Abstract
Purpose
The purpose of this study was to determine the effect-site concentration (Ce) of remifentanil in 50% of patients (EC50) and 95% of patients (EC95) for smooth laryngeal mask airway (LMA) removal in adults under propofol and remifentanil anesthesia.
Materials and Methods
Twenty-five patients of ASA physical status I-II and ages 18-60 years who were to undergo minor gynecological or orthopedic surgery were assessed in this study. Anesthesia was induced and maintained with propofol and remifentanil target-controlled infusion (TCI). Remifentanil was maintained at a predetermined Ce during the emergence period. The modified Dixon's up-and-down method was used to determine the remifentanil concentration, starting from 1.0 ng/mL (step size of 0.2 ng/mL). Successful removal of the LMA was regarded as absence of coughing/gagging, clenched teeth, gross purposeful movements, breath holding, laryngospasm, or desaturation to SpO2<90%.
Results
The mean±SD Ce of remifentanil for smooth LMA removal after propofol anesthesia was 0.83±0.16 ng/mL. Using isotonic regression with a bootstrapping approach, the estimated EC50 and EC95 of remifentanil Ce were 0.91 ng/mL [95% confidence interval (CI), 0.77-1.07 ng/mL] and 1.35 ng/mL (95% CI, 1.16-1.38 ng/mL), respectively.
During removal of laryngeal mask airways (LMA) at emergence, airway reflexes, such as coughing, biting, laryngospasm, or bronchospasm, should be obtunded to prevent airway complications.1,2 Removal of a LMA during an awake state can increase complications associated with airway hyper-reactivity and damage the LMA.1,3 However, in a deep anesthetic state, suppression of airway reflexes may increase the incidence of aspiration and airway obstruction.4,5 Therefore, providing an appropriate depth of anesthesia to achieve airway reflex suppression without delayed awakening is important for safe removal of a LMA.
Remifentanil is a potent short-acting opioid that provides rapid and predictable recovery. Maintaining a low dose remifentanil infusion during emergence after total intravenous anesthesia (TIVA) or balanced anesthesia decreases the cough reflex during tracheal extubation and the hemodynamic response, with minimal effects on delayed recovery.6,7,8 Therefore, remifentanil can be an ideal agent for smooth LMA removal during emergence. A recent study showed that maintaining remifentanil infusion during emergence from desflurane anesthesia reduces the incidence of complications associated with LMA removal without delayed recovery.9 However, to date, no dose-finding study has investigated effective concentrations of remifentanil for facilitating smooth LMA removal after propofol and remifentanil anesthesia. The aim of this study was to determine the effect-site concentration (Ce) of remifentanil in 50% of patients (EC50) and 95% of patients (EC95) for smooth LMA removal in adults under target-controlled infusion (TCI) with propofol and remifentanil.
This study was approved by the Institutional Review Board of Ajou University Hospital (Suwon, Korea) and registered at ClinicalTrials.gov (NCT 01931683). Written informed consent for the study was acquired from each patient. Twenty-five patients of ASA physical status I-II and ages 18-60 years who were to undergo minor orthopedic or gynecological surgery under general anesthesia were assessed. Patients were excluded for a suspected difficult airway, reactive airway disease, recent upper respiratory tract infection, gastrointestinal reflux, and obesity (body mass index>30 kg/m2).
No sedative premedication was given before surgery. Upon arrival in the operating room, all patients were monitored with an electrocardiogram, pulse oximeter, noninvasive blood pressure, and bispectral index (BIS) (BIS VISTA™ monitor, four electrode sensor; Aspect Medical Systems, Norwood, MA, USA). Induction of anesthesia was performed with propofol TCI at an Ce of 5.0 µg/mL and remifentanil TCI at a Ce of 4.0 ng/mL, using a two-channel TCI pump (Orchestra®, Fresenius Vial, Brezins, France). The pharmacokinetic models (Marsh model10 and Minto model11) were applied for calculating target Ces of propofol and re-mifentanil. Following loss of consciousness, the patients' lungs were manually ventilated with 100% oxygen through a face mask connected to a semi-closed anesthesia circuit. A muscle relaxant was not used. After reaching a BIS <50 and appropriate jaw relaxation was achieved, a LMA Supre-me (Laryngeal Mask Company Limited, Singapore, Singapore) was inserted (size 3 for women and size 4 for men). Mechanical ventilation was adjusted to maintain end-tidal CO2 at 35-40 mm Hg in 50% oxygen and air (total flow 3 L/min). Anesthesia was maintained with an effect-site TCI of propofol and remifentanil at 2.5-4.0 µg/mL and 2.0-4.0 ng/mL, respectively, to maintain blood pressure and heart rate (HR) within 20% of baseline values during the surgery.
After completing the surgery, the propofol infusion was stopped, and the remifentanil Ce was adjusted according to a predetermined concentration. Mechanical ventilation was stopped, and manual ventilation was performed with 100% oxygen at a total flow of 4 L/min, maintaining an end-tidal CO2 of 35-45 mm Hg. Once remifentanil Ce reached the predetermined value, it was maintained throughout the emergence period until 1 min after LMA removal. During the emergence period, patients were asked to open their eyes verbally at 30 s intervals without tactile stimulation. When patients opened their eyes spontaneously or responded to verbal commands, we encouraged them to breathe deeply, and the LMA was removed with the cuff inflated. Then, patients were given 100% oxygen using a facemask with jaw lifting. After confirming stable vital signs, the patients were transferred to the post-anesthesia care unit (PACU). In the PACU, Ramsay score, visual analogue scale (VAS) for pain, and duration of stay were measured, and fentanyl 1 µg/kg was administered if pain scores exceeded 5 on the VAS.
Hemodynamic data and BIS were recorded at baseline, at the end of surgery, prior to LMA removal, and 1 min and 2 min after LMA removal. Emergence time was defined as the time from discontinuation of propofol to LMA removal.
The remifentanil Ce for each patient was determined according to the response of the previously tested patient, using the modified Dixon's up-and-down method.12 The first patient was tested at a 1.0 ng/mL Ce of remifentanil (step size of 0.2 ng/mL). Successful removal of the LMA was regarded as absence of coughing/gagging, clenched teeth, gross purposeful movements, breath holding, laryngospasm, or desaturation to SpO2 <90%, during or immediately after removal. If LMA removal was successful, the target Ce of remifentanil for the next patient was decreased by 0.2 ng/mL. Conversely, if LMA removal was unsuccessful, the target Ce of remifentanil was increased by 0.2 ng/mL. A single measurement was obtained from each patient. The anesthesiologist who performed LMA removal and assessed "success" or "failure" was unaware of the remifentanil Ce.
Sample size was decided based on that in prior literature, which demonstrated that at least six independent pairs with successful/unsuccessful LMA removal are required for reliable estimates of the optimal remifentanil Ce when applying the modified Dixon's up-and-down method;12 thus, data from six independent pairs of patients were collected for this study.
Statistical analyses were performed using SPSS 13.0 for Windows (SPSS Inc., Chicago, IL, USA) and R for Windows (version for R 3.0.1). Data are expressed as mean±SD or median [range] or the number of patients. The EC50 of re-mifentanil Ce that enabled successful LMA removal was determined by calculating the average of the midpoint dose of all independent pairs of patients after six crossover points were obtained. For backup analysis, the data were also subjected to isotonic regression estimators for calculation of EC50, EC95, and 95% confidence interval (CI).13 An adjusted response probability was easily calculated by the pooled adjacent-violators algorithm (PAVA), and the CI was estimated by a bootstrapping approach.14 Hemodynamic changes were compared by repeated measures ANOVA. All p-values<0.05 were considered significant.
We enrolled 27 patients in this study. However, two patients were excluded because of incomplete LMA ventilation and changes in the surgery plan during anesthesia; a total of 25 patients completed the study protocol. Patient characteristics and recovery profiles are shown in Table 1 and 2.
The sequences of successful and unsuccessful LMA removal for each patient obtained by the up-and-down method are illustrated in Fig. 1. One patient with a remifentanil Ce of 1.4 ng/mL, four of five patients with a remifentanil Ce of 1.2 ng/mL, five of nine patients with a remifentanil Ce of 1.0 ng/mL, and three of seven patients with a remifentanil Ce of 0.8 ng/mL showed smooth and successful LMA removal. All three patients with a remifentanil Ce of 0.6 ng/mL failed to show smooth removal of the LMA. The required mean±SD of remifentanil Ce for smooth LMA removal after propofol anesthesia was 0.83±0.16 ng/mL according to Dixon's method. Using isotonic regression estimated from the PAVA response rate, the EC50 and EC95 of remifentanil Ce were 0.91 ng/mL (95% CI, 0.77-1.07 ng/mL) and 1.35 ng/mL (95% CI, 1.16-1.38 ng/mL), respectively.
Removal of the LMA was unsuccessful in 12 of 25 patients. Causes of unsuccessful LMA removal were coughing/gagging (five patients), teeth clenching (five patients), gross purposeful movements (six patients), and breath holding (one patient). The one patient who showed breath holding was treated easily with positive pressure ventilation with 100% oxygen. Laryngospasm and desaturation to SpO2 <90% were not observed in any of the patients.
The hemodynamic and respiratory profiles of all patients are presented in Table 3. Mean arterial pressure and HR at the end of surgery were significantly lower than those at baseline, although they returned to baseline prior to or after LMA removal. No patient had clinically significant bradycardia or hypotension.
We investigated the Ce of remifentanil for achieving smooth LMA removal at emergence from TIVA with propofol and remifentanil. Obtained via Dixon's method, a Ce of 0.83±0.16 ng/mL of remifentanil facilitated smooth LMA removal, and the estimated EC50 and EC95 values of remifentanil by isotonic regression were 0.91 ng/mL (95% CI, 0.77-1.07 ng/mL) and 1.35 ng/mL (95% CI, 1.16-1.38 ng/mL), respectively.
For smooth and safe emergence during removal of a LMA, proper depth of anesthesia is required to minimize the upper airway reflexes and to prevent adverse events of coughing, gagging, and laryngospasm. Remifentanil infused with a TCI pump during emergence can be predicted and safely maintained at a targeted Ce. During emergence, remifentanil enables easy titration of the Ce to the desired depth of anesthesia with minimal airway complications and early awakening. We focused on the depressant effects of remifentanil on upper airway and cough reflexes, and investigated a suitable concentration of remifentanil to facilitate smooth removal of LMA at emergence after TIVA. In this study, the EC95 of remifentanil TCI was 1.35 ng/mL. A recent study by Ozkan, et al.9 reported that smooth removal of LMA was possible in 86% of patients during emergence after desflurane-remifentanil anesthesia when maintaining remifentanil Ce at 1.5 ng/mL. This difference in the required concentration of remifentanil for smooth LMA removal may be related to the type of main anesthetic. Desflurane is an inhalational anesthetic with an airway irritant property and is associated with a higher incidence of airway complications, such as coughing and breath holding, at emergence from anesthesia and removal of LMAs, compared to those for sevoflurane.15,16 Propofol is known to suppress pharyngeal and laryngeal reflexes, and laryngospasm during tracheal extubation can be prevented even at subhypnotic doses of propofol.17 In addition, one study demonstrated that TIVA with propofol and remifentanil causes less coughing of lower severity during emergence, compared to sevoflurane-based balanced anesthesia.18 Further studies may be ne-eded to demonstrate the relationship between the type of an-esthetic agent and remifentanil Ce for smooth LMA removal.
Considering that irritation of the upper airway and pharynx might be greater for an endotracheal tube than an LMA,19 it is not surprising that the EC95 of remifentanil for smooth LMA removal in our study was lower than the EC95 of remifentanil for suppressing cough during tracheal extubation from balanced desflurane anesthesia. During desflurane-remifentanil anesthesia, that EC95 of remifentanil Ce for smooth removing endotracheal tube without coughing was 2.88 ng/mL.20 In contrast, smooth LMA removal was reportedly possible in 86% of the patients at a remifentanil Ce 1.5 ng/mL during emergence.9 Additionally, the EC95 of remifentanil during propofol-remifentanil anesthesia for smooth LMA removal was 1.35 ng/mL in our study and that for suppressing cough during extubation was 2.14 ng/mL.21
In our study, a mean remifentanil Ce of 1.0 ng/mL (0.6-1.4 ng/mL) was administered, and respiratory function was well preserved without apnea or desaturation during emergence. This result is in concordance with that of a previous study,9 which reported that TCI of remifentanil <1.5 ng/mL during the emergence period does not influence the level of sedation and cause respiratory depression or delayed recovery after desflurane-remifentanil anesthesia. However, the risk of hypoventilation and delayed awakening should be cautioned at a remifentanil TCI 2.0 ng/mL.22 The predicted optimal concentration of remifentanil for preventing coughing and airway reflexes during endotracheal tube extubation varies according to the type of surgery. During propofol-remifentanil TIVA, the EC50 of remifentanil Ce for suppressing cough at emergence was 1.46 ng/mL during thyroid surgery.21 In contrast, maintaining remifentanil Ce at 2.0 ng/mL prevented cough in only 54% of patients after laryngomicrosurgery.22 Although our study was limited to minor surgery, because LMA insertion is generally used in anesthesia for minor surgery, the application of our results to other types of surgeries should be considered carefully.
There are some limitations to our study. First, emergence from propofol anesthesia might be more rapid in females due to gender differences in the pharmacokinetics and pharmacodynamics of propofol.23 Our study population had a higher portion of females; therefore, this difference should be considered. Second, the incidence of smokers may have affected the remifentanil Ce. Upper airway sensitivity is increased in smokers and can theoretically affect the incidence of cough. A previous study reported that the incidence and severity of cough during emergence is significantly higher in smokers than that in non-smokers.24 However, smoking had less influence on coughing during TIVA with propofol because of the suppressive effect on the airway reflex; thus, the smoking bias could be acceptable. Third, Ces of propofol at LMA removal in this study varied in each patient: the propofol Ce at the end of surgery and at the time to achieve the predetermined remifentanil concentration after the surgery were different among patients. In addition, pharmacodynamic interactions between propofol and remifentanil could differ according to propofol concentration.25 However, since the range of propofol Ce at LMA removal in this study was small, we expect that the varying concentrations of propofol might have little clinical significance.
In conclusion, the EC50 and EC95 of remifentanil Ce for smooth removal of a LMA from propofol anesthesia were 0.91 ng/mL and 1.35 ng/mL, respectively. We showed that remifentanil TCI at an established Ce is a reliable technique for achieving safe and smooth emergence without coughing, laryngospasm, or other airway reflex movements.
Figures and Tables
Fig. 1
The responses of 25 patients to laryngeal mask airway removal and the remifentanil concentration. Arrows represent the midpoint doses of all independent pairs of patients involving a crossover (i.e., success to failure). The remifentanil concentration required for smooth removal in 50% of the patients was 0.83±0.16 ng/mL.
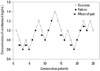
Table 1
Patient Characteristics
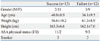
| Success (n=13) | Failure (n=12) | |
|---|---|---|
| Gender (M/F) | 2/11 | 3/9 |
| Age (yrs) | 40.8±8.9 | 36.1±9.5 |
| Weight (kg) | 56.6±10.2 | 61.3±8.9 |
| Height (cm) | 163.3±6.6 | 162.1±7.0 |
| ASA physical status (I/II) | 11/2 | 9/3 |
| Smoker | 3 | 3 |
Table 2
Anesthesia and Recovery Profiles

Table 3
Hemodynamic Profiles and Bispectral Indices (BIS) during Laryngeal Mask Airway (LMA) Removal

References
1. Gataure PS, Latto IP, Rust S. Complications associated with removal of the laryngeal mask airway: a comparison of removal in deeply anaesthetised versus awake patients. Can J Anaesth. 1995; 42:1113–1116.

2. Pappas AL, Sukhani R, Lurie J, Pawlowski J, Sawicki K, Corsino A. Severity of airway hyperreactivity associated with laryngeal mask airway removal: correlation with volatile anesthetic choice and depth of anesthesia. J Clin Anesth. 2001; 13:498–503.

3. Cameron AJ, Sellers WF. Early vs late LMA removal; risks to patients and damage to equipment. Anaesth Intensive Care. 2001; 29:80–81.
4. Nunez J, Hughes J, Wareham K, Asai T. Timing of removal of the laryngeal mask airway. Anaesthesia. 1998; 53:126–130.

5. Baird MB, Mayor AH, Goodwin AP. Removal of the laryngeal mask airway: factors affecting the incidence of post-operative adverse respiratory events in 300 patients. Eur J Anaesthesiol. 1999; 16:251–256.

6. Aouad MT, Al-Alami AA, Nasr VG, Souki FG, Zbeidy RA, Siddik-Sayyid SM. The effect of low-dose remifentanil on responses to the endotracheal tube during emergence from general anesthesia. Anesth Analg. 2009; 108:1157–1160.

7. Chen J, Li W, Wang D, Hu X. The effect of remifentanil on cough suppression after endoscopic sinus surgery: a randomized study. Acta Anaesthesiol Scand. 2010; 54:1197–1203.

8. Nho JS, Lee SY, Kang JM, Kim MC, Choi YK, Shin OY, et al. Effects of maintaining a remifentanil infusion on the recovery profiles during emergence from anaesthesia and tracheal extubation. Br J Anaesth. 2009; 103:817–821.

9. Ozkan D, Ergil J, Alptekin A, Aktürk N, Gümüs H. Target controlled remifentanil infusion for smooth laryngeal mask airway removal during emergence from desflurane-remifentanil anesthesia. J Anesth. 2012; 26:369–374.

10. Marsh B, White M, Morton N, Kenny GN. Pharmacokinetic model driven infusion of propofol in children. Br J Anaesth. 1991; 67:41–48.

11. Minto CF, Schnider TW, Egan TD, Youngs E, Lemmens HJ, Gambus PL, et al. Influence of age and gender on the pharmacokinetics and pharmacodynamics of remifentanil. I. Model development. Anesthesiology. 1997; 86:10–23.

13. Stylianou M, Flournoy N. Dose finding using the biased coin up-and-down design and isotonic regression. Biometrics. 2002; 58:171–177.

14. Pace NL, Stylianou MP. Advances in and limitations of up-and-down methodology: a précis of clinical use, study design, and dose estimation in anesthesia research. Anesthesiology. 2007; 107:144–152.
15. Arain SR, Shankar H, Ebert TJ. Desflurane enhances reactivity during the use of the laryngeal mask airway. Anesthesiology. 2005; 103:495–499.

16. White PF, Tang J, Wender RH, Yumul R, Stokes OJ, Sloninsky A, et al. Desflurane versus sevoflurane for maintenance of outpatient anesthesia: the effect on early versus late recovery and perioperative coughing. Anesth Analg. 2009; 109:387–393.

17. Batra YK, Ivanova M, Ali SS, Shamsah M, Al Qattan AR, Belani KG. The efficacy of a subhypnotic dose of propofol in preventing laryngospasm following tonsillectomy and adenoidectomy in children. Paediatr Anaesth. 2005; 15:1094–1097.

18. Hohlrieder M, Tiefenthaler W, Klaus H, Gabl M, Kavakebi P, Keller C, et al. Effect of total intravenous anaesthesia and balanced anaesthesia on the frequency of coughing during emergence from the anaesthesia. Br J Anaesth. 2007; 99:587–591.

19. Abdi W, Amathieu R, Adhoum A, Poncelet C, Slavov V, Kamoun W, et al. Sparing the larynx during gynecological laparoscopy: a randomized trial comparing the LMA Supreme and the ETT. Acta Anaesthesiol Scand. 2010; 54:141–146.

20. Cho HB, Kim JY, Kim DH, Kim DW, Chae YJ. Comparison of the optimal effect-site concentrations of remifentanil for preventing cough during emergence from desflurane or sevoflurane anaesthesia. J Int Med Res. 2012; 40:174–183.

21. Lee B, Lee JR, Na S. Targeting smooth emergence: the effect site concentration of remifentanil for preventing cough during emergence during propofol-remifentanil anaesthesia for thyroid surgery. Br J Anaesth. 2009; 102:775–778.

22. Chang CH, Lee JW, Choi JR, Shim YH. Effect-site concentration of remifentanil to prevent cough after laryngomicrosurgery. Laryngoscope. 2013; 123:3105–3109.

23. Hoymork SC, Raeder J. Why do women wake up faster than men from propofol anaesthesia? Br J Anaesth. 2005; 95:627–633.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download