This article has been
cited by other articles in ScienceCentral.
Abstract
Objective
Because villoglandular adenocarcinoma (VGA) of the uterine cervix has favorable features and outcomes, patients receive less radical surgery and young women preserve their ovaries. We aimed to evaluate the clinicopathological features and outcomes of VGA and to see if the ovarian preservation is safe in young women with VGA.
Methods
We retrospectively reviewed medical records and identified patients with VGA, who had been treated and followed from January 2004 to December 2015.
Results
This study consisted of 17 patients with VGA, including 9 premenopausal women. International Federation of Gynecology and Obstetrics (FIGO) stage IB1 disease was found in 12 patients (70.6%), IA1 in 2, IA2 in 1, IB2 in 1, and IIA1 in 1. Of the 12 women diagnosed with stage IB1 disease, a young woman received only conization and she has not showed a recurrence. During a median follow-up of 58 months (range: 12–116), 4 patients, who had undergone radical surgery for stage IB1 disease, had a recurrence and one of them died due to disease progression. Among patients with stages IB–IIA disease, 2 premenopausal women did not receive simultaneous oophorectomy or chemoradiation therapy. Both of them had a recurrent tumor at adnexa.
Conclusion
This study revealed favorable features and outcomes of VGA. However, the appropriate treatment for young women with early-stage VGA must be cautiously selected. Ovarian preservation might not be safe when young women with stages IB–IIA VGA undergo surgical procedures.
Keywords: Adenocarcinoma, Papillary, Uterine Cervical Neoplasms, Therapy, Fertility Preservation, Treatment Outcome
INTRODUCTION
The incidence of adenocarcinoma of the uterine cervix has increased over the last several decades whereas that of squamous cell carcinoma (SCC) has decreased [
12]. Compared to women with SCC, patients with adenocarcinoma tend to be younger and manifest different responses to treatment [
234]. Additionally, compared to SCC, adenocarcinoma is known to be commonly associated with lymph node (LN) involvement and distant metastasis and have poorer prognosis [
456]. Villoglandular adenocarcinoma (VGA), as rare subtype of well-differentiated adenocarcinoma, is generally detected in younger women and it has better prognosis than the usual adenocarcinoma [
789101112]. VGA is known to show a superficial invasion, rare lymphovascular space invasion (LVSI), and few LN involvements [
789101112].
Standard surgical procedures for patients with stages IA2–IIA1 cervical cancer consist of radical hysterectomy (RH) and pelvic LN dissection (PLND), occasionally accompanied by bilateral salpingo-oophorectomy (BSO) [
56]. However, early-stage cervical cancer, particularly in the absence of high-risk pathological factors, has a favorable prognosis with 5-year survival rates reaching approximately 90% [
56]. Therefore, much attention has been devoted to the preservation of normal tissues and physiological functions [
13]. Furthermore, fertility-sparing surgeries including conization and trachelectomy have been proposed as alternatives for young women desiring childbearing [
14]. Especially, the favorable features of VGA have led many oncologists to conduct conservative treatments such as conization or trachelectomy.
Ovarian preservation improves quality of life. However, the safety of ovarian preservation in young women with early-stage cervical cancer remains unclear. Although risk factors for ovarian metastasis are not well established, the histological types have been associated with ovarian metastasis [
1516]. Oophorectomy eliminates the possibility of ovarian metastasis. However, it can trigger a surgical menopause in young women. A study demonstrated that while ovaries could be preserved in young patients with stages IB–IIA SCC, ovaries should be removed from all patients with adenocarcinoma [
16]. On the other hand, a few authors concluded that ovarian preservation is oncologically safe for young women with stage I adenocarcinoma because it is not associated with increased risk of cancer-specific or overall mortality [
17].
Ovarian preservation in young women with early-stage VGA has not yet to be reported. Because VGA is a rare tumor, there are limitations in evaluating the natural history of VGA and selecting optimal management options. Therefore, we aimed to examine the clinicopathological features and outcomes of VGA and to see if the ovarian preservation is safe in young women with VGA.
MATERIALS AND METHODS
We retrospectively reviewed medical records of 1,952 patients who were diagnosed with cervical cancer from January 2004 to December 2015 at Chonnam National University Hospital, Gwangju, Korea. We excluded 1,558 patients with SCC and 55 patients with other types of cervical cancer except adenocarcinoma. Among 339 patients with adenocarcinoma, 17 patients with VGA were identified. The design of this study was approved by the Institutional Review Board (IRB) of Chonnam National University (approval No. 2015-049).
All patients underwent cervical cytology of Thin-Prep and human papillomavirus (HPV) DNA Chip test at the initial visit. We performed pelvic examination and, if needed, colposcopy. We carried out punch biopsy of cancerous lesion of the cervix or conducted conization when tumor was uncertain. After VGA was histologically confirmed, all patients underwent pelvic magnetic resonance imaging (MRI) and positron emission tomography-computed tomography (PET-CT) for preoperative evaluation of invasion to adjacent organs or distant metastasis. After thorough consultation with patients about the results, we decided the appropriate treatment option which was acceptable for each patient.
Clinical characteristics of patients included age, menopausal status, initial symptoms, results of cervical cytology, HPV infections, and stage according to International Federation of Gynecology and Obstetrics (FIGO). Pathological findings of tumor included macroscopic features, tumor size, histological grade, depth of cervical stromal invasion, resection margin, LVSI, and LN involvement status. Data pertaining to treatments and outcomes included primary treatments, adjuvant therapies, follow-up period, recurrence of disease, and survival. Histological diagnosis was based on analysis of biopsies or hysterectomy specimens. Tumor size was calculated according to the clinical stage. The resection margin was considered negative when the margin was greater than 10 mm from carcinoma in cases of hysterectomy and when the safety of 3 mm or more was secured in conization. Histology and cytology slides were finally confirmed by a single gynecologic pathologist of our institution. LN status before initial treatment was determined by pelvic MRI and PET-CT. Concurrent chemoradiation therapy (CCRT) was combined with cisplatin. HPV DNA chip test, a polymerase chain reaction (PCR)-based HPV DNA microarray system, is a HPV genotyping method for 15 high-risk HPV types (HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 53, 56, 58, 59, 66, and 68) and 9 low-risk HPV types (HPV types 6, 11, 34, 40, 42, 43, 44, 57, and 70).
Descriptive statistics were calculated for age and follow-up period. Overall survival (OS) time was calculated as the number of months from the date of initial treatment until the date of death. Disease-free survival (DFS) time was calculated as the number of months from the date of initial treatment to the date of recurrence. Follow-up was updated in January 2017. All data were analyzed using Statistical Package Service Solution (SPSS) software for Windows version 23.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
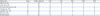
Clinicopathological characteristics of patients are listed in
Table 1. The median age was 50 years (range, 28 to 68 years) and 9 patients (52.9%) were premenopausal. Results of cervical cytology revealed adenocarcinoma in 14 patients and atypical glandular cells in 3. Sixteen women (94.1%) were infected with HPV. Stage IB1 disease (70.6%) was most common. Thirteen patients underwent different types of surgical procedures and one of them received postoperative CCRT due to pelvic LN metastasis (LNM). Three patients received primary CCRT without any surgery. A woman with stage IB1 disease was not treated surgically because of poor medical status. The remaining 2 patients received primary CCRT due to stage IIA1 or IB2 disease. A young woman with stage IB1 disease was conservatively treated with only conization. Pelvic LNM was suspected in 2 patients based on preoperative imaging. One of the patients, the only woman with LVSI, had histological LNM after PLND. Another one received primary CCRT without histological confirmation.
Table 1
Clinicopathologic characteristics of patients with VGA of the uterine cervix

|
Clinical characteristics |
No. (%) |
|
Age (yr) |
50 (28–68) |
|
≥50 |
9 (52.9) |
|
≥40 and <50 |
6 (35.3) |
|
≥30 and <40 |
1 (5.9) |
|
<30 |
1 (5.9) |
|
Menopause |
|
|
Pre-menopause |
9 (52.9) |
|
Post-menopause |
8 (47.1) |
|
Presenting symptom |
|
|
Vaginal bleeding |
6 (35.3) |
|
Leukorrhea |
3 (17.6) |
|
Asymptomatic |
8 (47.1) |
|
Cervical cytology (Thin-Prep test) |
|
|
Adenocarinoma |
14 (82.4) |
|
Atypical glandular cell |
3 (17.6) |
|
HPV type |
|
|
16 |
6 (35.3) |
|
18 |
9 (52.9) |
|
18, 31 |
1 (5.9) |
|
Negative |
1 (5.9) |
|
FIGO stage |
|
|
IIA1 |
1 (5.9) |
|
IB2 |
1 (5.9) |
|
IB1 |
12 (70.6) |
|
IA2 |
1 (5.9) |
|
IA1 |
2 (11.7) |
|
LN status by imaging before primary treatment*
|
|
|
Involved |
2 (11.7) |
|
Not involved |
15 (88.3) |
|
Primary treatment |
|
|
Surgery |
13 (76.5) |
|
CCRT |
3 (17.6) |
|
Conization |
1 (5.9) |
|
LVSI |
|
|
Positive |
1 (5.9) |
|
Negative |
13 (76.5) |
|
Unknown |
3 (17.6) |
|
LN status by histology after PLND |
|
|
Involved |
1 (5.9) |
|
Not involved |
7 (41.2) |
|
Unknown (not PLND) |
9 (52.9) |
|
Follow-up (mo) |
58 (12–116) |
|
Recurrence |
4 (23.5) |
|
Non-recurrence |
13 (76.5) |
The median follow-up period was 58 months (range, 12 to 116 months). At the time of review, 13 women (76.5%) were alive without recurrence and, 4 patients (23.5%) showed a relapse. Three of them were alive after receiving appropriate treatments, however, one died due to disease progression. Consequentially, the 2-year and 5-year OS rates were 100.0% and 92.3%, respectively. The 2-year and 5-year DFS rates were 87.4% and 72.6%, respectively. Details are summarized in
Table 2.
Table 2
Details of patients with VGA of the uterine cervix

|
No. |
Age (yr) |
Menopause |
Macroscopic finding |
Size (mm) |
Cervical cytology |
HPV genotype |
FIGO stage |
Primary treatment |
Grade |
DOI |
Resection margin |
LVSI |
LNM |
F/U (mo) |
Outcome (mo)*
|
Secondary treatment |
|
1 |
68 |
Yes |
Ulcerative surface |
20 |
AC |
16 |
IIA1 |
CCRT |
1 |
? |
? |
? |
- |
116 |
NED |
- |
|
2 |
53 |
Yes |
Ulcerative surface |
20 |
AC |
16 |
IB1 |
LRH BSO PLND |
1 |
<1/2 |
Neg. |
- |
- |
108 |
NED |
- |
|
3 |
57 |
Yes |
Exophytic mass |
50 |
AC |
16 |
IB2 |
CCRT |
1 |
? |
? |
? |
+†
|
107 |
NED |
- |
|
4 |
43 |
No |
Exophytic mass |
35 |
AGC |
18 |
IB1 |
RH BSO PLND → CCRT |
1 |
<1/2 |
Neg. |
+ |
+‡
|
90 |
NED |
- |
|
5 |
50 |
No |
Exophytic mass |
30 |
AC |
18 |
IB1 |
MRH BSO PLND |
1 |
<1/2 |
Neg. |
- |
- |
80 |
NED |
- |
|
6 |
55 |
Yes |
Exophytic mass |
30 |
AC |
18 |
IB1 |
RH BSO PLND |
2 |
>1/2 |
Neg. |
- |
- |
67 |
ROD (22) – Vagina stump |
CCRT |
|
7 |
60 |
Yes |
Exophytic mass |
35 |
AC |
16 |
IB1 |
CCRT |
1 |
? |
? |
? |
- |
66 |
NED |
- |
|
8 |
28 |
No |
Ulcerative surface |
30 |
AC |
18, 31 |
IB1 |
Conization |
1 |
<1/2 |
Neg. |
- |
- |
65 |
NED |
- |
|
9 |
54 |
Yes |
Ulcerative surface |
30 |
AC |
18 |
IB1 |
LMRH BSO |
1 |
<1/2 |
Neg. |
- |
- |
58 |
ROD (42) – Liver |
ChemoTx |
|
10 |
46 |
No |
Polypoid mass |
30 |
AC |
18 |
IB1 |
LRH PLND |
1 |
<1/2 |
Neg. |
- |
- |
54 |
ROD (34) – Adnexa |
BSO & ChemoTx |
|
11 |
56 |
Yes |
No mass |
No |
AGC |
18 |
IA1 |
TVH BSO |
1 |
<1/2 |
Neg. |
- |
- |
54 |
NED |
- |
|
12 |
31 |
No |
Exophytic mass |
20 |
AC |
16 |
IB1 |
LMRH |
1 |
<1/2 |
Neg. |
- |
- |
41 |
ROD (12) – Adnexa |
BSO & ChemoTx |
|
DOD (42) |
|
13 |
46 |
No |
No mass |
No |
AGC |
No |
IA1 |
TLH |
1 |
<1/2 |
Neg. |
- |
- |
44 |
NED |
- |
|
14 |
64 |
Yes |
No mass |
No |
AC |
18 |
IA2 |
MRH BSO PLND |
1 |
<1/2 |
Neg. |
- |
- |
37 |
NED |
- |
|
15 |
47 |
No |
Ulcerative surface |
20 |
AC |
18 |
IB1 |
MRH BSO PLND |
1 |
>1/2 |
Neg. |
- |
- |
36 |
NED |
- |
|
16 |
48 |
No |
Exophytic mass |
20 |
AC |
18 |
IB1 |
LRH BSO PLND |
1 |
<1/2 |
Neg. |
- |
- |
18 |
NED |
- |
|
17 |
46 |
No |
Exophytic mass |
10 |
AC |
16 |
IB1 |
LMRH BSO |
1 |
<1/2 |
Neg. |
- |
- |
12 |
NED |
- |
Ten of 12 patients with stage IB1 disease underwent surgical procedures including RH or modified RH with or without BSO. Seven of them received PLND, however, the remaining 3 refused to undergo PLND due to the risk of postoperative lymphatic complications. Patient 4, who was confirmed with left hypogastric LNM after receiving RH and PLND with BSO for stage IB1 disease, received postoperative CCRT. She has been alive without any recurrence. Of the 2 patients treated without surgery, patient 7 was treated by primary CCRT and patient 8 underwent only conization. The disease in patient 8 was characterized by the 30 mm flat lesion without definitive mass, and the patient underwent conization initially for accurate diagnosis. Her cone specimen revealed well-differentiated tumor without LVSI, complete resection with clear margin, and invasion <50% of thickness. Additionally, preoperative images showed no LNM. We suggested further treatments. However, she declined surgery or radiation because she desired to preserve her fertility and was extremely afraid of surgery. She finally decided to follow-up without further treatment. She is alive without recurrence.
Patient 1 with stage IIA1 disease and patient 3 with IB2 received primary CCRT. No recurrence was found in either case. Patient 14 with stage IA2 disease underwent modified RH and PLND with BSO. Two patients with stage IA1 disease underwent total vaginal hysterectomy with BSO (patient 11) or total laparoscopic hysterectomy (patient 13). None of the 3 women with stage IA disease showed recurrence.
Four patients (patients 6, 9, 10, and 12) with recurrence were diagnosed at stage IB1. All of them underwent surgical procedures without adjuvant treatments. Two patients did not simultaneously receive BSO and had recurrent tumor at adnexa later. The remaining 2 patients had recurrent tumor at vaginal stump and liver, respectively. Three patients were cured with appropriate treatments. However, patient 12 died due to disease progression.
Patient 6 underwent RH and PLND with BSO for a 30 mm exophytic tumor. Her disease was diagnosed with grade-2 tumor without LVSI and invasion >1/2 of cervical thickness. Tumor recurred at vaginal stump 22 months later and the patient was treated with radiation combined with cisplatin. She has been alive without second recurrence for 45 months after treatment for recurrence. Patient 9 underwent laparoscopic modified radical hysterectomy (MRH) with BSO for the 30 mm ulcerative mass. Her disease was diagnosed with grade-1 tumor without LVSI and invasion <1/2 of cervical thickness. Recurrent hepatic tumor was seen 42 months later. She received systemic chemotherapy (cisplatin with paclitaxel). No second recurrence was detected during 29 months since treatment for recurrence. Patients 10 and 12 had recurrent tumor at adnexa, 42 and 12 months later after first operation, respectively. Neither patient underwent simultaneous BSO. They were confirmed to have grade-1 tumor without LVSI, invasion <1/2 of cervical thickness, and no LNM. They underwent BSO and received further chemotherapy (cisplatin with paclitaxel). Patient 10 has been alive without second recurrence for 33 months after treatment for recurrence. However, patient 12 had progressive disease and died 30 months later since the first recurrence, despite multiple courses of chemotherapy.
DISCUSSION
VGA of the uterine cervix is a rare subtype of adenocarcinoma. Similar to adenocarcinoma, VGA is generally found in younger women [
789101112]. In this study, 52.9% were premenopausal women, in addition, 20s and 30s women were also found. However, VGA is a distinct histological entity with more favorable prognosis compared to usual adenocarcinoma. VGA has been associated with well-differentiated tumor, superficial invasion, uncommon LVSI, and rare LNM (
Table 3). Like other series, our study also showed favorable features of VGA. These features of VGA might support less radical management approaches, especially for young women. Some authors have postulated that while SCC has lymphatic spread, adenocarcinoma has hematogenous metastasis [
16]. Absence of LNM in preoperative image and LVSI in biopsy may obviate the need for lymphadenectomy, although further study is needed. Sentinel LN biopsy may be an alternative, but this is also to require more research.
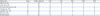
Table 3
Literature review of series published on VGA of the uterine cervix
|
References |
Cases |
Median age (yr) |
LND |
LVSI |
LNM |
ROD |
DOD |
|
Kaku et al. [7] |
7 |
45 |
7 |
2 |
2 |
1 |
1 |
|
Jones et al. [8] |
12 |
38 |
12 |
0 |
? |
2 |
1 |
|
Khunamornpong et al. [9] |
15 |
39 |
15 |
3 |
2 |
0 |
0 |
|
Utsugi et al. [10] |
13 |
45 |
13 |
4 |
1 |
0 |
0 |
|
Lataifeh et al. [11] |
28 |
38 |
21 |
? |
2 |
5 |
5 |
|
Kim et al. [12] |
15 |
40 |
10 |
2 |
1 |
3 |
0 |
|
Present report |
17 |
50 |
8 |
1 |
2 |
4 |
1 |
Among various prognostic parameters of survival in patients with cervical cancer, the most important factors include clinical stage and LN status [
18]. Additionally, high-grade tumor, positive resection margin, parametrial invasion, and deep cervical invasion are considered as high-risk factors for recurrence of early-stage cervical cancer (stage IA2–IIA) [
181920]. In our study, all cases of recurrence represented stage IB1 disease. Patient 6 manifested high-risk factors such as grade-2 tumor and deep cervical invasion. However, the remaining 3 patients showed no high-risk factor. Patients had well-differentiated tumor, superficial cervical invasion, no LVSI, and no LNM. These results suggest that VGA might have prognostic factors different from other types of cervical carcinoma. VGA is too rare to provide a detailed and concrete description on its clinicopathological features and survival outcomes.
In contrast to favorable outcome of VGA, our study disputes the safety of ovarian preservation in young women with VGA. In studies of cervical cancer, several risk factors of ovarian metastasis have been proposed, including large tumor size, high-grade tumor, deep stromal invasion, LVSI, LNM, and endometrial invasion [
2122]. In our study, however, 2 patients had a recurrence at adnexa despite the absence of risk factors. A recent meta-analysis of stages IB–IIB cervical cancer revealed that adenocarcinoma (2.7%) increased the risk of ovarian metastasis compared with SCC (0.7%) [
15]. Although the number of patients in this study was small, the results showed that adnexal recurrence may be more common in VGA, compared to usual adenocarcinomas.
Ovarian function is important for quality of life in premenopausal women. Although BSO in young patients with cervical cancer eliminates the possibility of concealed metastasis in adnexa, the procedure can induce surgical menopause. Currently, there is no consensus on ovarian preservation in young patients with early-stage cervical cancer. The decision on performing simultaneous BSO is mainly based on 2 factors: patient's age at diagnosis and likelihood of ovarian metastasis. A prior study suggested that ovarian preservation was considered in SCC, while BSO was recommended in patients with adenocarcinoma irrespective of age [
16]. No study has reported the safety of ovarian preservation in young patients with VGA. The results of our study show that simultaneous BSO is appropriate for young women with stage IB–IIA VGA undergoing surgical procedures.
This study had a small number of cases due to rarity of VGA. In addition, this study was retrospectively designed at a single institution. Nonetheless, all patients had long-term follow-up data to provide valuable information on survival outcomes.
In conclusion, we observed that VGA of the uterine cervix was associated with favorable prognosis and commonly occurred in younger women. Because of favorable features, less radical surgery or fertility-sparing surgery is safe for patients with early-stage VGA, especially in young women. However, the management of young women with VGA of stage IB or higher must be selected cautiously. Young women with stages IB–IIA VGA may be safe to receive simultaneous BSO when undergoing surgical procedures. A large prospective study is required to investigate the treatments for and outcomes of VGA of the uterine cervix.






 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download