Abstract
Objective
To evaluate the efficacy of concurrent chemoradiation (CCRT) using 5-flurouracil (5-FU) and cisplatin for locally advanced cervical cancer.
Methods
We reviewed the medical records of 57 patients with locally advanced cervical cancer (stage IIB-IVA and bulky IB2-IIA tumor) who underwent the CCRT at Dong-A University Hospital from January 1997 to June 2007. The CCRT consisted of 5-FU, cisplatin and pelvic radiation. Every three weeks, 75 mg/m2 cisplatin was administered on the first day of each cycle and 5-FU was infused at the dose of 1,000 mg/m2/d from the second day to the fifth day of each cycle. Radiation was administered to the pelvis at a daily dose of 1.8 Gy for five days per week until a medium accumulated dose reached to 50.4 Gy. If necessary, the radiation field was extended to include paraaortic lymph nodes. Consolidation chemotherapy was performed using 5-FU and cisplatin.
Results
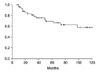
Fifty-seven patients were enrolled and the median follow-up duration was 53 months (range 7-120 months). The overall response rate was 91.5% (74% complete response and 17.5% partial response). The 5-year overall survival and 3-year progression free survival rates were 69.4% and 74.9%, respectively. During the follow-up period (median 23 months, range 7-60 months), fourteen patients were diagnosed as recurrent disease.
Although cervical cancer was one of the commonest cancers in women and had a high mortality rate, the early detection of precancerous or early stage disease by screening test has decreased the incidence and improved the prognosis of patients with cervical cancer. However, cervical cancer is still second in incidence and third in mortality among gynecologic cancers.1 In addition, 80% of cervical cancer of the globe occurs in the developing countries and cervical cancer is the most common cause of cancer-related death in those countries.2 Although the incidence has been decreasing in the last 10 years, the cervical cancer is the fifth common cancer in women and the most common gynecologic cancer in Korea.3
Both surgery and radiation have been known to be effective in the treatment of small-sized cervical cancer. For locally advanced or bulky cervical cancer, radiation has been the standard treatment modality. The rationale of radiation in the treatment of locally advanced or bulky cervical cancer was that the cervical cancer has a tendency of initial local progression and late metastasis. However, for 20 years, there has been no significant advances in the treatment of locally advanced or bulky cervical cancer.4
To improve the treatment outcome in locally advanced or bulky cervical cancer, many studies have been reported on concurrent chemoradiation (CCRT). The theoretical advantages of CCRT were that the chemotherapy agent may be effective in eradicating the subclinical metastasis and act as a radiosensitizer.5 The representative chemotherapy drugs used for CCRT were cisplatin, 5-fluorouracil (5-FU), hydroxyurea, ifosfamide, mitomycin-C, and bleomycin.6 In the late 1990s, five randomized prospective studies reported the superiority of CCRT to radiation alone in the treatment of locally advanced or high-risk cervical cancer. Thereafter, CCRT has been regarded as the primary treatment modality for locally advanced or high-risk cervical cancer.7-11
We conducted this study to assess the response, survival, recurrence rates, and adverse effects in patients with locally advanced or bulky cervical cancer who were treated with CCRT using 5-FU and cisplatin.
Records of patients with locally advanced or bulky cervical cancer who were diagnosed at Dong-A University Hospital, from January 1997 to June 2007, were reviewed for this study. Patients who were treated with primary surgery, neoadjuvant chemotherapy, or radiation alone were excluded. Among the identified 60 patients, three patients were excluded due to incomplete medical records. The remaining 57 patients underwent CCRT with 5-FU and cisplatin. Information on response to treatment and adverse effects were obtained retrospectively via reviewing medical records.
The bulky tumor was defined as a tumor with a diameter equal to or longer than 5 cm. Tumors with stage IIB, IIIA, IIIB, and IVA were regarded as the locally advanced tumors. The diagnosis of lymph node involvement was made when there was a lymph node with a diameter equal to or larger than 1cm on computed tomography (CT) or magnetic resonance imaging (MR).
History, physical examination, complete blood count, chest X-ray, CT or MR of the abdomen and pelvis area were performed before treatment.
Radiation was performed with four-field box technique using 15 MV linear accelerator. The borders of the radiation field were as follows: the midline between the fourth and fifth lumbar vertebrae for the upper border, ischial spine for the lower border, and the imaginary lines which are 1.5-2 cm lateral to the pelvic cavity for the lateral borders. From the lateral view, the anterior border was the outer margin of pubic bone and the posterior border was the midline between the second and third sacrum. Patients received external beam radiation to the pelvic area at a daily dose of 1.8 Gy for five days per week until the accumulated dose reached to 45 Gy. Every patient underwent 6 to 7 cycles of the high-dose brachytherapy with a dose of 5 Gy at the A point per each cycle. Extended field radiation was performed for patients with suspicious para-aortic lymph node involvements.
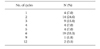
During the radiation therapy, chemotherapy was administered every three weeks. The patients received the intravenous cisplatin 75 mg/m2 on the first day and 5-FU 1,000 mg/m2/d from the second day to fifth day of each cycle. Additional cycles of chemotherapy were given to patients who responded partially or poorly to the initial treatment and the mean number of cycles was six (range 1-12) (Table 1).
To evaluate the treatment response and to detect recurrence, pelvic examination, measurement of serum levels of squamous cell carcinoma antigen (SCC), and Pap smears were performed every two months for the first year, every three months for the second year, and every six months thereafter.
If recurrence was suspected, CT or MR of the suspicious area was performed. Also, positron emission tomography has been performed since 2006. If necessary, biopsies for suspicious lesions were performed.
Adverse effects were evaluated by examining the symptoms and signs, the results of laboratory or imaging studies, and were graded according to the GOG common toxicity criteria grade (October 1988).
Gastrointestinal toxicity was evaluated by measuring the severity of nausea / vomiting, diarrhea, the level of bilirubin and aminotransferase (GOT/GTP). Myelotoxicity was evaluated by measuring the level of hemoglobin, white blood cell count, lymphocyte count, and platelet count. Nephrotoxity was evaluated by measuring the level of serum creatinine. Toxicities observed within 30 days after the start of treatment were regarded as acute toxicities, and otherwise as chronic toxicities.
Treatment outcome was evaluated with overall survival and disease free survival rates. Survival curves were plotted using the Kaplan-Meier Method.
The mean age was 53 years (range 33-72 years). The longest diameter of tumor based on MR was 9 cm and 14 patients had a bulky tumor over 5 cm. The number of patients with each FIGO stage was as follows: three patients with IB2, seven patients with IIA, 40 patients with IIB, two patients with IIIB, and five patients with IVA. Histologic type was squamous cell carcinoma in 55 patients and adenocarcinoma in 2 patients. Parametrial invasion was present in 47 patients. Lymph node metastasis was present in 40 patients; six out of 40 patients had a paraaortic lymph node metastasis (Table 2).
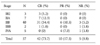
Based on physical examination, the mean time for the disappearance of tumor was three months after treatment. Complete and partial remission was achieved in 42 (73.7%) and 10 (17.5%) patients, respectively. However, five patients (8.8%) were refractory to treatment. Responses according to stages are presented in Table 3.
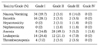
Several acute toxicities were observed during the treatment period. Nausea and vomiting was observed in most patients: grade 1 in 34 patients (59.7%), grade 2 in two patients (3.5%), and grade 3 in eight patients (14%). Radiation-induced enterocolitis was diagnosed in one-third of patients: grade 1 in 16 patients (28.1%), grade 2 in two patients (3.5%), and grade 3 in two patients (3.5%). Grade 2 and 3 hepatotoxicity was present in two (3.5%) and one (1.8%) patients, respectively. Nephrotoxicity was observed in 2 patients: grade 2 in a patient (1.8%) and grade 3 in a patient (1.8%). Leucopenia was observed in over half of patients: grade 1 in 14 patients (24.6%), grade 2 in 12 patients (21.1%), and grade 3 in four patients (7.0%). Anemia was present in two-thirds of patients: grade 1 in eight patients (14.0%), grade 2 in 28 patients (49.1%), grade 3 in three patients (5.2%), and grade 4 in a patient (1.8%). Thrombocytopenia was observed in eight patients: grade 1 in four patients (7.0%), grade 2 in two patients (3.5%), and grade 3 in two patients (3.5%) (Table 4).
Observed chronic toxicities of CCRT were as follows: intestinal obstruction in 1 patient (1.8%), cystitis in 2 patients (3.5%), colitis in 5 patients (8.8%), rectovaginal fistula in 3 patients (5.2%), cystovaginal fistula in 1 patient (1.8%), and leg edema in 3 patients (5.2%) (Table 5).
Fourteen recurrences were observed during the follow-up period. One out of seven patients with IIA cervical cancer experienced lung metastasis. Among the 40 patients with IIB cervical cancer, 3 patients were refractory to treatment and 11 patients experienced recurrence. Out of 11 patients with a recurrence, 4 patients had local recurrence and 7 patients had distant recurrence. Sites of distant recurrences were as follows: lung in 4 patients, paraaortic lymph node in 1 patient, liver in 1 patient, and bone in 1 patient. One out of two patients with IIIB cervical cancer was diagnosed as having a recurrent tumor in the left supraclavicular lymph nodes, although she had achieved complete remission initially. Four out of five patients with IVA cervical cancer had a partial response to initial treatment, but a recurrent tumor in the bone was detected in one out of four patients. The mean interval from the initial treatment to recurrence was 23 months (range 7-60 months). Out of 14 patients with recurrence, at the last follow-up, 13 patients died and one patient was alive after salvage treatment. The mean overall survival time was 16.7 months.
Radiation has been used as the main treatment modality for inoperable, locally advanced cervical cancer. However, considerable treatment failures were observed in patients who were treated with radiotherapy alone. For example, 20-50% of patients with stage IIB cervical cancer and 50-75% of patients with stage III cervical cancer suffered local recurrence.12-14 To decrease the local recurrence, several strategies were adopted. For example, hypoxic sensitizers,15,16 hyperbaric oxygen,17 radioprotector,18 neutron therapy,19 hyperthermia,20 and hyperfractionation21 were attempted to decrease the local recurrence. In the 1990s, through the development of new chemotherapy drugs, the addition of chemotherapy to radiation was suggested to decrease the rate of local recurrence.
The chemotherapy drugs were suggested to augment the therapeutic effect of radiation through cell cycle specific cytotoxicity, cell synchronization to more radiosensitive phase, decreased tumor repopulation, and disturbing repair of radiation-induced cell damage.5,22
The most common chemotherapy drugs used for CCRT are 5-FU and cisplatin. There have been many studies on the combination of 5-FU and cisplatin in patients with cervical cancer.23,24 5-FU exhibits the synergistic effect with radiation by inhibiting the DNA replication in cells which are damaged by radiation. After it was shown to be effective in gastrointestinal cancers, 5-FU has been used for treatment of cervical cancer. 5-FU was administered for four to seven days per three or four week. The common toxicities of 5-FU are diarrhea and myelotoxocity.25 In this study, 5-FU was administered intravenously from the second day to the fifth day of each cycle. Cisplatin is known to act synergistically with the radiation by killing the cells with radiation-induced sublethal damage. The common toxicities of cisplatin are nephrotoxicity, upper gastrointestinal toxicity, and myelosuppression.26 In this study, cisplatin 75 mg/m2 were administered at the first day of each chemotherapy cycle.
In the late 1990s, there were five randomized prospective studies on the efficacy of CCRT in patients with locally advanced or high-risk cervical cancers. Rose et al. evaluated the efficacy of CCRT with three different chemotherapy regimens: cisplatin only, cisplatin+5-FU+hydroxyurea, and hydroxyurea only. The mean follow-up duration was 35 months. They reported that the overall survival rate of the patients with cervical cancer who were treated with cisplatin-based CCRT was 67%.7 Whitney et al. showed that the patients treated with CCRT using 5-FU and cisplatin had the longer disease-free survival than the patients treated with CCRT using hydroxyurea.8 Also, Keys et al. reported that the treatment efficacy was improved by adding 5-FU and cisplatin to radiation in patients with cervical cancer.9 Morris et al. compared the 5-year overall survival rate of patients treated with radiation alone with that of patients treated with CCRT. The chemotherapy regimen used for CCRT was 5-FU and cisplatin. The mean follow-up duration was 43 months. The 5-year overall survival rate of patients treated with radiation alone was 58% and that of patients treated with CCRT was 73%. These findings showed that the CCRT is superior to the radiation alone in the treatment of locally advanced cervical cancer.10
In this study, the overall response rate was 91.5% (complete response 74%, partial response 17.5%); 3-year disease-free survival rate was 74.9%; 5-year overall survival rate was 69.4%. These results were similar with those of previous studies. Therefore, we consider that the CCRT is more effective than radiation alone in the treatment of locally advanced cervical cancer.
Because every drug had its own adverse effects, we expected that CCRT would cause more adverse effects than radiation alone. In a previous study, adverse effects were observed in 5-15% of patients with cervical cancer who were treated with radiation alone.27 However, in a study conducted by Mancuso et al., adverse effects were reported in 19.2% of patients who were treated with CCRT.28 Intestinal toxicity and myelotoxicity accounted for 11.5% and 23.1% of adverse effects caused by CCRT, respectively. In 1988, GOG formulated criteria by which the toxicities caused by chemotherapy could be assessed and graded. In this study, we graded the toxicities according to the GOG criteria. Toxicities occurred within 30 days after treatment were regarded as acute toxicities, otherwise as chronic toxicities. In this study, acute toxicities were as follows: grade 3 nausea and vomiting in eight patients (14%), grade 3 hepatotoxicity in a patient (1.8%), grade 3 nephrotoxicity in a patient (1.8%), grade 3 leucopenia in four patients (7.0%), grade 3 anemia in three patients (5.2%), grade 4 anemia in a patient (1.8%), grade 3 thrombocytopenia in two patients (3.5%). Chronic toxicities were as follows: small bowel obstruction in a patient (1.8%), cystitis in two patients (3.5%), colitis in five patients (8.8%), rectovaginal fistula in three patients (5.2%), cystovaginal fistula in a patient (1.8%), leg edema in three patients (5.2%). The patient with small bowel obstruction died of sepsis. Rectovaginal fistula was corrected by surgery.
In conclusion, the patients treated with the CCRT using 5-FU and cisplatin had better overall survival and disease-free survival rates than the patients treated with radiation alone. Therefore, CCRT using 5-FU and cisplatin are thought to be more effective than the radiation alone in the treatment of locally advanced or bulky cervical cancer.
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005. 55:74–108.
2. Jenal A, Siegel E, Ward E, Murray T, Xu J, Smigal C, et al. Cancer statistics, 2006. CA Cancer J Clin. 2006. 56:106–130.
3. Annual Report of Gynecologic Cancer Registry Program in Korea for 2002 (Jan. 1, 2002-Dec. 31, 2002). Korean J Obstet Gynecol. 2005. 48:1130–1180.
4. Green JA, Kirwan JM, Tierney JF, Symonds P, Fresco L, Collingwood M, et al. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: A systematic review and meta-analysis. Lancet. 2001. 358:781–786.
5. Fu KK. Biological basis for the interaction of chemotherapeutic agents and radiation therapy. Cancer. 1985. 55:2123–2130.
6. Stehman FB, Bundy BN, Kucera PR, Deppe G, Reddy S, O'Connor DM. Hydroxyurea, 5-fluorouracil infusion, and cisplatin adjunct to radiation therapy in cervical carcinoma: A phase I-II trial of the Gynecologic Oncology Group. Gynecol Oncol. 1997. 66:262–267.
7. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999. 340:1144–1153.
8. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph node: A Gynecologic Oncology Group and Southwest Oncology Group Study. J Clin Oncol. 1999. 17:1339–1348.
9. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999. 340:1154–1161.
10. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999. 340:1137–1143.
11. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation-therapy compared with pelvic radiation therapy alone as adjuvant therapy after radicalsurgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000. 18:1606–1613.
12. Coia L, Won M, Lanciano R, Marcial VA, Martz M, Hanks G. The patterns of care outcome study for cancer of the uterine cancer: Results of the second national practice survey. Cancer. 1990. 66:2451–2456.
13. Perez CA. Radiation therapy in the management of cancer of the cervix: Part II. Oncology. 1993. 7:61–76.
14. Jampolis S, Andras EJ, Fletcher GH. Analysis of sites and causes of failure of irradiation in invasive squamous cell carcinoma of the intact uterine cervix. Radiology. 1975. 115:681–685.
15. Simpson JR, Bauer M, Perez CA, Wasserman TH, Emami B, Doggett RL, et al. Radiation therapy alone or combined with misonidazole in the treatment of locally advanced non-oat cell lung cancer: Report of an RTOG prospective randomized trial. Int J Radiat Oncol Biol Phys. 1989. 16:1483–1491.
16. Garcia-Angulo AH, Kagiya VT. Intratumoral and parametrial infusion of a 3-nitronidazole (AK-2123) in the radiotherapy of the uterine cervix cancer: Stage II-III preliminary positive results. Int J Radiat Oncol Biol Phys. 1992. 22:589–591.
17. Brady LW, Plenk HP, Hanley JA, Glassburn JR, Kramer S, Parker RG. Hyperbaric oxygen therapy for carcinoma of the cervix-stages IIB, IIIA, IIIB and IVA: Results of a randomized study by the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys. 1981. 7:991–998.
18. Mitsuhashi N, Takahashi I, Takahashi M, Hayakawa K, Niibe H. Clinical study of radioprotective effects amifostine on long-term outcome for patients with cervical cancer. Int J Radiat Oncol Biol Phys. 1993. 26:407–411.
19. Maor MH, Gillespie BW, Peters LJ, Wambersie A, Griffin TW, Thomas FJ, et al. Neutron therapy in cervical cancer: Results of a phase III RTOG study. Int J Radiat Oncol Biol Phys. 1988. 14:885–891.
20. Hornback NB, Shupe RE, Shidnia H, Marshall CU, Lauer T. Advanced stage IIIB cancer of the cervix treatment by hyperthermia and radiation. Gynecol Oncol. 1986. 23:160–167.
21. Horiot JC, Le Fur R, N'guyen T, Chenal C, Schraub S, Alfonsi S, et al. Hyperfractionation versus conventional fractionation in oropharyngeal carcinoma: final analysis of a randomized trial of the EORTC cooperative group of radiotherapy. Radiother Oncol. 1992. 25:231–241.
22. Vokes EE, Weichselbaum RR. Concomitant Chemotherapy: Rational and clinical experience in patients with solid tumors. J Clin Oncol. 1990. 8:911–934.
23. Robert WS, Hoffman MS, Kavanaugh JJ, Fiorica JV, Greenberg H, Finan MA, et al. Further experience with radiation therapy and concomitant intravenous chemotherapy in advanced squamous carcinoma of the lower female genital tract. Gynecol Oncol. 1991. 43:233–236.
24. Dionet C, Verrelle P. Curability of mouse L1210 leukemia by combination of 5-fluorouracil, cis-diamminedichloroplatinum (II), and low doses of gamma-rays. Cancer Res. 1984. 44:652–656.
25. Grem JL. Mechanisms of Action and Modulation of Fluorouracil. Semin Radiat Oncol. 1997. 7:249–259.
26. Britten RA, Evans AJ, Allalunis-Turner MJ, Pearcey RG. Effect of cisplatin on the clinically relevant radiosensitivity of human cervical carcinoma cell lines. Int J Radiat Oncol Biol Phys. 1996. 34:367–374.
27. Hamberger AD, Unal A, Gershenson DM, Fletcher GH. Analysis of the severe complication of irradiation of carcinoma of the cercix: Whole pelvis irradiation and intracavitary radium. Int J Radiat Oncol Biol Phys. 1983. 9:367–371.
28. Mancuso S, Smaniotto D, Benedetti Panici P, Favale B, Greggi S, Manfredi R, et al. Phase I-II trial of preoperative chemoradiation in locally advanced cervical carcinoma. Gynecol Oncol. 2000. 78:324–328.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download