1. Poulter NR, Prabhakaran D, Caulfield M. Hypertension. Lancet. 2015; 386:801–812. PMID:
25832858.

2. Esteghamati A, Meysamie A, Khalilzadeh O, Rashidi A, Haghazali M, Asgari F, et al. Third national Surveillance of Risk Factors of Non-Communicable Diseases (SuRFNCD-2007) in Iran: methods and results on prevalence of diabetes, hypertension, obesity, central obesity, and dyslipidemia. BMC Public Health. 2009; 9:167. PMID:
19480675.

3. Gillum RF, Mussolino ME, Madans JH. Body fat distribution and hypertension incidence in women and men. The NHANES I Epidemiologic Follow-up Study. Int J Obes Relat Metab Disord. 1998; 22:127–134. PMID:
9504320.

4. Harris MM, Stevens J, Thomas N, Schreiner P, Folsom AR. Associations of fat distribution and obesity with hypertension in a bi-ethnic population: the ARIC study. Atherosclerosis Risk in Communities Study. Obes Res. 2000; 8:516–524. PMID:
11068957.
5. Folsom AR, Prineas RJ, Kaye SA, Munger RG. Incidence of hypertension and stroke in relation to body fat distribution and other risk factors in older women. Stroke. 1990; 21:701–706. PMID:
2339449.

6. Cassano PA, Segal MR, Vokonas PS, Weiss ST. Body fat distribution, blood pressure, and hypertension. A prospective cohort study of men in the normative aging study. Ann Epidemiol. 1990; 1:33–48. PMID:
1669488.
7. Troisi RJ, Weiss ST, Segal MR, Cassano PA, Vokonas PS, Landsberg L. The relationship of body fat distribution to blood pressure in normotensive men: the normative aging study. Int J Obes. 1990; 14:515–525. PMID:
2401588.
8. Amato MC, Giordano C, Galia M, Criscimanna A, Vitabile S, Midiri M, et al. Visceral adiposity index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010; 33:920–922. PMID:
20067971.
9. Lemieux I, Poirier P, Bergeron J, Almeras N, Lamarche B, Cantin B, et al. Hypertriglyceridemic waist: a useful screening phenotype in preventive cardiology? Can J Cardiol. 2007; 23(Suppl B):23B–31B.

10. Elisha B, Messier V, Karelis A, Coderre L, Bernard S, Prud'homme D, et al. The visceral adiposity index: relationship with cardiometabolic risk factors in obese and overweight postmenopausal women: a MONET group study. Appl Physiol Nutr Metab. 2013; 38:892–899. PMID:
23855278.
11. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity is an independent predictor of incident hypertension in Japanese Americans. Ann Intern Med. 2004; 140:992–1000. PMID:
15197016.

12. Hayashi T, Boyko EJ, Leonetti DL, McNeely MJ, Newell-Morris L, Kahn SE, et al. Visceral adiposity and the prevalence of hypertension in Japanese Americans. Circulation. 2003; 108:1718–1723. PMID:
12975250.

13. Fox CS, Massaro JM, Hoffmann U, Pou KM, Maurovich-Horvat P, Liu CY, et al. Abdominal visceral and subcutaneous adipose tissue compartments: association with metabolic risk factors in the Framingham Heart Study. Circulation. 2007; 116:39–48. PMID:
17576866.
14. Foy CG, Hsu FC, Haffner SM, Norris JM, Rotter JI, Henkin LF, et al. Visceral fat and prevalence of hypertension among African Americans and Hispanic Americans: findings from the IRAS family study. Am J Hypertens. 2008; 21:910–916. PMID:
18566594.

15. Oka R, Miura K, Sakurai M, Nakamura K, Yagi K, Miyamoto S, et al. Impacts of visceral adipose tissue and subcutaneous adipose tissue on metabolic risk factors in middle-aged Japanese. Obesity (Silver Spring). 2010; 18:153–160. PMID:
19498348.

16. Koh H, Hayashi T, Sato KK, Harita N, Maeda I, Nishizawa Y, et al. Visceral adiposity, not abdominal subcutaneous fat area, is associated with high blood pressure in Japanese men: the Ohtori study. Hypertens Res. 2011; 34:565–572. PMID:
21228782.

17. Boyko EJ, Leonetti DL, Bergstrom RW, Newell-Morris L, Fujimoto WY. Visceral adiposity, fasting plasma insulin, and blood pressure in Japanese-Americans. Diabetes Care. 1995; 18:174–181. PMID:
7729294.

18. Kanai H, Matsuzawa Y, Kotani K, Keno Y, Kobatake T, Nagai Y, et al. Close correlation of intra-abdominal fat accumulation to hypertension in obese women. Hypertension. 1990; 16:484–490. PMID:
2228147.

19. Johnson D, Prud'homme D, Despres JP, Nadeau A, Tremblay A, Bouchard C. Relation of abdominal obesity to hyperinsulinemia and high blood pressure in men. Int J Obes Relat Metab Disord. 1992; 16:881–890. PMID:
1337343.
20. Amini M, Janghorbani M. Diabetes and impaired glucose regulation in first-degree relatives of patients with type 2 diabetes in isfahan, iran: prevalence and risk factors. Rev Diabet Stud. 2007; 4:169–176. PMID:
18084674.

21. Executive summary: standards of medical care in diabetes 2013. Diabetes Care. 2013; 36(Suppl 1):S4–S10. PMID:
23264424.
22. Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Report of the expert committee on the diagnosis and classification of diabetes mellitus. Diabetes Care. 2003; 26(Suppl 1):S5–S20. PMID:
12502614.
23. James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507–520. PMID:
24352797.
24. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972; 18:499–502. PMID:
4337382.

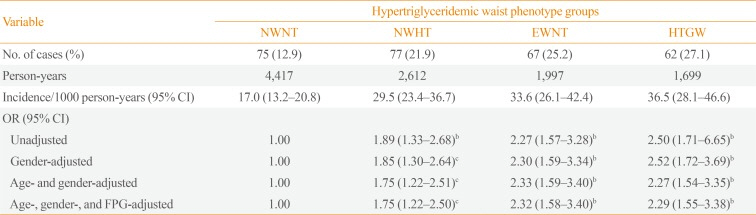
25. Janghorbani M, Amini M. Utility of hypertriglyceridemic waist phenotype for predicting incident type 2 diabetes: the Isfahan Diabetes Prevention Study. J Diabetes Investig. 2016; 7:860–866.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download