Abstract
Materials and Methods
Results
References
SUPPLEMENTARY MATERIAL
Supplementary Table 1
Fig. 1
Trends in the age-standardized prevalence of hypertension and the participants with anti-hypertensive medication. (A) The age-standardized prevalence of hypertension. (B) The age-standardized prevalence of the participants with anti-hypertensive medication. Standardized to the age structure of the 2005 Korean population. p for trend was determined by logistic regression after setting the KNHANES phase as the continuous variable. KNHANES, Korean National Health and Nutrition Examination Survey.
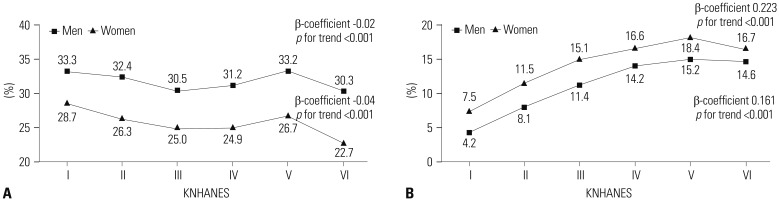
Fig. 2
Prevalence trends of less-than-normotensive BP or less-than-hypertensive BP according to KNHANES phase. (A) The prevalence of less-than-normotensive BP. (B) The prevalence of less-than-hypertensive BP. p for trend was determined by linear regression analysis with weighting of survey design. Less-than-normotensive BP, SBP <120 mm Hg and DBP <80 mm Hg; less-than-hypertensive BP, SBP <140 mm Hg and DBP <90 mm Hg. KNHANES, Korean National Health and Nutrition Examination Survey; BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure.
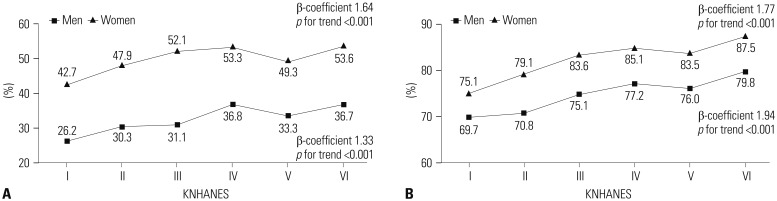
Fig. 3
ORs for less-than-normotensive or less-than-hypertensive BP according to KNHANES phase. (A) ORs trends for less-than-normotensive and less-than-hypertensive BP in men. (B) ORs trends for less-than-normotensive and less-than-hypertensive BP in women. Less-than-normotensive BP, SBP <120 mm Hg and DBP <80 mm Hg; less-than-hypertensive BP, SBP <140 mm Hg and DBP <90 mm Hg. Adjusting for age, body mass index, fasting plasma glucose, total cholesterol, sufficient activity, heavy alcohol drinking, smoking status, energy intake, and sodium intake. ORs, odds ratios; KNHANES, Korean National Health and Nutrition Examination Survey; BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure.
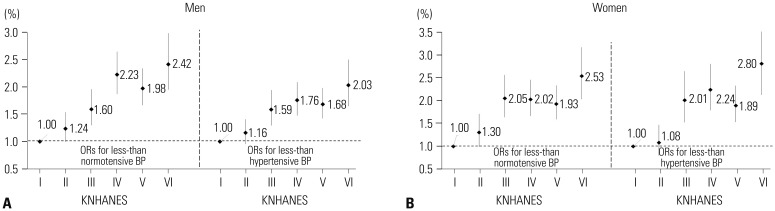
Table 1
Participant Characteristics according to KNHANES Phase
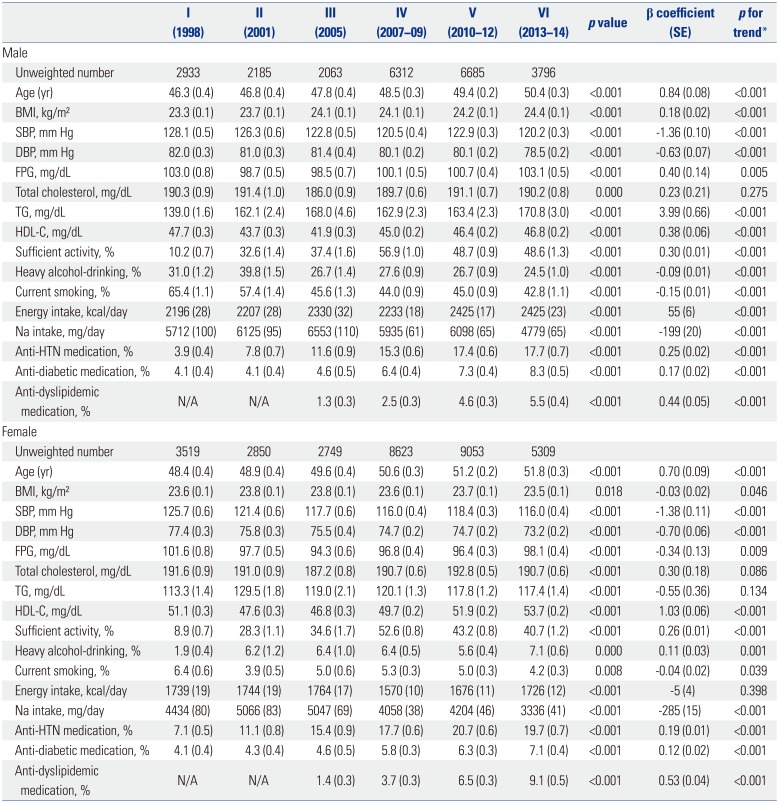
KNHANES, Korean National Health and Nutrition Examination Survey; SE, standard error; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; Na, sodium; HTN, hypertension.
All data are presented as a mean (SE) or percentage.
*p for trend was determined by linear regression analysis with weighting of survey design.
Table 2
Characteristics of the Participants Taking Anti-Hypertensive Medication according to KNHANES Phase
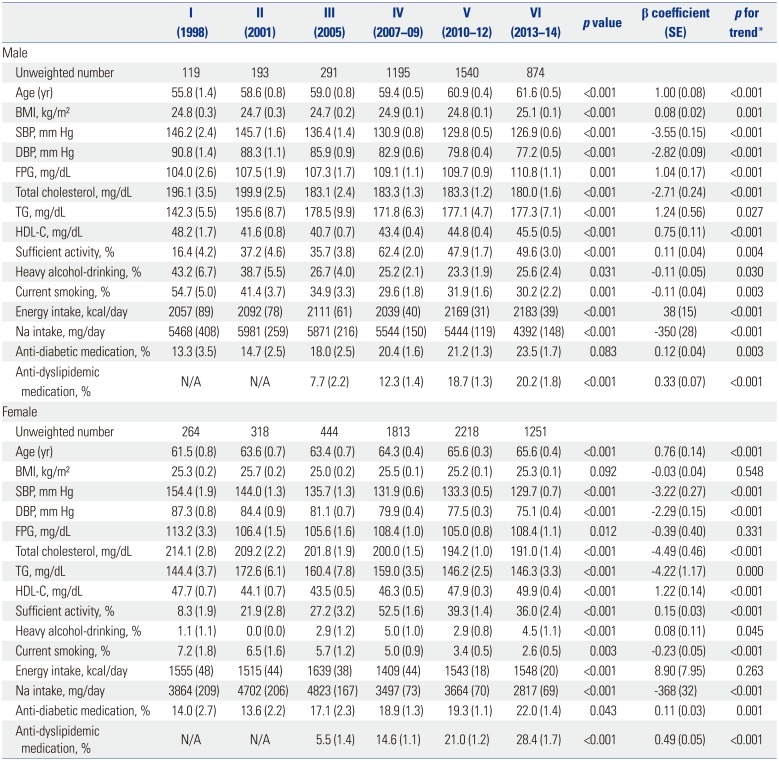
KNHANES, Korean National Health and Nutrition Examination Survey; SE, standard error; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; Na, sodium.
All data are presented as a mean (SE) or percentage.
*p for trend was determined by linear regression analysis with weighting of survey design.
Table 3
Characteristics of the Participants Not Taking Anti-Hypertensive Medication According to KNHANES Phase
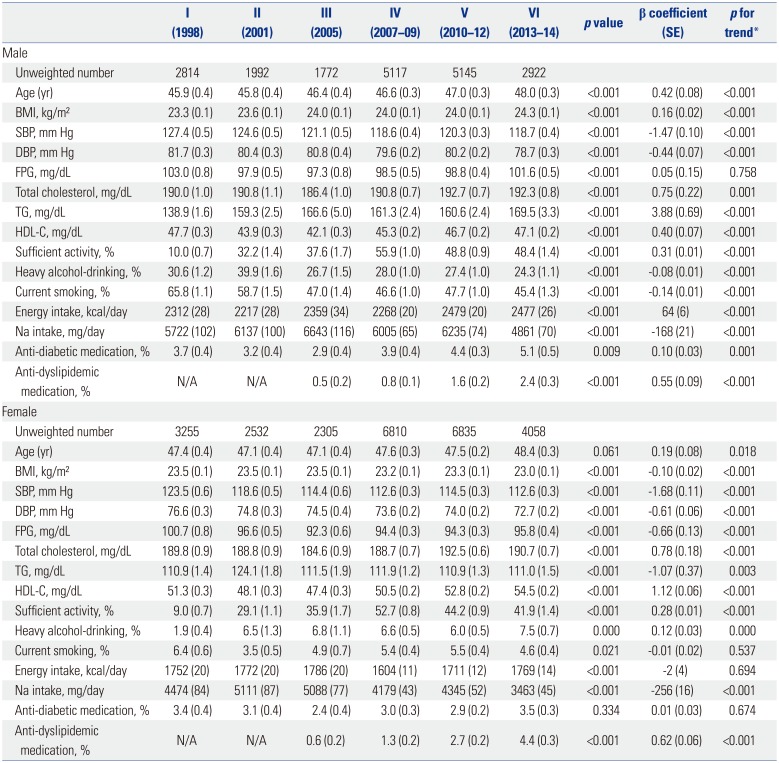
KNHANES, Korean National Health and Nutrition Examination Survey; SE, standard error; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; FPG, fasting plasma glucose; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; Na, sodium.
All data are presented as a mean (SE) or percentage.
*p for trend was determined by linear regression analysis with weighting of survey design.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download