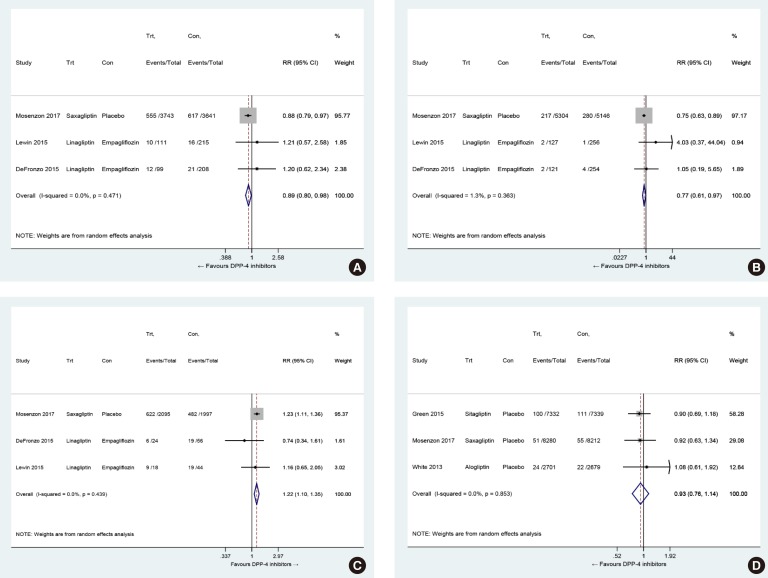
Table 1
Characteristics of Included Studies in the Systematic Review and Meta-Analysis
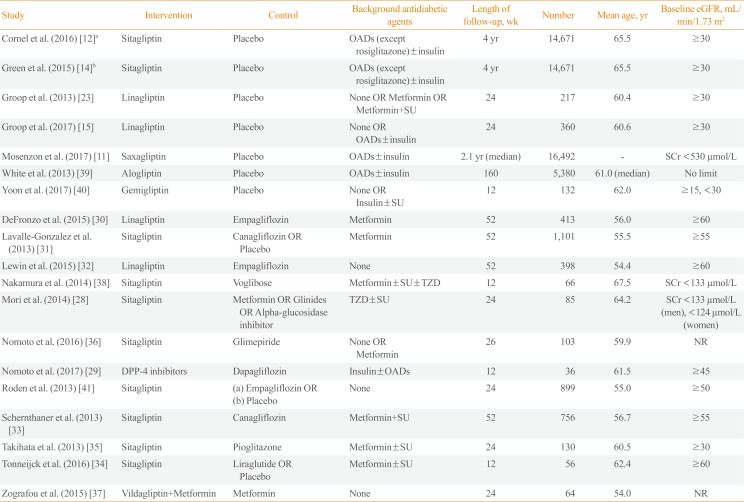
| Study | Intervention | Control | Background antidiabetic agents | Length of follow-up, wk | Number | Mean age, yr | Baseline eGFR, mL/min/1.73 m2 |
|---|---|---|---|---|---|---|---|
| Cornel et al. (2016) [12]a | Sitagliptin | Placebo | OADs (except rosiglitazone)±insulin | 4 yr | 14,671 | 65.5 | ≥30 |
| Green et al. (2015) [14]b | Sitagliptin | Placebo | OADs (except rosiglitazone)±insulin | 4 yr | 14,671 | 65.5 | ≥30 |
| Groop et al. (2013) [23] | Linagliptin | Placebo | None OR Metformin OR Metformin+SU | 24 | 217 | 60.4 | ≥30 |
| Groop et al. (2017) [15] | Linagliptin | Placebo | None OR OADs±insulin | 24 | 360 | 60.6 | ≥30 |
| Mosenzon et al. (2017) [11] | Saxagliptin | Placebo | OADs±insulin | 2.1 yr (median) | 16,492 | - | SCr <530 µmol/L |
| White et al. (2013) [39] | Alogliptin | Placebo | OADs±insulin | 160 | 5,380 | 61.0 (median) | No limit |
| Yoon et al. (2017) [40] | Gemigliptin | Placebo | None OR Insulin±SU | 12 | 132 | 62.0 | ≥15, <30 |
| DeFronzo et al. (2015) [30] | Linagliptin | Empagliflozin | Metformin | 52 | 413 | 56.0 | ≥60 |
| Lavalle-Gonzalez et al. (2013) [31] | Sitagliptin | Canagliflozin OR Placebo | Metformin | 52 | 1,101 | 55.5 | ≥55 |
| Lewin et al. (2015) [32] | Linagliptin | Empagliflozin | None | 52 | 398 | 54.4 | ≥60 |
| Nakamura et al. (2014) [38] | Sitagliptin | Voglibose | Metformin±SU±TZD | 12 | 66 | 67.5 | SCr <133 µmol/L |
| Mori et al. (2014) [28] | Sitagliptin | Metformin OR Glinides OR Alpha-glucosidase inhibitor | TZD±SU | 24 | 85 | 64.2 | SCr <133 µmol/L (men), <124 µmol/L (women) |
| Nomoto et al. (2016) [36] | Sitagliptin | Glimepiride | None OR Metformin | 26 | 103 | 59.9 | NR |
| Nomoto et al. (2017) [29] | DPP-4 inhibitors | Dapagliflozin | Insulin±OADs | 12 | 36 | 61.5 | ≥45 |
| Roden et al. (2013) [41] | Sitagliptin |
(a) Empagliflozin OR (b) Placebo |
None | 24 | 899 | 55.0 | ≥50 |
| Schernthaner et al. (2013) [33] | Sitagliptin | Canagliflozin | Metformin+SU | 52 | 756 | 56.7 | ≥55 |
| Takihata et al. (2013) [35] | Sitagliptin | Pioglitazone | Metformin±SU | 24 | 130 | 60.5 | ≥30 |
| Tonneijck et al. (2016) [34] | Sitagliptin | Liraglutide OR Placebo | Metformin±SU | 12 | 56 | 62.4 | ≥60 |
| Zografou et al. (2015) [37] | Vildagliptin+Metformin | Metformin | None | 24 | 64 | 54.0 | NR |




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download