Abstract
Objective
Considering the increased use of [18F]FDG PET or PET/CT, the clinical significance of thyroid incidentalomas is the subject of controversy. The aim of this study was to determine the incidence of malignancies associated with thyroid incidentalomas detected by pre-treatment PET or PET/CT in patients with cervical cancer.
Methods
We retrospectively reviewed the medical records of patients with cervical cancer who had thyroid incidentalomas detected
by pre-treatment PET or PET/CT and were treated at our institute between January 2001 and December 2009.
Results
Of 327 patients who underwent pre-treatment PET or PET/CT, 33 patients had thyroid incidentalomas (10.1%) and 4 patients were diagnosed with thyroid malignancies by percutaneous needle aspiration (PCNA) or surgery. To put it concretely, of 33 patients with thyroid incidentaloma, 16 patients had a diffuse uptake and 17 patients had a focal uptake. Four of 17 patients with focal uptake were diagnosed with thyroid malignancies (23.5%). One patient with a focal uptake had an atypical cell based on PCNA, but did not undergo additional studies. The mean SUVmax of thyroid malignancies did not differ from that of benign thyroid diseases.
Recently, the clinical use of [18F]FDG PET or PET/CT has rapidly increased as a management tool for staging or localization of metastatic disease in patients with various malignancies. Uptake of FDG in the normal thyroid gland is very low and is usually not visualized on whole-body PET or PET/CT [1]. Occasionally, thyroid incidentalomas are shown on PET or PET/CT as a focal or diffuse increase in FDG uptake. The clinical issue is whether or not thyroid incidentalomas are benign or malignant. Considering the convenience and increased use of PET or PET/CT in pre-treatment assessment of patients with cancer, the clinical significance of thyroid incidentalomas is an important issue.
Until now, many investigators have shown the results which have focused on the incidence of thyroid incidentalomas and the rate of malignancies associated with thyroid incidentalomas on PET or PET/CT in patients with malignancy. Based on our experience, the incidence of thyroid incidentalomas in patients with cervical cancer is higher than expected. However, there are no studies which have focused on the patients with cervical cancer.
In the current study we determined the incidence of thyroid incidentalomas and the rate of malignancies associated with thyroid incidentalomas detected by pre-treatment PET or PET/CT in patients with cervical cancer.
The medical records of patients with cervical cancer who had thyroid incidentalomas by pre-treatment PET or PET/CT and were treated at our institute between January 2001 and December 2009 were reviewed retrospectively. Age, cervical cancer stage, type of thyroid incidentalomas (focal and diffuse), the maximal standardized uptake value (SUVmax) of the thyroid incidentalomas, thyroid ultrasonography (USG) findings, serum thyroid-stimulating hormone (TSH) level, percutaneous needle aspiration (PCNA) of the thyroid incidentalomas results, and final biopsy results from lobectomy or thyroidectomy specimens were obtained. Approval from the Institutional Review Board was obtained for this retrospective study (K-1009-002-071).
Until September 2005, PET was performed on an advance HR+ Scanner (General Electric, Waukesha, WI, USA). After September 2005, we used the following PET/CT scanners: Biograph 6 (Siemens Medical Solutions, Malvern, PA, USA); or Discovery LS (General Electric Medical Systems, Milwaukee, WI, USA). Each scan was obtained following the protocol. Patients were fasted at least 6-hour before the PET acquisition. Intravenous injection of 440±60 MBq (range, 165 to 758 MBq) of FDG was followed by a tracer up take phase of about 60 minutes, during which the patients sat in a quiet room without talking.
The CT scan was performed before emission PET scans. The current of the CT tube was adjusted according to patient weight. The CT data were resized from a 512×512 matrix to a 128×128 matrix to match the PET data in order to generate a CT transmission map and to fuse images. PET emission data were acquired for five to seven bed positions, typically from the base of the skull through the upper thigh. PET images were reconstructed using CT for attenuation correction with the ordered-subsets expectation maximization algorithm (two iterations, eight subsets) and a 5-mm Gaussian filter using a 128×128 matrix.
Thyroid incidentalomas was defined as a newly identified thyroid lesion on PET or PET/CT in a patient without a previous, known history of thyroid disease. FDG uptake in less than 1 lobe was defined as a focal lesion, whereas uptake in the entire thyroid gland was considered a diffuse pattern [2].
Thyroid nodules satisfying any one of the following conditions were classified as malignant: 1) hypoechogenicity, 2) taller shape, 3) ill-defined margin, 4) central vascularity, 5) incomplete halo, and 6) micro- or macro-calcification [3,4]. Cases that did not satisfy any of those six criteria were considered as benign nodule on USG examinations.
PCNA was performed using a 21-guage needle on a 10-mL syringe under US guidance. Specimens were smeared on glass slides and stained using the Papanicolaou method. A cytologic diagnosis was made by experienced cytopathologists in our institution. Cytologic diagnosis was as followings; 1) nondiagnostic applies to specimens that are unsatisfactory owing to blood, overly thick or air dried smears, or an inadequate number of follicular cells; 2) benign was made by cytologic findings of an adequately cellular specimen composed of varying proportions of colloid and benign follicular cells arranged as macrofollicles and macrofollicle fragments; 3) atypia of undetermined significance (AUS) was diagnosed when the results of PCNA cytology are not easily classified into the benign, suspicious, or malignant categories; 4) follicular neoplasm was made by cytologic findings of high cellularity and colloid is scant or absent; 5) suspicious for malignancy was classified when only 1 or 2 characteristic features of papillary thyroid carcinoma are presented or a malignant diagnosis cannot be made with certainty; 6) malignant was used whenever the cytomorphologic features are conclusive for malignancy [5].
Data were expressed as the percentage of focal and diffuse incidental thyroid FDG uptake among the population. The difference in SUVmax between benign and malignant groups was analyzed by a Student's t-test, and significance was set at a p<0.05. Data were analyzed using SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA).
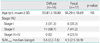
Total 1,271 patients were newly diagnosed as cervical cancer, and 327 patients underwent pre-treatment PET or PET/CT during the study period. We recommended PET or PET/CT to all patients before starting treatment; however, 75% of all patients did not undergo pre-treatment PET or PET/CT due to long waiting time for evaluation or their own economic problems. Of 327 patients, 33 patients had thyroid incidentalomas (10.1%). Twenty nine of 33 patients (89.7%) had cervical cancer with early stage (Table 1). The mean SUVmax of patients with thyroid incidentaloma was 4.24 for diffuse uptake and 8.40 for focal uptake, without a statistical difference between these groups (p=0.08).
Sixteen of 17 patients with focal uptake underwent thyroid USGs and PCNAs. Only one patient with diffuse uptake underwent a thyroid PCNA and was diagnosed with thyroiditis. One patient with focal thyroid incidentalomas had an AUS based on the PCNA result, but did not undergo additional studies (Fig. 1).
The results of PCNA in patients with focal uptake were as follows: nine patients had benign lesions; three patients had malignancies; two patients had follicular neoplasms; one patient had AUS; and one patient had normal thyroid tissue. Three patients with malignancies and one patient with follicular neoplasm based on PCNA underwent total thyroidectomy or lobectomy, all of whom were confirmed to have thyroid cancer. Therefore, 4 of 17 patients with focal uptake were diagnosed with thyroid cancer by PCNA or surgery (23.5%). One patient with follicular neoplasm refused additional treatment. Three of four patients with thyroid malignancies had a relatively high SUVmax on pre-treatment PET or PET/CT (Table 2). The mean SUVmax of patients with thyroid malignancies was higher than that of patients with benign masses, but the difference of SUVmax was statistically insignificant (17.8 vs. 6.16, respectively, p=0.056).
Thyroid incidentalomas are defined as newly identified focal thyroid lesions encountered during imaging studies, including CT, MRI, and USG. Although some studies using high-resolution USG have reported the risk of cancer of thyroid incidentalomas 1.5-10% [6], these modalities (CT, MRI, and USG) are not specific for thyroid malignancy [7].
The current widespread use of PET or PET/CT has resulted in an increase in the detection of thyroid incidentalomas. The incidence of thyroid incidentalomas and the rate of malignancy associated with thyroid incidentalomas on PET or PET/CT varies with the study population. Generally, the incidence of thyroid incidentalomas is 2-9% [3,8,9], and the rate of malignancy associated with focal thyroid incidentalomas is as high as 28-64% [2,10]. Especially, some authors reported that the prevalence of thyroid incidentaloma in cancer screening group was about 3% and this value was not differ from metastasis work-up group [9]. In another study, the authors showed the results that the incidence of thyroid incidentalomas in patients with gynecologic cancer is 10.4% and the rate of malignancy of diffuse and focal thyroid incidentalomas is 9.7% [11].
In our study, thyroid incidentalomas were identified in 33 of 327 patients with cervical cancer, corresponding to a prevalence of 10.1%. This finding is similar or higher than previously reported in the literature [3,8,9,11]. However, it was remarkable that the incidence of malignancy in focal FDG uptake in patients with cervical cancer is 23.5% and which is higher than previous reports included all gynecologic malignancies [11].
Some studies have reported that the average SUVmax of malignant lesions is significantly higher than benign lesions [9,11,12]. A recent study even showed the result that the size and visual grade on the PET/CT were the potent predictors for differentiation of malignancy in focal thyroid incidentaloma rather than the mean SUVmax [13]. In this study, the mean SUVmax was 6.16 for benign lesions and 17.8 for malignant lesions, with a marginal difference between the two groups (p=0.056). Although some authors suggest that the mean SUVmax of thyroid malignancies were significantly higher than those of benign tumors (p<0.001) [9], the role of SUVmax in differentiating benign from malignant lesions is controversial, because the SUVmax overlaps between benign and malignancy and the study sample number has been small in most previous studies.
We admit that our study has some limitations. First, PET or PET/CT produce functional images that reflect increase rates of glucose metabolism in tumor, and it has many pit-falls in clinical use. Second, the number of patients enrolled in this study was too small to induce a strong conclusion. Therefore, more data and large-scale studies are required to determine the clinical significance of thyroid incidentalomas in patients with cervical cancer.
In conclusion, the incidence of thyroid incidentalomas detected by PET or PET/CT in patients with cervical cancer was 10.1%; approximately one-half of thyroid incidentalomas have focal uptake and one-half of thyroid incidentalomas have diffuse uptake. The rate of malignancy of focal thyroid incidentalomas in patients with cervical cancer was 23.5% and this result was much higher than that in other gynecologic malignancies reported in the previous literature. Because of the high rate of malignancy, histological confirmation including PCNA in patients with focal thyroid incidentalomas is necessary to distinguish between benign and malignant thyroid incidentalomas. SUVmax could be helpful to distinguish malignant thyroid incidentaloma from benign ones.
Figures and Tables
Fig. 1
Flow chart of patient selection process. PET, [18F]FDG PET; USG, ultrasoundgraphy; PCNA, percutaneous needle aspiration; AUS, atypia of undetermined significance.

Table 2
Characteristics of patients with focal thyroid incidentalomas on PET or PET/CT

PET, [18F]FDG PET; SUVmax, maximal standard unit value; USG, ultrasonography; PCNA, percutaneous needle aspiration; TSH, thyroid stimulating hormone; PC, papillary carcinoma; HFC, hyperplastic follicular cell; BFC, benign follicular cell; AUS, atypia of undetermined significance; TT, total thyroidectomy; LND, lymph node dissection; FC, follicular carcinoma.
ACKNOWLEDGMENT
We thank our staffs and research nurses (Hee Sook Lee and Younha Kim) for their contribution in data collection for this study.
References
1. Nakamoto Y, Tatsumi M, Hammoud D, Cohade C, Osman MM, Wahl RL. Normal FDG distribution patterns in the head and neck: PET/CT evaluation. Radiology. 2005. 234:879–885.
2. Eloy JA, Brett EM, Fatterpekar GM, Kostakoglu L, Som PM, Desai SC, et al. The significance and management of incidental [18F]fluorodeoxyglucose-positron-emission tomography uptake in the thyroid gland in patients with cancer. AJNR Am J Neuroradiol. 2009. 30:1431–1434.
3. Kang BJ, O JH, Baik JH, Jung SL, Park YH, Chung SK. Incidental thyroid uptake on F-18 FDG PET/CT: correlation with ultrasonography and pathology. Ann Nucl Med. 2009. 23:729–737.
4. Rago T, Vitti P. Role of thyroid ultrasound in the diagnostic evaluation of thyroid nodules. Best Pract Res Clin Endocrinol Metab. 2008. 22:913–928.
5. Cibas ES, Ali SZ. NCI Thyroid FNA State of the Science Conference. The Bethesda system for reporting thyroid cytopathology. Am J Clin Pathol. 2009. 132:658–665.
6. Burguera B, Gharib H. Thyroid incidentalomas: prevalence, diagnosis, significance, and management. Endocrinol Metab Clin North Am. 2000. 29:187–203.
7. Mazzaferri EL. Thyroid cancer in thyroid nodules: finding a needle in the haystack. Am J Med. 1992. 93:359–362.
8. Cohen MS, Arslan N, Dehdashti F, Doherty GM, Lairmore TC, Brunt LM, et al. Risk of malignancy in thyroid incidentalomas identified by fluorodeoxyglucose-positron emission tomography. Surgery. 2001. 130:941–946.
9. Kang KW, Kim SK, Kang HS, Lee ES, Sim JS, Lee IG, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-fluorodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endocrinol Metab. 2003. 88:4100–4104.
10. Chen W, Parsons M, Torigian DA, Zhuang H, Alavi A. Evaluation of thyroid FDG uptake incidentally identified on PET/CT imaging. Nucl Med Commun. 2009. 30:240–244.
11. Bae JS, Chae BJ, Park WC, Kim JS, Kim SH, Jung SS, et al. Incidental thyroid lesions detected by PET/CT: prevalence and risk of thyroid cancer. World J Surg Oncol. 2009. 7:63.
12. Choi JY, Lee KS, Kim HJ, Shim YM, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterization. J Nucl Med. 2006. 47:609–615.
13. Kim BH, Na MA, Kim IJ, Kim SJ, Kim YK. Risk stratification and prediction of cancer of focal thyroid fluorodeoxyglucose uptake during cancer evaluation. Ann Nucl Med. 2010. 24:721–728.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download