Abstract
Purpose
This study investigated whether hormones and pain perception are associated with exam anxiety, and also whether exam anxiety is affected by seasonal differences in testosterone and cortisol levels.
Materials and Methods
Forty-six healthy males were recruited from a medical college. Anxiety was induced by having participants perform the Objective Structured Clinical Examination. Pressure was applied to the participants to induce pain. Pain thresholds, pain ratings, anxiety ratings, blood pressure, heart rate, salivary testosterone and cortisol levels were measured under resting and anxiety conditions in the spring and summer. Data were collected from 46 participants during the spring (n=25) and summer (n=21).
Results
Pain thresholds and testosterone levels were significantly lower under anxiety than at rest for all participants (n=46), while cortisol levels, pain ratings, and anxiety ratings were significantly higher under anxiety than at rest. In the spring (n=25), testosterone levels were significantly higher at rest than under anxiety, while there was no difference in cortisol levels between resting and anxiety conditions. In the summer (n=21), cortisol levels were significantly higher under anxiety than at rest, while there was no difference in testosterone levels between resting and anxiety conditions. There were no significant seasonal differences in pain and anxiety ratings and pain threshold.
Conclusion
These results indicate that seasonal differences in testosterone and cortisol levels under anxiety and at rest may affect pain responses. These results also suggest that acute clinical pain may be relieved by managing anxiety that is related to a decrease of testosterone in spring and a large increase of cortisol in summer.
Examination anxiety activates the sympathetic nervous system (SNS) and hypothalamic pituitary adrenal (HPA) axis. Previous studies have shown that examination stress increases anxiety, salivary cortisol levels and blood pressure,1,2 and that psychological stress increases the activity of the HPA axis with a subsequent rise in salivary cortisol levels.3 Some studies have indicated that higher stress ratings during exams are associated with higher salivary cortisol levels, and that students who report higher stress and have higher cortisol levels before the examination also tend to have significantly lower examination scores.2,4
Furthermore, anticipatory stress decreases mean testosterone levels.5 Human serum testosterone levels are lowered during psychological and physical stress, as well during the acute stress of surgery.6 Men with low testosterone levels tend to be more irritable and anxious than men with normal testosterone levels.7 Animal studies have also reported that testosterone has analgesic and anti-anxiety effects8 and modulates opioid analgesia.9
Understanding seasonal variations in hormones is important when evaluating the effects of hormones on pain responses. Seasonal variations in testosterone production in various non-human species are known to affect behavior, cognition, fertility, and morphology.10 Approximately 70% of non-human species seasonally regulate glucocorticoid concentrations and approximately 80% of those species show a peak during breeding.11 In addition to seasonal variations of basal glucocorticoid in animals, recent evidence indicates that the magnitude of stress-induced glucocorticoid concentrations varies seasonally.11,12
Studies on seasonal variation of hormones in humans, however, have shown inconsistent results. Most studies have found circannual variations in male testosterone levels,13-23 although some have not.24-29 In humans, few studies have examined seasonal variations in salivary cortisol concentration: higher cortisol concentrations have been observed during the summer and puberty,30 while one study failed to show a seasonal variation of cortisol.31
It is generally accepted that the induction of fear decreases sensitivity to pain, whereas the induction of anxiety may increase sensitivity to pain.32-35 Extant evidence suggests that testosterone and cortisol levels are altered by stress and anxiety;2-6 however, whether exam anxiety and pain perception are affected by seasonal differences in testosterone and cortisol levels remains unclear. Therefore, we hypothesized that seasonal differences in testosterone and cortisol levels would affect pain responses to pressure stimuli at rest and under anxiety. Hormonal changes and pain responses at rest and under anxiety were compared in a total of 46 participants without considering season; then, hormonal changes and pain responses at rest and under anxiety were compared in the spring and summer.
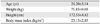
Forty-six healthy Korean male medical students were recruited for this study (Table 1). They voluntarily participated in this experiment, which was held in the polyclinic of the Department of Anesthesiology and Pain Medicine at Yonsei University Wonju College of Medicine. All volunteers provided written, informed consent acknowledging that 1) they would experience experimental pressure pain; 2) no tissue damage would result from this stimulation; 3) all of the methods and procedures were clearly explained; and 4) they were free to withdraw from the experiment at any time. Participants with metabolic diseases or any other significant clinical conditions which could influence the hypothalamic-pituitary-gonadal (HPG) and HPA axes were excluded from the study. The Medical Ethics Committee of Yonsei University, Wonju College of Medicine approved this study.
The methods of this pressure pain study were similar to those in a previously reported study on electrical pain.36 After publishing electrical pain data during Objective Structured Clinical Examination (OSCE),36 the pressure pain data were analyzed according to season. The OSCE was completed from 27 April 2011 to 12 August 2011 at the Department of Anesthesiology and Pain Medicine of Yonsei University Wonju College of Medicine. The OSCE uses a human anatomy model (dummy) for three basic medical anesthetic technique tests: Test #1, intubation; Test #2, venipuncture; and Test #3, local anesthesia. The pain experiments were conducted twice, during a period of rest two days before the OSCE and under anxiety on the day of OSCE. The experiment conducted while the participant was under OSCE was carried out during a break between the venipuncture practice and the local anesthesia practice tests. The OSCE is considered to be a very stressful exam for medical licensure in Korea. Therefore, anxiety was induced by making participants to perform the OSCE.
Participants sat in a chair and placed their left hand comfortably on their thigh. After saliva samples were collected, participants were asked to rate their anxiety before the pressure pain application both at rest and under OSCE. Before pressure was applied at rest and under OSCE, blood pressure and heart rate were measured using an automatic sphygmomanometer on the arm. Pressure pain was induced experimentally using the tourniquet technique. A 12-cm-wide mercury sphygmomanometer cuff (CK-101, Spirit Medical Co., Ltd., New Taipei, Taiwan) was placed tightly around the wrist. Pressure was applied to participants equally at rest and under OSCE to induce pain. The cuff was inflated to a pressure of 300 mm Hg in a step-by-step fashion at a rate of approximately 10 mm Hg/sec until the participant first reported pain. The pain threshold was defined as the lowest pressure at which the participants reported pain. After the pain threshold was reached, the pressure was increased to 300 mm Hg and maintained for 15 sec. Participants were then asked to rate their degree of pain. If the participants reported feeling intolerable pain at a given pressure before reaching 300 mm Hg, the pressure was not increased further. Ratings were assessed using the numerical rating scale ranging from 0 to 100 (0=no pain and anxiety; 100=maximum imaginable pain and anxiety). A pressure of 300 mm Hg is the level of pressure routinely used in an orthopedic surgery procedure in order to arrest hemorrhage. In fact, that level of pressure may be applied for longer durations in a clinical setting, but 15 sec at 300 mm Hg pressure was the maximum applied pressure in this experiment in order to ensure participant safety.
Saliva samples were used to evaluate the activity of the HPA and hypothalamic pituitary gonadal (HPG) axes because saliva sampling is noninvasive and has been previously validated for measurement of bioactive steroid hormones.37-39 Saliva samples were collected in the afternoon (14:30-16:30) before applying pain stimuli on both rest and anxiety days. On anxiety days, saliva samples were collected between the venipuncture and local anesthesia tests. A saliva sample was collected once for each participant under each condition. Four to five participants per week took part in this experiment, according to the polyclinic schedule. In order to minimize the effects of diurnal variations, saliva samples were collected within the same time period for both resting and anxiety conditions. In order to avoid the possibility of contamination, participants were instructed to avoid eating, drinking, chewing gum or brushing their teeth for one hour prior to sampling. Passive drool was used because it is cost-effective and approved for use with almost all analytes. Participants rinsed with water 10 minutes prior to collection. With head tilted forward, participants drooled down the straw and saliva was collected in a cryovial. After the samples were collected, they were kept in a deep freezer overnight or longer as needed.
The samples were thawed and spun at 3000 rpm for 5 minutes to obtain a clear, watery supernatant with low viscosity for salivary cortisol and testosterone analysis (GunSei Biotec, Inc., Gwanak-gu, Seoul, Korea). Then, 100 uL of saliva was removed for duplicate analysis of cortisol levels using a commercial kit (DRG instruments GmbH, Marburg, Germany). The lower detection limit of the assay was 0.1 ng/mL with inter-assay and intra-assay coefficients of variance of <5% across the expected range of cortisol levels. In addition, 100 uL of saliva was used for duplicate analysis of testosterone levels using a commercial kit (IBL-America, Minneapolis, MN, USA). The lower detection limit of the assay was 10 pg/mL. Intra-assay coefficients of variation for salivary testosterone were between 2.2 and 5.2%, while inter-assay coefficients of variation for salivary testosterone were between 3.2 and 9.6%.
The experiment was conducted in Wonju, South Korea at an elevation of approximately 150 meters. Data were collected from 46 participants during the spring (n=25) or summer (n=21). Mean temperature and humidity in the spring (27 April-2 June 2011) in Wonju are 18.3℃ and 56%, respectively. Mean temperature and humidity in the summer (29 June-12 August 2011) in Wonju are 25.7℃ and 77.8%, respectively.
Data from all 46 participants were analyzed together, and then grouped by season. Grouped data were analyzed using the paired-samples t-test and independent samples t-test with PASW (Predictive Analytics Software) Statistics version 20 (SPSS Inc., Chicago, IL, USA). Using repeated measures analysis of variance, the interaction between seasonal effects (spring and summer) and conditional effects (resting and anxiety conditions) was investigated. A p value of less than 0.05 was considered significant.
All 46 participants completed the pain trial up to 300 mm Hg pressure under resting and anxiety conditions. None of the participants felt intolerable pain before reaching the maximum 300 mm Hg in both conditions. Therefore, data from all 46 participants were used in the analyses.
In all 46 participants sampled during the spring (n=25) or summer (n=21), testosterone levels, pain thresholds, and testosterone/cortisol ratio were significantly lower under anxiety than at rest. Pain ratings, anxiety ratings, cortisol levels, systolic blood pressure (SBP) and heart rate were significantly higher under anxiety than at rest (Table 2). Differences in SBP between anxiety and resting conditions were significantly positively correlated with differences in pain ratings between anxiety and resting conditions (r=0.397, p=0.006, n=46) (Fig. 1). In other words, when there were large differences in SBP between anxiety and resting conditions, there were also large differences in pain ratings between these two conditions.
In the 25 participants sampled during the spring, testosterone levels were significantly lower under anxiety than at rest (p=0.005), but there was no significant difference in cortisol levels at rest vs. under anxiety (p=0.689) (Table 3). Pain thresholds and pain and anxiety ratings did not vary significantly by season.
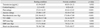
In the 21 participants sampled during the summer, there was no significant difference in testosterone levels between anxiety and resting conditions (p=0.428), but cortisol levels were significantly lower at rest than under anxiety (p=0.006) (Table 4). As mentioned above, pain thresholds and pain and anxiety ratings did not vary significantly by season.
Testosterone level differences between anxiety and resting conditions in the spring were significantly higher than those in the summer (Table 5). Cortisol level differences between anxiety and resting conditions in the summer were significantly higher than those in the spring (Table 5).
There was a significant interaction between seasonal effects (spring and summer) and conditional effects (resting and anxiety conditions) on the cortisol levels (p=0.037). Furthermore, there was a significant interaction between seasonal effects and conditional effects on testosterone levels (p=0.03). There was not a significant interaction between seasonal effects and conditional effects in regard to pain rating, anxiety rating, or pain threshold.
The results described herein indicate that hormones and pain perception are changed by exam anxiety, and that exam anxiety is affected by seasonal differences in testosterone and cortisol levels. When results from all 46 participants were analyzed, testosterone levels and pain thresholds were significantly lower under anxiety than at rest, while cortisol levels, pain ratings, and anxiety ratings were significantly higher under anxiety than at rest. Furthermore, when spring and summer data were analyzed separately, the results showed that seasonal differences in testosterone and cortisol levels under anxiety and at rest appeared to influence responses to pain stimuli.
Anecdotally, students have reported suffering from shaking hands, quivering voices and increased blood pressure during OSCE.1,40 In all 46 participants of the present study, anxiety ratings, SBP and heart rate were significantly higher under OSCE than at rest. Also, SBP differences between OSCE and resting conditions were positively correlated with pain rating differences between those two conditions. These findings suggest that the OSCE-induced anxiety activated the SNS, which might have increased pain ratings during the exam. Exam anxiety has been linked to significant increases in blood pressure and heart rate in college students.41 Stress also potentiates anxiety and induces increased salivary cortisol, blood pressure, heart rate, and subjective distress.42 Therefore, increased exam anxiety appears to increase SBP and pain ratings.
Salivary testosterone levels (88.64±40.86 pg/mL) collected in the spring when a subject was at rest were significantly higher than those (69.56±26.49 pg/mL) collected in the spring when the subject was under anxiety (Table 3), while salivary testosterone levels (63.19±26.07 pg/mL) collected in the summer when a subject was at rest were not significantly different from those (60.81±24.12 pg/mL) collected in the summer when the subject was under anxiety (Table 4). These results suggest that resting testosterone levels in Wonju may increase in the relatively pleasant spring months (88.64±40.86 pg/mL) and then decrease during the hot summer months (63.19±26.07 pg/mL). These changes in testosterone levels are in support of previous findings that testosterone levels are the lowest in months with the highest temperatures and longest hours of daylight.22 Similarly, in St. Louis, Missouri, the lowest testosterone levels were observed in August, and St. Louis has a climate similar to Wonju (the highest daytime August temperature and the average high temperature in August in Wonju are around 35℃ and 30℃, respectively, while the average high temperature in August in St. Louis is around 31℃).18
We previously showed that testosterone levels in humans are positively correlated with activation of the middle frontal cortex during electrical and thermal pain stimulation, leading to a decrease in pain perception.43,44 During the pain stimulation period, there is a significant negative correlation between serum testosterone levels and activation of the medial dorsal nucleus (the medial dorsal nucleus is thought to play a role in the affective and motivational aspects of pain).43,45 Furthermore, testosterone levels are positively correlated with pain thresholds during stress,36 and pain increases with a decrease in testosterone levels 30 min post-competition,46 suggesting that high testosterone levels may decrease pain sensation. The present results indicate that low testosterone levels in both resting and anxiety conditions during the summer did not contribute to increased pain perception under anxiety during the summer. Although it was not possible to infer a causal relationship between seasonal variation in testosterone and pain, the low testosterone levels observed under anxiety conditions in the spring, compared to the high levels observed under resting conditions in the spring might contribute to the increase in pain perception observed when individuals were under anxiety in the spring.
Salivary cortisol levels in the spring were not significantly different when a subject was under anxiety (3.03±2.85 ng/mL) compared to at rest (2.74±2.46 ng/mL) (Table 3), while the cortisol levels in the summer were significantly higher when a subject was under anxiety (4.92±4.32 ng/mL) compared to at rest (2.21±4.92 ng/mL) (Table 4). These results suggest that cortisol levels may not increase in response to anxiety during relatively pleasant spring weather in Wonju, but they may increase in response to anxiety during hot summer months. These results also indicate that changes in cortisol levels in response to anxiety in the summer11,12 might also affect the response to pain stimuli. This is supported by a previous study showing that cortisol levels are negatively correlated with pain thresholds during stress.36 Although it was not possible to infer a causal relationship between seasonal variation in cortisol and pain, these results suggest that the high cortisol levels observed under anxiety conditions during the summer, compared to the low levels observed under resting conditions during the summer, might contribute to the increase in pain perception observed when individuals were under anxiety in the summer.
The testosterone-to-cortisol ratios of all participants (n=46) and participants in the summer (n=21) were significantly higher in the resting condition than in the anxiety condition. Because testosterone inhibits the activity of the hypothalamic-pituitary-adrenal system, stress responses to threats are weaker when testosterone levels are high.47 Testosterone and cortisol function cooperatively to maintain appropriate balance in how an individual responds to rewarding stimuli vs. fearful or threatening stimuli.48 It is hypothesized that, in the amygdala, testosterone promotes reward-seeking and approach behavior,48,49 while cortisol promotes fearfulness and withdrawal behavior.48,50 A high testosterone-to-cortisol ratio may enhance sensitivity to rewards relative to punishments, and promote approach behavior rather than avoidance reactions.48 Individuals with a high testosterone-to-cortisol ratio might experience decreased pain sensation, which is shown in the present study by demonstrating that pain ratings were lower in the resting condition, when individuals' testosterone-to-cortisol ratios were higher.
This study has several limitations. It did not include all four seasons because it was based around the polyclinic schedule of the Department of Anesthesiology and Pain Medicine. In order to clarify seasonal variations in testosterone and cortisol levels under stress and at rest, future studies should be performed in a clinical practice or with a better experimental model. Only male participants were included in this study because there were too few female volunteers available for the study. In future studies, female participants should be included. Another limitation of this study is small sample size. Therefore, a randomized, controlled trial with a larger sample size is needed to validate the seasonal variations in testosterone and cortisol levels in participants at rest and under stress.
Although diurnal variations in testosterone and cortisol are relatively well understood, seasonal variations in testosterone and cortisol are not adequately documented. Seasonal variation in testosterone is related to seasonal changes in human behavior and physiology.51 Although further study is needed to clarify the effects of seasonal variations of testosterone and cortisol on pain responses, understanding that seasonal differences in testosterone and cortisol levels under anxiety and at rest may affect responses to pain stimuli could have important implications in a clinical practice.
In conclusion, the present study indicates that seasonal differences in testosterone and cortisol levels under anxiety and at rest may affect responses to pain stimuli, and these differences should be taken into account in future studies when investigating responses to pain stimuli. These results also suggest that acute clinical pain may be relieved by managing anxiety that is related to a decrease of testosterone in spring and a large increase of cortisol in summer.
Figures and Tables
Fig. 1
Correlation between systolic blood pressure differences and pain rating differences under anxiety and resting conditions (n=46). Horizontal axis: systolic blood pressure (SBP, mm Hg) differences between anxiety and resting conditions (SBP under anxiety conditions-SBP under resting conditions). Vertical axis: pain rating differences between anxiety and resting conditions (pain ratings under anxiety conditions-pain ratings under resting conditions).
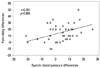
Table 2
Comparison of Hormone Levels and Other Parameters at Rest and Under Anxiety in Both Spring and Summer (n=46)
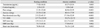
Table 3
Comparison of Hormone Levels and Other Parameters at Rest and Under Anxiety in the Spring (n=25)
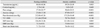
Table 4
Comparison of Hormone Levels and Other Parameters at Rest and Under Anxiety in the Summer (n=21)
ACKNOWLEDGEMENTS
The authors thank the participants of Yonsei University, Wonju College of Medicine for voluntarily participating in this experiment. The authors also thank Gi Bong Um, BA (Planning Team, Yonsei University), Gill Ho Lee, BA (Instructional Department, Yonsei University), Ju Seog Kim, BA (Librarian Section, Yonsei University), Sang Min Lee, BA (Academic Affairs, Yonsei University), and Myung Ha Kim, BA (Librarian Section, Yonsei University) for their excellent technical assistance.
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2012R1A1A2004868).
References
1. Brand HS, Schoonheim-Klein M. Is the OSCE more stressful? Examination anxiety and its consequences in different assessment methods in dental education. Eur J Dent Educ. 2009; 13:147–153.

2. Ng V, Koh D, Mok BY, Chia SE, Lim LP. Salivary biomarkers associated with academic assessment stress among dental undergraduates. J Dent Educ. 2003; 67:1091–1094.

3. Kirschbaum C, Hellhammer DH. Salivary cortisol in psychoneuroendocrine research: recent developments and applications. Psychoneuroendocrinology. 1994; 19:313–333.

4. Ng V, Koh D, Chia SE. Examination stress, salivary cortisol, and academic performance. Psychol Rep. 2003; 93(3 Pt 2):1133–1134.

5. Schulz P, Walker JP, Peyrin L, Soulier V, Curtin F, Steimer T. Lower sex hormones in men during anticipatory stress. Neuroreport. 1996; 7:3101–3104.

6. Van den Berghe G. The neuroendocrine response to stress is a dynamic process. Best Pract Res Clin Endocrinol Metab. 2001; 15:405–419.

7. Sternbach H. Age-associated testosterone decline in men: clinical issues for psychiatry. Am J Psychiatry. 1998; 155:1310–1318.

8. Edinger KL, Frye CA. Testosterone's anti-anxiety and analgesic effects may be due in part to actions of its 5alpha-reduced metabolites in the hippocampus. Psychoneuroendocrinology. 2005; 30:418–430.

9. Craft RM, Mogil JS, Aloisi AM. Sex differences in pain and analgesia: the role of gonadal hormones. Eur J Pain. 2004; 8:397–411.

10. van Anders SM, Hampson E, Watson NV. Seasonality, waist-to-hip ratio, and salivary testosterone. Psychoneuroendocrinology. 2006; 31:895–899.

11. Romero LM. Seasonal changes in plasma glucocorticoid concentrations in free-living vertebrates. Gen Comp Endocrinol. 2002; 128:1–24.

12. Romero LM, Wingfield JC. Alterations in hypothalamic-pituitary-adrenal function associated with captivity in Gambel's white-crowned sparrows (Zonotrichia leucophrys gambelii). Comp Biochem Physiol B Biochem Mol Biol. 1999; 122:13–20.

13. Andersson AM, Carlsen E, Petersen JH, Skakkebaek NE. Variation in levels of serum inhibin B, testosterone, estradiol, luteinizing hormone, follicle-stimulating hormone, and sex hormone-binding globulin in monthly samples from healthy men during a 17-month period: possible effects of seasons. J Clin Endocrinol Metab. 2003; 88:932–937.

14. Dabbs JM Jr. Age and seasonal variation in serum testosterone concentration among men. Chronobiol Int. 1990; 7:245–249.

15. Meriggiola MC, Noonan EA, Paulsen CA, Bremner WJ. Annual patterns of luteinizing hormone, follicle stimulating hormone, testosterone and inhibin in normal men. Hum Reprod. 1996; 11:248–252.

16. Nicolau GY, Haus E, Lakatua DJ, Bogdan C, Sackett-Lundeen L, Popescu M, et al. Circadian and circannual variations of FSH, LH, testosterone, dehydroepiandrosterone-sulfate (DHEA-S) and 17-hydroxy progesterone (17 OH-Prog) in elderly men and women. Endocrinologie. 1985; 23:223–246.
17. Nicolau GY, Lakatua D, Sackett-Lundeen L, Haus E. Circadian and circannual rhythms of hormonal variables in elderly men and women. Chronobiol Int. 1984; 1:301–319.

18. Perry HM 3rd, Miller DK, Patrick P, Morley JE. Testosterone and leptin in older African-American men: relationship to age, strength, function, and season. Metabolism. 2000; 49:1085–1091.

19. Reinberg A, Lagoguey M, Chauffournier JM, Cesselin F. Circannual and circadian rhythms in plasma testosterone in five healthy young Parisian males. Acta Endocrinol (Copenh). 1975; 80:732–734.

20. Reinberg A, Smolensky MH, Hallek M, Smith KD, Steinberger E. Annual variation in semen characteristics and plasma hormone levels in men undergoing vasectomy. Fertil Steril. 1988; 49:309–315.

21. Smals AG, Kloppenborg PW, Benraad TJ. Circannual cycle in plasma testosterone levels in man. J Clin Endocrinol Metab. 1976; 42:979–982.

22. Svartberg J, Jorde R, Sundsfjord J, Bønaa KH, Barrett-Connor E. Seasonal variation of testosterone and waist to hip ratio in men: the Tromsø study. J Clin Endocrinol Metab. 2003; 88:3099–3104.

23. Valero-Politi J, Fuentes-Arderiu X. Annual rhythmic variations of follitropin, lutropin, testosterone and sex-hormone-binding globulin in men. Clin Chim Acta. 1998; 271:57–71.

24. Baker HW, Burger HG, de Kretser DM, Hudson B, O'Connor S, Wang C, et al. Changes in the pituitary-testicular system with age. Clin Endocrinol (Oxf). 1976; 5:349–372.

25. Brambilla DJ, O'Donnell AB, Matsumoto AM, McKinlay JB. Lack of seasonal variation in serum sex hormone levels in middle-aged to older men in the Boston area. J Clin Endocrinol Metab. 2007; 92:4224–4229.

26. Dai WS, Kuller LH, LaPorte RE, Gutai JP, Falvo-Gerard L, Caggiula A. The epidemiology of plasma testosterone levels in middle-aged men. Am J Epidemiol. 1981; 114:804–816.

27. Martikainen H, Tapanainen J, Vakkuri O, Leppäluoto J, Huhtaniemi I. Circannual concentrations of melatonin, gonadotrophins, prolactin and gonadal steroids in males in a geographical area with a large annual variation in daylight. Acta Endocrinol (Copenh). 1985; 109:446–450.

28. Svartberg J, Barrett-Connor E. Could seasonal variation in testosterone levels in men be related to sleep? Aging Male. 2004; 7:205–210.

29. Vitzthum VJ, Worthman CM, Beall CM, Thornburg J, Vargas E, Villena M, et al. Seasonal and circadian variation in salivary testosterone in rural Bolivian men. Am J Hum Biol. 2009; 21:762–768.

30. Matchock RL, Dorn LD, Susman EJ. Diurnal and seasonal cortisol, testosterone, and DHEA rhythms in boys and girls during puberty. Chronobiol Int. 2007; 24:969–990.

31. Bellastella A, Criscuolo T, Mango A, Perrone L, Sinisi AA, Faggiano M. Circannual rhythms of plasma luteinizing hormone, follicle-stimulating hormone, testosterone, prolactin and cortisol in prepuberty. Clin Endocrinol (Oxf). 1983; 19:453–459.

33. Meagher MW, Arnau RC, Rhudy JL. Pain and emotion: effects of affective picture modulation. Psychosom Med. 2001; 63:79–90.

34. Rhudy JL, Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. 2000; 84:65–75.

35. Rhudy JL, Meagher MW. Noise stress and human pain thresholds: divergent effects in men and women. J Pain. 2001; 2:57–64.

36. Choi JC, Chung MI, Lee YD. Modulation of pain sensation by stress-related testosterone and cortisol. Anaesthesia. 2012; 67:1146–1151.

37. Kanegane K, Penha SS, Munhoz CD, Rocha RG. Dental anxiety and salivary cortisol levels before urgent dental care. J Oral Sci. 2009; 51:515–520.

39. Liening SH, Stanton SJ, Saini EK, Schultheiss OC. Salivary testosterone, cortisol, and progesterone: two-week stability, interhormone correlations, and effects of time of day, menstrual cycle, and oral contraceptive use on steroid hormone levels. Physiol Behav. 2010; 99:8–16.

40. Zartman RR, McWhorter AG, Seale NS, Boone WJ. Using OSCE-based evaluation: curricular impact over time. J Dent Educ. 2002; 66:1323–1330.

41. Zhang Z, Su H, Peng Q, Yang Q, Cheng X. Exam anxiety induces significant blood pressure and heart rate increase in college students. Clin Exp Hypertens. 2011; 33:281–286.

42. Grillon C, Duncko R, Covington MF, Kopperman L, Kling MA. Acute stress potentiates anxiety in humans. Biol Psychiatry. 2007; 62:1183–1186.

43. Choi JC, Park SK, Kim YH, Shin YW, Kwon JS, Kim JS, et al. Different brain activation patterns to pain and pain-related unpleasantness during the menstrual cycle. Anesthesiology. 2006; 105:120–127.

44. Choi JC, Yi DJ, Han BS, Lee PH, Kim JH, Kim BH. Placebo effects on analgesia related to testosterone and premotor activation. Neuroreport. 2011; 22:419–423.

45. Martin JH. Neuroanatomy: Text and Atlas. 3rd ed. New York: McGraw-Hill Companies;2003. p. 125–126.
46. Choi JC, Min S, Kim YK, Choi JH, Seo SM, Chang SJ. Changes in pain perception and hormones pre- and post-kumdo competition. Horm Behav. 2013; 64:618–623.

47. Terburg D, Morgan B, van Honk J. The testosterone-cortisol ratio: a hormonal marker for proneness to social aggression. Int J Law Psychiatry. 2009; 32:216–223.

48. Glenn AL, Raine A, Schug RA, Gao Y, Granger DA. Increased testosterone-to-cortisol ratio in psychopathy. J Abnorm Psychol. 2011; 120:389–399.

49. Daitzman R, Zuckerman M. Disinhibitory sensation seeking, personality and gonadal hormones. Pers Individ Differ. 1980; 1:103–110.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download