Abstract
Purpose
The aim of this study was to evaluate the cost-effectiveness of the use of drug-eluting stents (DESs), as compared with bare-metal stents (BMSs) in Korea.
Materials and Methods
A retrospective cohort study was conducted between January 2000 and December 2007. Subjects were stent-treated for the first time between 2004 and 2005, with four years of follow-up (2004-2007) (n=43674). The incremental cost-effectiveness ratio (ICER) was used to calculate the costs of DESs compared with BMSs among patients with coronary artery disease (CAD). Cost-effectiveness was assessed with effectiveness defined as a reduction in major adverse cardiac events after six months and after one, two, three, and four years.
Results
The total costs of a DESs were 674108 Korean won (KRW) higher than that of a BMSs at the end of the follow-up; 13635 thousand KRW per patient treated with DESs and 12960 thousand KRW per patient treated with BMSs. The ICER was 256315 per KRW/death avoided and 293090 per KRW/re-stenting avoided among the CAD patients at the end of the follow-up.
Stent implantation is the most effective successful treatment method for coronary artery disease (CAD) in Korea. It is used in more than 80% of patients.1 However, the implantation of bare-metal stents (BMSs) is associated with major side-effects, including in-stent restenosis and stent thrombosis.2 Drug-eluting stents (DESs) were developed to overcome these side-effects, but its cost effectiveness is unclear yet.
The demand for health care is constantly increasing like the aging of population and the development of medical technology, but the available budget is limited. The health economic evaluation is a tool to compare health outcomes and costs under limited resources. Government agencies in a variety of healthcare related data are used as the basis for policy decisions. In South Korea, the recent health care expenditure has actively progressed in relation to such rationalization or pharmaceutical policy for the economic evaluation of pharmaceuticals and medical technology.
The average benefit fee paid by the National Health Insurance (NHI) in 2007 for DESs was 1996000 Korean won (KRW) and 1647000 KRW for BMS per stent. DESs are about 21.2% more expensive than BMSs. In 2007, medical devices were classified into 1440 divisions in Korea. DESs cost the Ministry of Health, Welfare and Family Affairs (MOHW) 113 billion KRW in 2007, which are 10.5% of the total expenditure for medical devices among the total medical device claim amount. In contrast, the reimbursement costs for BMSs were 5.1 billion KRW in 2007, which are only 0.5% of the total expenditure for medical devices.
According to the study results published world-wide so far,2,3,4,5 DESs are associated with a decreased incidence of coronary in-stent restenosis and major adverse cardiac events (MACE); however, in-stent restenosis and stent thrombosis remain critical problems in patients treated with DESs.6
Presently, a world-wide randomized clinical trial is in progress to compare the economic value of DES- and BMS-based treatments for CAD. However, the economic evaluation results comparing the two types of stents vary between countries because of the nature of their health insurance policies. Therefore, these economic evaluation results may not be applicable to Korea.
The objective of this study was to compare the economic value of DESs and BMSs in the treatment of CAD using all stent-treated patients registered in the Korean NHI Database.
We referenced two databases from January 2000 to December 2007: the NHI Claims Database of the Health Insurance Review & Assessment Service (HIRA), which includes medical claims that are filed by medical institutions through the NHI and compiled and referenced through the Electronic Data Interchange (EDI) and the National Death Index.
Since the social insurance for health care started 1977 in Korea, the NHI program is applied for all but 3.5% of public assistance in the Korean population. The social insurance for health care is single insurer. The NHI program uses a fee-for-service system to reimburse health care providers and the MOHW regulates the fees.7,8
The study subjects (30 years of age or older as of 2005) were selected based on the following criteria: received treatment for CAD with stent implantation for the first time [International Classification of Disease (ICD) codes I20, I21, I22, I23, I24, and I25] between 2004 and 2005 (43674 patients; DES-treated n=34229, BMS-treated n=9445). Patients who had previously received a stent implant within four years of this time were excluded from the study. Subgroup analyses were carried out for patients with myocardial infarction (MI) (18256 patients; DES-treated n=13761, BMS-treated n=4459).
The stent types used in the study were divided in BMSs and DESs. DESs were divided into paclitaxel-, sirolimus-, everolimus- and zotrolimus-eluting stents; however, DESs included only paclitaxel- and sirolimus-eluting stents, because everolimus- and zotrolimus-eluting stents were listed since 2006.
Comorbidity was predicted using the age-adjusted Charlson Comorbidity Index (ACCI). The Charlson Comorbidity Index (CCI) is based on disease severity; it predicts the one-year mortality for a patient who may have a range of comorbid conditions (a total of 17 conditions). Each condition is assigned a score of 1 to 6 depending on the risk of dying associated with that condition. In this study, clinical data collected during the first year prior to stent implantation were used as criteria. Weights were assigned to 17 predetermined clinical conditions (adapted from the ICD-10 codes of Sundararajan, et al.9) and summed; one point for every additional ten years of age was added to the score for patients over 50 because of the increased risk of developing CAD in older subjects. A final ACCI score was obtained from the age-adjusted sum.10 The ACCI score was assessed at three levels: 0-2 points, low-risk patients; 3-4 points, medium-risk patients; and ≥5 points, high-risk patients.
The costs per patient were calculated as the initial procedural costs and all follow-up medical care costs. The initial procedural costs included all initial hospitalization and medical device costs accrued during stent treatment. The follow-up costs were calculated as the sum of medical resources used for four years after discharge (i.e., through December of 2007); this included such costs as outpatient visits, medical expenses, and hospitalization costs for re-stenting during the follow-up period. The total costs per patient were the sum of the initial procedural costs and follow-up medical care costs; pharmaceutical costs were not included because drugs used to treat CAD are difficult to determine. Moreover, follow-up costs were analyzed on a per annum basis. Total costs were estimated over a six-month, one-year, two-year, three-year, and four-year follow-up period. When subjects were re-implanted with stents two or more times during follow-up, only the costs of the initial stent were applied. All costs are expressed in Korean currency.
The composite clinical end-point of the study was surgical re-stenting or death at six-month, one-year, two-year, three-year, and four-year. The re-stenting rate was defined as the proportion of patients who had stents re-implanted. The morbidity was defined as the proportion of patients who died from all causes among first-time stent-treated patients.
The major economic value of DESs is the result of a decreased death rate and reduced expenses. The incremental cost effectiveness ratio (ICER; calculated by dividing the difference in mean medical care costs by the difference in the death rate or re-stenting between the DESs and BMSs groups) was used to calculate the extra costs of DESs implantation when the death rates and re-stenting rates were reduced to 1%.
The remaining quadrants represent situations where the evaluated strategy is more expensive and less effective (dominated; upper left quadrant) or less expensive and more effective (dominant; lower right quadrant).
Discrete data are reported as frequencies, while continuous data are reported as mean±SD. Discrete variables were compared using chi-square tests. Independent Student's t-tests were used to compare costs between the DESs and BMSs groups. Differences between the event-free survival curves for the two groups were compared using Wilcoxon signed- and log-rank tests.
All statistical analyses were performed using Statistical Analysis System (SAS) version 9.1 (SAS Institute Inc., Cary, NC, USA).
All baseline characteristics are presented in Table 1. Three times more DESs were implanted in the CAD and MI populations than BMSs. Females were more likely to receive a DESs than males and the DESs implantation rate increased with age. DESs implantation was preferred in high-risk patients and diabetics. The average initial procedural costs for CAD patients were 6653000±2344000 KRW compared to 7185000±2725000 KRW for MI patients. Initial procedural costs for the CAD patients were 911000 KRW higher per patient for the DES group versus the BMS group compared to 973000 KRW higher in the MI group.
The cumulative survival rate for the patients with DESs and BMSs implantation decreased in the CAD and MI populations during follow-up (Fig. 1A and B). Patients were classified as low- or high-risk patients in both populations. The cumulative survival rate was not significantly different for the low-risk CAD and MI patients implanted with BMSs and DESs; however, the cumulative survival rate for patients in the high-risk group implanted with DESs was significantly higher (p<0.001) compared to that of patients implanted with BMSs (Fig. 1C and D).
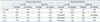
The cumulative re-stenting rate was lower for patients with DESs than with BMSs in the low-risk CAD and MI populations. However, the cumulative re-stenting rate was higher for patients in the high-risk group implanted with DESs compared to that for patients implanted with BMSs in MI populations (p<0.001) (Fig. 2).
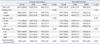
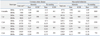
Table 2 and 3 summarize the estimated differences in costs and effectiveness of DESs compared with BMSs at six months, one year, two years, three years, and four years after initial stent treatment. The ICER was calculated using an ACCI-adjusted value for both the CAD and MI groups based on the costs and results for the low- and high-risk patients.
In the CAD population, the mean total medical costs per patient during the six-month follow-up period were 693950 KRW higher in the DESs group compared with the BMSs group. The ICER was 387682 KRW/death avoided and 660905 KRW/re-stenting avoided. The ICER was 256315 KRW/death avoided and 293090 KRW/re-stenting avoided after four years of follow-up. The ICER increased for the first two years of follow-up and then decreased afterward until the end of the fourth year.
In the MI group, the mean total medical costs for the DESs patients were 897831 KRW higher than in the BMSs group during the six-month follow-up period. The ICER was 342684 KRW/death avoided and 1068846 KRW/re-stenting avoided. After four years of follow-up, the ICER was 508574 KRW/death avoided and 732748 KRW/re-stenting avoided. The ICER increased for the first three years of follow-up and then decreased.
The ICER was similar for the low- and high-risk patients among the CAD patients. The ICER tended to be lower in the high-risk patients compared to the low-risk patients.
For MI patients, the ICER for the low-risk patients was 1420955 KRW/death avoided after one year of follow-up. DESs became cost-effective after two years of follow-up. Further, the use of DESs not only proved to be cost-effective but also showed its evidence of cost-saving among the high-risk patients after four years of follow-up.
Data in this study were obtained from an analysis of the costs and effectiveness of initial stent treatments and four years of follow-ups in first-time stent-treated patients in Korea. The study was designed based on the assumption that the rates of mortality and re-stenting associated with DESs treatment would be lower than those associated with BMSs, but that the costs of DESs would be higher than that of BMSs. The specific objectives of this study were to calculate the difference in the ICER between DESs and BMSs treatment.
More than 80% of CAD patients undergo DESs implantation; the use of DESs is more common than that of BMSs in the United States.2 Randomized clinical trials indicate that DESs compared with BMSs have decreased the clinical side-effects associated with stent treatment by reducing stent thrombosis, in-stent restenosis, target lesion revascularization and MACE. However, despite this improved clinical efficacy, in-stent restenosis still occurs in 15-30% of DESs patients.2,11,12,13,14,15
Presently, global randomized clinical trials are being used to compare the incremental costs of treatment with the clinical effectiveness of DESs and BMSs in CAD patients. These trials include the EXCELLA First-in-Man (FIM),16 REALITY,14 Sirolimus-Eluting Balloon Expandable Stent in the Treatment of Patients With De Novo Native Coronary Artery Lesions (SIRIUS),15 RAVEL (randomised study with the sirolimus eluting Bx Velocity balloon expandable stent in the treatment of patients with de novo native coronary artery lesions),17 TAXUS-IV (Treatment of De Novo Coronary Disease Using a Single Paclitaxel-Eluting Stent) trial,18 and Basel Stent Kosten Effektivitäts Trial (BASKET) trials.4,5
The RAVEL study compared DESs treatment with BMS treatment in patients with angina pectoris at 19 medical centers. During a follow-up period of one year, the overall rate of major cardiac events was 5.8% in the DESs group and 28.8% in the BMSs group.17
In the SIRIUS trial, repeated revascularization procedures were needed in 13.7% of DESs patients and 28.4% of BMSs patients, indicating that DESs are more effective for preventing in-stent restenosis. The repeat revascularization rate was reduced by 52% in the DESs group compared with the BMSs group. Moreover, DESs treatment was associated with substantial reductions in various morbid events, including re-hospitalization, repeat percutaneous coronary intervention, and bypass surgery over a follow-up period of one year.15
A recent hierarchical Bayesian meta-analysis of randomized clinical trials involving DESs, showed based on 11 trials with 5103 patients, decreased incidences of MACE through DESs from 16.4% (BMSs) to 7.8% (DESs), mainly by reducing the rate of target vessel revascularization (TVR), but not by reducing the rate of MI or death.2
The randomized BASKET real-world study showed a 44% (OR 0.56, 95% CI 0.35-0.91) reduction in the rate of MACE comparing the use of DESs with BMSs over a follow-up period of six months. However, there was no statistically significant difference in cardiac death or acute MI between the stent groups.4 Their results at 18 months indicated a higher death rate in patients with a DESs. Among high-risk patients, the use of DESs was associated with reduced rates of MACE, death/MI (9% vs. 15%) and non-MI TVR. However, the rates of MACE and death/MI were increased (9% vs. 5%) among low-risk DESs patients.5
In this study, the cumulative death and re-stenting rates per 100 patients were respectively reduced by 20.4% and 16.7% in the DESs groups compared to the BMSs groups over a period of four years following initial treatment. The longer the follow-up period, the larger the difference in the death- and re-stenting rates between the DESs and BMSs patients (p<0.05). The reduction in the death and re-stenting rates among the high-risk patients reached a greater level of significance than in the low-risk group (p<0.05).
The death and re-stenting rates showed a significant improvement for the DESs patients in the MI group; DESs appeared to be clinically effective and stable in these patients. However, the efficacy of DESs treatment in MI patients is controversial.
The death rate in our study was similar to that in other accepted medical intervention studies. The re-stenting rate in our DESs patients was slightly lower than in other studies, while the re-stenting rate in our BMSs patients was a great deal lower than in other studies probably because of variations in the re-stenting criteria. However, the re-stenting and death rates in our study were in accordance with those from other randomized clinical trials, indicating that death and re-stenting in patients treated with DESs are less common compared to patients treated with BMSs, regardless of differences in geographical region or the received quality of health care.
There is a large difference in the costs between DESs and BMSs. In the US, the costs of DESs and BMSs are $2700-2900 and $800-900 per stent, respectively; DESs is three times as expensive as BMSs.15,18 In Korea, DESs is about 21.2% more expensive than BMSs. We propose the ICER for these stents might be different from that in other countries as a result of the higher cost of BMSs and the lower cost of DESs in Korea.
The ICER for CAD patients was 387682 KRW associated with a 1% avoided death rate after six months of follow-up. It was 256315 KRW after four years of follow-up. The ICER was the highest after two years of follow-up and was decreased after the third and the fourth year of follow-up. The ICER associated with a 1% re-stenting rate was 660905 KRW after six months of follow-up and 293090 KRW after four years of follow-up. The ICER was lower after four years of follow-up than that after six months of follow-up.
In the MI patients, the ICER associated with a 1% avoided death rate was 342684 KRW after six months of follow-up and 508574 KRW after four years. The ICER associated with a 1% avoided re-stenting rate was 1068846 KRW after six months of follow-up and 732748 KRW after four years. The ICER's were relatively higher for the MI patients than those for the CAD patients.
In the BASKET trial, the average ICER was €64732, preventing 1% of MACE per patient after 18 months of follow-up. It was 3.5 times higher than that calculated after six months of follow-up.5 Those results were in conflict with our study results. In the SIRIUS trial, repeated revascularization procedures were reduced by 52% in DESs patients compared with the BMS group; aggregated one-year follow-up costs were $309 higher per patient for DESs and an ICER of $1650 was calculated per avoided repeat revascularization event.15
In the TAXUS-IV trial, aggregated one-year medical care costs were $572 higher per patient in the DESs group and 12.2 fewer TVR events were performed per 100 patients during follow-up. The result was a disease-specific ICER of $4678 per TVR avoided.18
In conclusion, in this study, we found that DESs are clinically more useful for CAD and MI patients than BMSs. Moreover, DESs are cost-effective in Korea.
All patients included in this study were identified using the Korean NHI Claims Database; however, this database has several limitations.
First, the confirmation of a previous stent was impossible in some patients. The NHI Claims Database began operating in 2000; thus, patients who were stent-treated before 2000 but had implanted revascularizations between 2004 and 2005 were not excluded from the study.
Second, the stent site could not be confirmed. Therefore, it was unclear whether revascularization was at the same site as in-stent restenosis in some patients; consequently, the re-stenting rate could have been overestimated.
Third, death rates were calculated in all-cause mortality. This study cannot take advantage of cause of death statistics of Statistics Korea and the principle diagnosis of the National Death Index cannot determine the exact cause of death.
Fourth, our analysis was incapable of accurately reflecting the specific severity of heart disease. We used comorbidity which influences treatment and follow-up medical costs as a measure of disease severity. In this analysis, we used an age-adjusted CCI to adjust the severity. Nevertheless, it was impossible to accurately measure the specific severity of heart disease in our patients.
Finally, the study was limited in consideration of costs. The total medical costs were used to assess the annual follow-up medical costs for the stent-treated patients; however, our calculation did not include associated pharmaceutical costs and non-medical costs such as transportation and nursing.
Nevertheless, the results of this study are important, reflecting information obtained from the Korean NHI Claims Database. In contrast to previous studies that sampled data from selected hospitals have our results a country-wide perspective.
Despite the limitations of the Korean NHI Claims Database, this study provides an important economic evaluation of a medical device. Our data provide essential information for fee-setting and the economics of the national health insurance system.
Our analysis was carried out from the perspective of the health insurance system. We performed an economic evaluation using EDI data from the HIRA for the past eight years. In societal perspective, we did not complete the costs and the results obtained, it can identify that our analysis was performed as important evidence. Our data are also beneficial to society as they provide a resource-based, relative-value scale for the use of stents in Korea.
Figures and Tables
Fig. 1
Cumulative survival rate in patients with drug-eluting stents and bare-metal stents. (A) Coronary artery disease patients. (B) Myocardial infarction patients. (C) Low-risk and high-risk coronary artery disease patients. (D) Low-risk and high-risk myocardial infarction patients. DES, drug-eluting stent; BMS, bare-metal stent; CAD, coronary artery disease; MI, myocardial infarction.
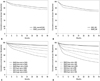
Fig. 2
Cumulative re-stenting rate in patients with drug-eluting stents and bare-metal stents. (A) Coronary artery disease patients. (B) Myocardial infarction patients. (C) Low-risk and high-risk coronary artery disease patients. (D) Low-risk and high-risk myocardial infarction patients (***p<0.001). DES, drug-eluting stent; BMS, bare-metal stent; CAD, coronary artery disease; MI, myocardial infarction.

ACKNOWLEDGEMENTS
This research was supported by Health Insurance Review & Assessment Service (No. D94-2009-18).
References
1. Cho JS, Jeong MH, Jeong SY, Choi MJ, Chung JW, Hwang SH, et al. Predictive factor of the third coronary stent restenosis. Korean J Med. 2005; 69:255–263.
2. Babapulle MN, Joseph L, Bélisle P, Brophy JM, Eisenberg MJ. A hierarchical Bayesian meta-analysis of randomised clinical trials of drug-eluting stents. Lancet. 2004; 364:583–591.

3. Jeong MH, Kim SH, Ahn YK, Cho JG, Park JC, Na KJ, et al. Predictive factors for the second restenosis after coronary interventions. Catheter Cardiovasc Interv. 2000; 50:34–39.

4. Kaiser C, Brunner-La Rocca HP, Buser PT, Bonetti PO, Osswald S, Linka A, et al. Incremental cost-effectiveness of drug-eluting stents compared with a third-generation bare-metal stent in a real-world setting: randomised Basel Stent Kosten Effektivitäts Trial (BASKET). Lancet. 2005; 366:921–929.

5. Brunner-La Rocca HP, Kaiser C, Bernheim A, Zellweger MJ, Jeger R, Buser PT, et al. Cost-effectiveness of drug-eluting stents in patients at high or low risk of major cardiac events in the Basel Stent KostenEffektivitäts Trial (BASKET): an 18-month analysis. Lancet. 2007; 370:1552–1559.

6. Stone GW, Grines CL, Cox DA, Garcia E, Tcheng JE, Griffin JJ, et al. Comparison of angioplasty with stenting, with or without abciximab, in acute myocardial infarction. N Engl J Med. 2002; 346:957–966.

7. Kwon S. Payment system reform for health care providers in Korea. Health Policy Plan. 2003; 18:84–92.

8. Lee K, Lee S. Effects of the DRG-based prospective payment system operated by the voluntarily participating providers on the cesarean section rates in Korea. Health Policy. 2007; 81:300–308.

9. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004; 57:1288–1294.

10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987; 40:373–383.

11. Serruys PW, de Jaegere P, Kiemeneij F, Macaya C, Rutsch W, Heyndrickx G, et al. A comparison of balloon-expandable-stent implantation with balloon angioplasty in patients with coronary artery disease. Benestent Study Group. N Engl J Med. 1994; 331:489–495.

12. Fischman DL, Leon MB, Baim DS, Schatz RA, Savage MP, Penn I, et al. A randomized comparison of coronary-stent placement and balloon angioplasty in the treatment of coronary artery disease. Stent Restenosis Study Investigators. N Engl J Med. 1994; 331:496–501.

13. Hoffmann R, Mintz GS. Coronary in-stent restenosis-predictors, treatment and prevention. Eur Heart J. 2000; 21:1739–1749.

14. Morice MC, Colombo A, Meier B, Serruys P, Tamburino C, Guagliumi G, et al. Sirolimus- vs paclitaxel-eluting stents in de novo coronary artery lesions: the REALITY trial: a randomized controlled trial. JAMA. 2006; 295:895–904.

15. Cohen DJ, Bakhai A, Shi C, Githiora L, Lavelle T, Berezin RH, et al. Cost-effectiveness of sirolimus-eluting stents for treatment of complex coronary stenoses: results from the Sirolimus-Eluting Balloon Expandable Stent in the Treatment of Patients With De Novo Native Coronary Artery Lesions (SIRIUS) trial. Circulation. 2004; 110:508–514.

16. Costa JR Jr, Abizaid A, Feres F, Costa R, Seixas AC, Maia F, et al. EXCELLA First-in-Man (FIM) study: safety and efficacy of novolimus-eluting stent in de novo coronary lesions. EuroIntervention. 2008; 4:53–58.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download