Abstract
Purpose
The aim of the present study was to evaluate the clinical characteristics of the primary Epstein-Barr virus (EBV) hepatitis with elevation of both serum alkaline phosphatase (ALP) and γ-glutamyltransferase (γ-GT) levels in children.
Materials and Methods
A retrospective study was performed by reviewing of the medical records of 36 patients who were diagnosed with primary EBV hepatitis. The patients were divided into 2 groups: patients with elevated serum ALP and γ-GT levels (group 1) and patients without (group 2).
Results
The classic features of infectious mononucleosis (fever, pharyngitis and/or tonsillitis, and cervical lymphadenitis) were seen in 20 (57.1%) of group 1 patients and 18 (50.0%) of group 2 patients. Hepatitis with elevated serum ALP and γ-GT levels were present in 14 (38.9%) of the all patients. Of these patients, Jaundice occurred in only 2 (5.6%). The mean levels of aspartate aminotransferase and alanine aminotransferase (ALT) as well as the number of patients with ALT greater than 400 IU/L were significantly different between the groups (177 IU/L vs. 94 IU/L, 418 IU/L vs. 115 IU/L, and 50.0% vs. 13.6%; p=0.001, p=0.001, p=0.026, respectively). The mean duration of elevated serum ALT levels was 17.5 days in group 1 and 9.0 days in group 2 (p=0.013). All patients recovered fully without any chronic or serious complications.
The Epstein-Barr virus (EBV), a member of the herpes virus family, is known as the cause of infectious mononucleosis (IM), which presents with fever, pharyngitis, lymphadenopathy, hepatosplenomegaly, and atypical lymphocytosis.1 Over 95% of adults worldwide are infected with this virus and about half of the population has primary EBV infection until the age of 5 in industrialized countries.2 Although most children with EBV infections usually have mild or no symptoms, some children or adults manifest symptomatic full-blown IM.2,3 In the acute phase of primary EBV infections, hepatic involvement is common. Mild to moderate elevations of liver enzymes are seen in up to 80% to 90% of patients, while jaundice may occur in 5%.4,5 Hepatic failure has rarely been reported.5,6 According to a study on adults, hepatitis due to primary EBV infection is mostly benign and resolves spontaneously within 5 weeks.7 However, little is known about the clinical features and natural course of primary EBV hepatitis in children.
The aim of the present study was to evaluate the presenting features and clinical course of acute hepatitis in children with elevation of both serum alkaline phosphatase (ALP) and γ-glutamyltransferase (γ-GT) levels caused by primary EBV infection.
We retrospectively collected data on patients who were treated for acute hepatitis due to primary EBV infection at the Department of Pediatrics, Chungnam National University Hospital between September 2005 and December 2012.
The diagnosis of primary EBV hepatitis was made based on the elevation of serum alanine aminotransferase (ALT) level over 45 IU/L and early positive immunoglobulin M antibody to EBV viral capsid antigen (anti-EBV VCA IgM) or early positive anti-EBV VCA IgG with positive EBV-polymerase chain reaction (PCR) in the absence of antibody to EBV early antigen (EA) and EB nuclear antigen (anti-EBNA). Anti-VCA IgM, anti-VCA IgG, anti-EA and anti-EBNA were detected by enzyme immunoassay test system (Toshiba Medical Systems Co., Tokyo, Japan). EBV DNA was detected by PCR (Bio-Rad C1000 Touch™ Thermal cycler, Hercules, CA, USA).
In the present study, patients with primary EBV hepatitis were divided into 2 groups: group 1 included patients with elevation of both serum ALP and γ-GT levels greater than the upper limit of normal reference values according to age and sex. Group 2 were patients with hepatitis, but without any elevation in ALP and γ-GT levels.
Patients with the following characteristics were excluded from the study: 1) early detection of anti-EBNA, 2) loss to follow-up before normalization of ALT, 3) missing medical records, 4) cytomegalovirus (CMV) co-infection (positive CMV IgM and positive urine CMV-PCR and/or culture), or 5) pre-existing hepatitis or other underlying disease. The Institutional Review Board of Chungnam National University Hospital approved the study.
Medical records were reviewed for patient, demographics, clinical features, laboratory results, clinical course, and outcomes. Collected data were analyzed using SPSS ver. 19.0 (SPSS Inc., Chicago, IL, USA). Fisher's exact test was used to compare clinical features between groups 1 and 2. The Mann-Whitney U test was performed to examine the differences in laboratory findings, the duration of fever, the peak time of ALT, the duration of abnormal ALT levels, and the length of hospital stays between the two groups. A p value <0.05 was considered statistically significant.
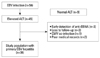
Elevation of liver enzymes occurred in 45 (83.3%) of the 54 patients who were diagnosed with acute EBV infection. Of these 45 patients, nine were excluded from the study because of early detection of anti-EBNA (n=3), loss to follow-up (n=3), poor medical records (n=2), and CMV co-infection (n=1) (Fig. 1). Thirty-six patients, aged 10 months to 16.7 years (mean, 6.3±4.2 years), were recruited for the study. Of these 36 patients, 24 (66.7%) were less than 7 years of age. Fig. 2 shows the age distribution. The male to female ratio was approximately 1 : 1 (males 19 and females 17).
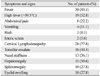
The most common clinical feature was fever, which was noted in 30 (83.3%) patients. High fever over 39.5℃ was present in 19 (52.8%) patients. The mean fever duration was 9.0 days (range, 1-16 days). Cervical lymphadenopathy was the second most common clinical feature and noted in 28 (77.8%) patients. Tonsillar exudates were observed in 16 (44.4%) patients. The classic features of IM such as fever, pharyngitis or tonsillitis, and lymphadenopathy were seen in 19 (52.8%) patients. Hepatomegaly and splenomegaly were observed in 13 (30.6%) and 10 (27.8%) patients, retrospectively. Gastrointestinal symptoms included abdominal pain (n=8, 22.2%), vomiting (n=4, 11.1%), and jaundice (n=2, 5.6%). Skin rash was present in three (8.3%) patients.
Gall bladder wall thickening (GBWT) was identified in 6 (50.0%) of 12 patients (group 1, n=7; group 2, n=5), who were examined by abdominal ultrasonography (US) or computed tomography (CT). GBWT was observed in four (57.1%) of the seven in group 1 and two (40.0%) of the five patients in group 2. Of these four patients with GBWT in group 1, two had an additional finding of fluid collection around the gall bladder (GB) and one had combined GB hydrops suggestive acute acalculous cholecystitis. In contrast, the two patients in group 2 had only GBWT without findings of fluid collection.
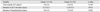
Clinical features and their comparisons between the two groups are presented in Table 1 and 2. There were no significant differences in age, the male to female ratio, and the duration of fever nor the incidences of abdominal pain, jaundice, hepatomegaly, splenomegaly and GBWT between the groups (Table 2).
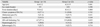
The mean leukocyte count was 15073/µ (SD, 5515/µ), with a range of 4490-32350/µ, in which lymphocytes were dominant. Leukocytosis (white blood cell ≥10000) was noted in 31 (86.1%) patients. Atypical lymphocytosis (atypical lymphocyte ≥10%) was observed in 14 (38.9%) patients. Serum ALT levels greater than 10 times the upper normal limit were seen in 10 (27.8%) patients, which were more common in group 1 than in group 2 (p=0.026). Serum ALT levels above 1000 IU/L occurred in four (11.1%) of patients. Elevations of both ALP and γ-GT were observed in 14 (38.9%) patients. Of these patients, two (5.6%) had elevated serum direct bilirubin levels. The leukocytes, neutrophils, lymphocytes, atypical lymphocytes, and platelet counts were not significantly different between the groups. Serum transaminases levels and the proportion of serum ALT levels greater than 400 IU/L were higher in group 1 than in group 2 (p=0.001, p=0.001, and p=0.026, respectively) (Table 3).
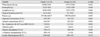
The mean time to peak serum ALT levels after the first presentation of EBV infection was 5.4 days in group 1 and 6.6 days in group 2, but there was no statistical significance. The mean duration of serum ALT elevation was significantly longer in group 1 than in group 2 (p=0.013). Complications occurred in eight patients, which included pneumonia in four patients, sinusitis in two, splenic infarction in one, bilateral pleural effusion/ascites in one. The incidence of complications and the mean duration of hospitalization were not significantly different between the groups (Table 4).
Antibiotics were prescribed to 15 (41%) patients at the beginning of treatment because of suspicious bacterial infections and discontinued in most of them soon after hospitalization. Steroids were given to reduce inflammation in two patients. One patient presented with a prolonged high fever, and the other had a high fever with severe nasal obstruction. All patients recovered fully without any complications.
In this retrospective study, we described the clinical characteristics of primary EBV hepatitis. We also compared laboratory findings as well as the clinical courses between the groups. Group 1 presented with hepatitis with elevation of both ALP and γ-GT levels and group 2 had hepatitis without any elevation in ALP and γ-GT levels. The results showed that hepatic manifestations of EBV infection usually occurred in those less than 7 years of age and half of our patients did not have the classic features of IM. Primary EBV hepatitis with elevation of both ALP and γ-GT levels occurred frequently, but jaundice was rare. Importantly, patients in group 1 had higher serum aminotransferases levels and a significantly longer mean duration of elevated serum aminotransferase levels than patients in group 2.
In the literature, hepatic involvement occurs in 80% to 90% of primary EBV infection and is mostly mild and self-limited.4,7,8 Serum aminotransferase levels are usually elevated by less than 5 times the upper normal level, infrequently greater than 10 times, and rarely over 1000 IU/L.8,9 Kofteridis, et al.7 reported in a study of adults that abnormalities of aminotransferase levels occurred from the first week after the onset of EBV infection, reached the peak levels during the second week, and normalized 3 weeks later.
In our study, liver enzyme increased in 30 (83.3%) of all patients, which was similar to the result of a previous report.9 Serum ALT levels that were elevated to more than 10 times the upper normal limit were observed in approximately one-third of our patients, which is higher than the incidence of previous reports.10,11 The incidence of serum ALT greater than 1000 IU/L was similar to a previous study.8 Serum ALT levels peaked within 2 weeks and returned to normal between 5 and 78 days after the first presentation of EBV infection such as fever, sore throat, or lymph node swelling. The mean duration of elevated serum ALT levels was significantly longer in group 1 than in group 2.
Cholestatic jaundice with elevated serum direct bilirubin levels have been reported in only a small number of cases during acute EBV infection.5,7,11-13 According to a study by Kofteridis, et al.,7 only 6% had clinical jaundice, but the transient cholestatic liver disease was the predominant hepatic involvement with biochemical abnormalities of elevated ALP and γ-GT in 59%.7 In the present study, hepatitis with biochemical abnormalities of the elevated ALP and γ-GT levels occurred in 14 (39%) patients, and that is lower than the result by a previous study.7 However, the incidence of the cholestatic jaundice is similar to that of previous study.7 In our icteric patients, serum bilirubin levels were elevated at an early phase of EBV hepatitis and returned to normal within 1 week after the onset of jaundice.
The pathogenesis of EBV hepatitis is still poorly understood. In general hepatotrophic viruses, such as hepatitis B and C, infect hepatocytes directly without cytopathic activity and liver injury results from the immune response to viral antigens expressed by infected hepatocytes.14,15 In contrast to hepatotrophic viruses, EBV does not infect hepatocytes, biliary epithelium, or sinusoidal epithelium.16 Recent experimental reports have shown that EBV-infected CD8+ T cells accumulate in the liver and produce some soluble products, especially interferon-γ, tumor necrosis factor α, and Fas ligand, which can destroy hepatocytes.16-19
A recent report showed that hepatomegaly and splenomegaly occurred in 24.7% and 12.3% of children with IM, retrospectively.20 In our study, hepatomegaly and splenomegaly were seen in nearly one-third of patients, which was higher than the results of Son and Shin20 probably because enrollment was restricted to patients with elevated serum aminotransferase levels in this study.
GBWT with or without GB distension may occur during the IM.21-23 A GBWT greater than 3 mm is defined as abnormal.24 Yamada and Yamada21 documented that duration of hospitalization was longer in patients with GBWT than in those without, and GBWT could be a sign of the severity of IM. However, GBWT is considered a nonspecific sign that can be seen in many conditions, including acute cholecystitis and acute hepatitis. In our study, there was no significant difference in duration of hospitalization between patients with GBWT and those without, which is inconsistent with the study by Yamada and Yamada.21 We could not clarify the clinical significance of GBWT because abdominal US or CT was performed on 12 select patients who had gastrointestinal manifestations and/or organomegaly.
Most patients with EBV hepatitis spontaneously recovered with supportive care. Sterods and antiviral agents are usually not effective and their use remain controversial in the treatment of EBV hepatitis, especially in patients with severe hepatic involvement.25 Orthotopic liver transplantation performed as a therapeutic option in a case of fulminant hepatitis caused by EBV infection.6 Steroids along with antiviral drugs were administered in 2 (5.6%) of our patients. All of our patients completely recovered without any chronic or serious illness.
In conclusion, although our study has some limitations due to its small number of patients and retrospective nature, it suggests that primary EBV hepatitis with predominant biochemical abnormalities of elevated ALP and γ-GT may represent a benign disease of mostly an anicteric nature, but a delay in recovery of liver function.
Figures and Tables
Fig. 1
Enrollment of patients. EBV, Epstein-Barr virus; ALT, alanine aminotransferase; anti-EBNA, EB nuclear antigen; CMV, cytomegalovirus.
References
1. Sumaya CV, Ench Y. Epstein-Barr virus infectious mononucleosis in children. I. Clinical and general laboratory findings. Pediatrics. 1985; 75:1003–1010.
2. Luzuriaga K, Sullivan JL. Infectious mononucleosis. N Engl J Med. 2010; 362:1993–2000.
3. Straus SE, Cohen JI, Tosato G, Meier J. NIH conference. Epstein-Barr virus infections: biology, pathogenesis, and management. Ann Intern Med. 1993; 118:45–58.

5. Shaw NJ, Evans JH. Liver failure and Epstein-Barr virus infection. Arch Dis Child. 1988; 63:432–433.

6. Feranchak AP, Tyson RW, Narkewicz MR, Karrer FM, Sokol RJ. Fulminant Epstein-Barr viral hepatitis: orthotopic liver transplantation and review of the literature. Liver Transpl Surg. 1998; 4:469–476.

7. Kofteridis DP, Koulentaki M, Valachis A, Christofaki M, Mazokopakis E, Papazoglou G, et al. Epstein Barr virus hepatitis. Eur J Intern Med. 2011; 22:73–76.

8. Vine LJ, Shepherd K, Hunter JG, Madden R, Thornton C, Ellis V, et al. Characteristics of Epstein-Barr virus hepatitis among patients with jaundice or acute hepatitis. Aliment Pharmacol Ther. 2012; 36:16–21.

9. Finkel M, Parker GW, Fanselau HA. The Hepatitis of infectious mononucluosis: experience with 235 cases. Mil Med. 1964; 129:533–538.
10. Horwitz CA, Burke MD, Grimes P, Tombers J. Hepatic function in mononucleosis induced by Epstein-Barr virus and cytomegalovirus. Clin Chem. 1980; 26:243–246.

11. Méndez-Sánchez N, Aguilar-Domínguez C, Chávez-Tapia NC, Uribe M. Hepatic manifestations of Epstein-Barr viral infection. Ann Hepatol. 2005; 4:205–209.

12. Hara S, Hoshino Y, Naitou T, Nagano K, Iwai M, Suzuki K, et al. Association of virus infected-T cell in severe hepatitis caused by primary Epstein-Barr virus infection. J Clin Virol. 2006; 35:250–256.

13. Hinedi TB, Koff RS. Cholestatic hepatitis induced by Epstein-Barr virus infection in an adult. Dig Dis Sci. 2003; 48:539–541.
14. Chang JJ, Lewin SR. Immunopathogenesis of hepatitis B virus infection. Immunol Cell Biol. 2007; 85:16–23.

15. Rosen HR. Hepatitis C pathogenesis: mechanisms of viral clearance and liver injury. Liver Transpl. 2003; 9:S35–S43.

16. Kimura H, Nagasaka T, Hoshino Y, Hayashi N, Tanaka N, Xu JL, et al. Severe hepatitis caused by Epstein-Barr virus without infection of hepatocytes. Hum Pathol. 2001; 32:757–762.

17. Küsters S, Gantner F, Künstle G, Tiegs G. Interferon gamma plays a critical role in T cell-dependent liver injury in mice initiated by concanavalin A. Gastroenterology. 1996; 111:462–471.

18. Bradham CA, Plümpe J, Manns MP, Brenner DA, Trautwein C. Mechanisms of hepatic toxicity. I. TNF-induced liver injury. Am J Physiol. 1998; 275(3 Pt 1):G387–G392.
19. Kondo T, Suda T, Fukuyama H, Adachi M, Nagata S. Essential roles of the Fas ligand in the development of hepatitis. Nat Med. 1997; 3:409–413.

20. Son KH, Shin MY. Clinical features of Epstein-Barr virus-associated infectious mononucleosis in hospitalized Korean children. Korean J Pediatr. 2011; 54:409–413.

21. Yamada K, Yamada H. Gallbladder wall thickening in mononucleosis syndromes. J Clin Ultrasound. 2001; 29:322–325.

22. Lagona E, Sharifi F, Voutsioti A, Mavri A, Markouri M, Attilakos A. Epstein-Barr virus infectious mononucleosis associated with acute acalculous cholecystitis. Infection. 2007; 35:118–119.

23. Iaria C, Arena L, Di Maio G, Fracassi MG, Leonardi MS, Famulari C, et al. Acute acalculous cholecystitis during the course of primary Epstein-Barr virus infection: a new case and a review of the literature. Int J Infect Dis. 2008; 12:391–395.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download