Abstract
Purpose
Our aim was to determine the effects of infliximab on bone mineral metabolism in rheumatoid arthritis (RA) patients and analyze the relationship between inflammatory markers of acute phase thought to play a major role in bone remodeling.
Materials and Methods
36 patients with established RA were investigated. All patients underwent physical examination and blood and urinary analysis at baseline, 2 weeks, 14 weeks, 6 months and 12 months after the initiation of treatment. The serum levels of: tumor necrosis factor alpha (TNF-alpha), tumor necrosis factor alpha receptor 1 (TNFR1), TNFR2, interleukin 6 (IL-6), IL-17, IL-23 and markers of bone remodeling such as osteocalcin (BGP), deoxypyridynoline (Dpd), and N-telopeptide of type I collagen (NTx) were measured by ELISA.
Results
The results showed significant decrease of all the above cytokines levels in RA patients in comparison with those after 2 weeks of treatment. After 6 months, the markers of bone formation and resorption decreased compared to baseline values. We found positive correlation between the levels of NTx and the levels of IL-6, IL-17 and TNFR1, and between the levels of Dpd and IL-6 and Dpd and TNFR2, whereas negative correlation between BGP and IL-23. After 12 months the positive association was found at the BGP level and IL-6 as well as Dpd and the level of IL-6. We also observed a positive relation between Dpd and TNF-alpha and negative between BGP and TNFR1.
Rheumatoid arthritis (RA) is a chronic, inflammatory connective tissue disease which leads to joint destruction and consequently to disability and premature death.1,2 Cytokines are intimately involved in RA pathogenesis. The interaction between various inflammatory cells and bone has been known to be mediated by cytokines and chemokines, however, also by direct cell-cell interaction, thus remodeling the bone matrix generating osteoblast and the bone resorbing osteoclasts. Osteoclasts are multicleated giant cells and are responsible for bone resorption and play a crucial role in bone remodelling in RA. interleukin 6 (IL-6) and tumor necrosis factor (TNF) induce osteoclast formation indirectly by stimulating osteoblast. Production of IL-6 from osteoblasts is induced by IL-17. It is know that in RA patients IL-17 has a pathogenetic role in the abnormal cartilage destruction and it has been shown to have powerful inflammatory properties and to be able to reduce bone formation via inhibition of the type I collagen synthesis as well as increase bone destruction.3 TNF-alpha and IL-17 contribute to osteoclastic bone resorption in RA patients.4 In addition, IL-17 induces the expression of Nuclear Factor-KappaB ligand receptor that is essential signal for differentiation of osteoclast and bone resorption.5,6 This cytokine is one of the factors associated with pathogenesis of RA, as manifested by IL-23 induced osteoclastogenesis.7 TNF-alpha is a pleiothropic cytokine produced in response to different antigens. Soluble receptors of TNFR1 (p55, CD120a) and TNFR2 (p75, CD120b) have a physiologic role in neutralizing many cytokines and are part of a feedbox loop that can modulate the inflammatory action of TNF-alpha.8,9 TNF-alpha binds to TNF receptors on the surface of many cells (monocytes, T cells, fibroblasts or osteoblasts).10,11 Biological therapy with TNF-blocking agents represents the most effective therapy so far available to patients with RA. Infliximab, a chimeric IgG1 antibody against TNF-alpha binds to soluble and membrane-bound TNF-alpha with a high affinity, and inhibits its effect by blocking TNF receptors interaction. Our aim was to determine the effects of infliximab on bone mineral metabolism by measuring biochemical parameters involved in the process of bone formation and resorption in RA patients and to analyze the relationship between many inflammatory markers of acute phase which have been thought to play major roles in osteoclast activation and bone resorption.
Thirty six patients (women's) with established RA were investigated, diagnosed according to the criteria of the American College of Rheumatology. Their mean age was 48 years [standard deviation (SD)=12] with a range of 35 to 69 years, and disease duration was 120 months. None of the patients had a history of hormone (oestrogen) replacement therapy or had used any other bone-sparing drugs or calcium supplements. Infliximab i.v. (3 mg/kg) was administrated by intravenous infusion at dose 3 mg/kg at the baseline, then at 2 weeks, 6 weeks and then every 8 weeks. MTX was administered orally. All patients underwent general and physical examination, and routine blood and urinary analysis at baseline, 14 weeks, 6 months and 12 months after the initial treatment.
At each treatment visit, serum and urine samples were collected before infliximab administration. Blood samples from all patients were taken in the morning after overnight fasting, without anticoagulants. Serum was separated immediately and stored at -70℃. Urine samples were obtained from the second morning portion after 24 hour diet (without calcium and food consisting collagen). Urine samples were spin and stored at -70℃. The serum levels of TNF-alpha, TNFR1, TNFR2, IL-6, IL-17 and IL-23 were measured by ELISA using the Quantikine kit from R&D System (Minneapolis, MN, USA). Osteocalcin (BGP), deoxypyridynoline (Dpd), and N-telopeptide of type I collagen (NTx) were measured by ELISA using Novocalcin and Pyrilinks-D kits from Metra Biosystems (Minneapolis, MN, USA) and Ostex International Inc. (USA), respectively.
All values are given as median and mean±SD. The Mann-Whitney U test was used for comparison of two independent variables, the Fisher test (differences were considered significant for p<0.05) was used for comparison of two dependent variables. The Spearman test was used to determine the correlation between the variables.
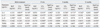
The results of our study showed statistically significant (p<0.01) decrease of all cytokines levels (IL-6, IL-17, IL-23, TNF-alpha, TNFR1 and TNFR2) in RA patients after 2 weeks of treatment. After 14 weeks, the levels of IL-6 (p<0.05), IL-17 (p<0.01), IL-23 (p<0.01), TNF-alpha (p<0.01), TNFR1 (p<0.01), and TNFR2 (p<0.01) were significantly lower in the patients treated with infliximab as compared to the results before the treatment. Moreover, IL-23 level was significantly (p<0.05) lower than that after 2 weeks of treatment and the levels of the cytokines (p<0.01) were still low at 6 months. Three of them (IL-23, TNF-alpha and TNFR2) were also decreased (p<0.05) compared to the levels after 2 weeks of treatment. Nevertheless, none of the cytokines showed statistically significant changes, compared to the levels measured at 14 weeks. The results of our study showed statistically significant decrease of the levels of IL-6 (p<0.05), IL-17 (p<0.01), IL-23 (p<0.01), TNF-alpha (p<0.01), TNFR1 (p<0.01) and TNFR2 (p<0.01) in RA patients, in comparison to the levels measured at 12 months of treatment. At the end of our study, the levels of cytokines such as IL-23, TNF-alpha, TNFR1 and TNFR2 were significantly lower (p<0.05), compared to 2 weeks of treatment. However, there was no statistical significance in all the cytokines analysed between the levels measured at 14 weeks and 6 months, compared to 12 months (Table 1).
The biochemical markers of osteoporosis (BGP, Dpd, and NTx) were determined in all patients, but the second measurement was done 14 weeks after initial treatment because of bone's remodelling. The levels of BGP (p<0.05) and NTx (p<0.01), but not Dpd were statistically significantly lower at 14 weeks in comparison to the results before treatment. After 6 months, statistically significant decrease of both, bone formation and resorption markers was observed in RA patients who received the therapy at the beginning of observation (p<0.01). Changes observed in RA patients who were treated with infliximab revealed significant decrease in the level of BGP (p<0.01), NTx (p<0.01) and Dpd (p<0.01) after 12 months, compared to the results before treatment. The levels of BGP, but not other markers, were found to be significantly lower compared to week 14. There was no statistical significance in all biochemical markers of osteoporosis analysed at 6 months and 12 months (Table 2).
We found positive correlation between the levels of NTx and IL-6, IL-17 and TNFR1 as well as between those of Dpd and IL-6, and Dpd and TNFR2, whereas negative correlation between BGP and IL-23 in RA patients before the treatment. At 14 weeks of the treatment, NTx level correlated significantly with IL-6, IL-17, TNF-alpha and TNFR1 levels. There was also a positive correlation between Dpd and IL-6 levels. At 6 months of infliximab treatment, positive correlations were found between NTx and IL-6 levels, and between Dpd and IL-6 levels whereas negative correlations between BGP and IL-17, and BGP and IL-23 levels. At the end of our measurement (12 months), a positive association was found between BGP and IL-6 levels as well as Dpd and IL-6 levels. We also observed a positive relation between Dpd and TNF-alpha and negative one between BGP and TNFR1 (Table 3).
Osteoclasts play an important role in bone remodeling in RA, however, the mechanism of osteoclasts activation or differentiation is still unclear. Generalized bone loss in RA patients may be influenced by inflammatory process associated with the levels of TNF, IL-6 or IL-17 and treatments such as corticoids. Therefore, the mechanism responsible for causing joint damage and functional impairments in RA is complex.12-15 Biological therapy with TNF-blocking agents represents the most effective therapeutic modality available to patients with RA.16 Therefore, we set out to show that infliximab inhibits bone destruction highly effectively and found that treatment with infliximab resulted in significant early decrease of the inflammatory markers. All the cytokines examined were found to be significantly lower after the first injection of infiximab. In RA patients several pathophysiological processes such as activity of inflammatory process or erosive joint destruction and high rate of bone turnover as occurs in osteoporosis, could be measured by elevated concentrations of bone metabolism markers.17 Similar to a previous study,18 disease activity in our present study, measured by cytokines levels, was not only decreased rapidly after the initial treatments, but they were also significantly decreased 14 weeks after the initial treatment and were still low 6 and 12 months after the initial treatment. The same could be said of the bone formation marker BGP as well as resorption marker NTx. It is well know that bone alkaline phosphatase is early marker of osteoblasts differentiation and useful marker of bone formation while NTx and Dpd have been showed to be useful markers of bone resorption. Torikai, et al.17 showed a significant decrease of Ntx, but not BGP levels, in RA patients who were treated with infliximab. In our study, infliximab treatment significantly decreased the levels of BGP and NTx, but not Dpd, at week 14. At 6 months, the levels of all bone markers measured were still low and significantly changed compared to their levels before the treatment. However, NTx and Dpd did not significantly change during the treatment. In contrast to the result of Torikai, et al.17 BGP levels in our study also decreased significantly after 12 months compared to 14 weeks of treatment. Kageyama, et al.19 found that serum levels of IL-23 at baseline changed not only after first injection but significantly decreased at 14 and 30 weeks after the initial infusion in good agreement with our results. Moreover, IL-23 in our study was only one of all cytokines measured which was statistically lower at 14 weeks compared to 2 weeks. This differences in the levels of cytokines during treatment may suggest at possibility that serum IL-23 levels are reduced by infliximab through a different pathway. The role of IL-23 in inflammatory process in RA has not been clearly understood: it may not depend on the general suppression of inflammation. In the current study, treatment with infliximab was showed to result in negative correlations between markers of bone formation BGP and IL-23 at 6 months of treatment. IL-23 was negatively correlated only with NTx at 6 month, and there were no associations with other biochemical markers of osteoporosis at any time of during the study. BGP also correlated with IL-6 at 12 months. The positive correlations between BGP, cytokines IL-6, and TNF-alpha measured at 12 months demonstrate the importance of inflammatory processes in RA patients. These result suggests that changes of IL-6 are associated with the changes in disease processes that occur during infliximab treatment. Furthermore, NTx and Dpd seem to be valuable markers to detect bone loss in RA and might be useful for treatment monitoring and evaluation of RA. We confirmed that NTx levels were associated mainly with the activity of cytokines before treatment, followed by IL-6, IL-17 and TNFR2 as well as at 14 week of treatment. Greenspan, et al.20 and Ravn, et al.21 indicated that NTx is a more sensitive marker than Dpd when measuring bone-derived type I collagen fragment. Our results also confirmed this conclusion. Infliximab potently inhibited IL-17 induced osteoclastogenesis by blocking TNF-alpha, consistent with the clinical effect of TNF-alpha antibody treatment in preventing bone destruction. In contrast to Kageyama, et al.22 who showed no significances changes at 14 and 30 weeks compared to those at pretreatment, the levels of IL-17 rapidly reduced in our study after the first injection of infliximab, which may suggest that the activity of this cytokines is inhibited by infliximab. The IL-17 levels were low at 14 weeks, 6 and 12 months, but not significant compared to previous measurement, and they correlated with NTx at first measurement and after 14 weeks. In RA patients IL-17 has a significant role in the destruction of bone, because begin the mechanism of osteoclastogenesis. It may suggest that control of production and function of this cytokine could be a strategy for the treatment of RA.23 Many studies on RA patients with active disease indicate that increased bone turnover and inflammation are important in the pathophysiology of RA-related osteoporosis, and that infliximab may slow down bone destruction. In fact, this is the first report to shown many cytokines related to bone metabolism. However, our study has several limitations. The number of patients in this study was low. Soluble receptors have short plasma half-lives and it would be required to neutralize the effects on inflammatory cytokines. In fact, during measured levels of bone markers in serum, we can not differentiate between local and systemic bone loss, these are the results of ongoing or decreased juxtaarticulare bone destruction or resorption and the systemic bone remodeling.
In conclusion, we showed that infliximab not only reduced clinical disease activity measured by cytokine levels, but also had a positive effect on bone remodeling. Thus, it is highly possible that it may limit the risk of osteoporosis in rheumatoid arthritis patients.
Figures and Tables
Table 1
The Levels of Interleukin-6 (IL-6), Interleukin-17 (IL-17), Interleukin-23 (IL-23), Tumour Necrosis Factor-α (TNF-α), Tumour Necrosis Factor-Receptor 1 (TNFR1), and Tumour Necrosis Factor-Receptor 2 (TNFR2) in Rheumatoid Arthritis Patients Treated with Infliximab

Table 2
The Levels of Osteocalcin (BGP), N-Telopeptide of Type I Collagen (NTx), and Deoxypyridynoline (Dpd) before and during Treatment with Infliximab in Rheumatoid Arthritis Patients

References
2. Vandenbroucke JP, Hazevoet HM, Cats A. Survival and cause of death in rheumatoid arthritis: a 25-year prospective followup. J Rheumatol. 1984. 11:158–161.
3. Li X, Yuan FL, Lu WG, Zhao YQ, Li CW, Li JP, et al. The role of interleukin-17 in mediating joint destruction in rheumatoid arthritis. Biochem Biophys Res Commun. 2010. 397:131–135.

4. Kotake S, Udagawa N, Takahashi N, Matsuzaki K, Itoh K, Ishiyama S, et al. IL-17 in synovial fluids from patients with rheumatoid arthritis is a potent stimulator of osteoclastogenesis. J Clin Invest. 1999. 103:1345–1352.

5. Nakashima T, Kobayashi Y, Yamasaki S, Kawakami A, Eguchi K, Sasaki H, et al. Protein expression and functional difference of membrane-bound and soluble receptor activator of NF-kappaB ligand: modulation of the expression by osteotropic factors and cytokines. Biochem Biophys Res Commun. 2000. 275:768–775.

6. Kelchtermans H, Schurgers E, Geboes L, Mitera T, Van Damme J, Van Snick J, et al. Effector mechanisms of interleukin-17 in collagen-induced arthritis in the absence of interferon-gamma and counteraction by interferon-gamma. Arthritis Res Ther. 2009. 11:R122.
7. Yago T, Nanke Y, Kawamoto M, Furuya T, Kobashigawa T, Kamatani N, et al. IL-23 induces human osteoclastogenesis via IL-17 in vitro, and anti-IL-23 antibody attenuates collagen-induced arthritis in rats. Arthritis Res Ther. 2007. 9:R96.

8. Choy EH, Panayi GS. Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med. 2001. 344:907–916.

9. Mohler KM, Torrance DS, Smith CA, Goodwin RG, Stremler KE, Fung VP, et al. Soluble tumor necrosis factor (TNF) receptors are effective therapeutic agents in lethal endotoxemia and function simultaneously as both TNF carriers and TNF antagonists. J Immunol. 1993. 151:1548–1561.
10. Scali JJ, Visentini S, Salomón J, Sevilla D, Ju YC, Morales E, et al. Rapid and deep control of inflammation in rheumatoid arthritis with infliximab and its correlation with acute-phase reactants. Ann N Y Acad Sci. 2007. 1110:389–401.

12. Martin JC, Munro R, Campbell MK, Reid DM. Effects of disease and corticosteroids on appendicular bone mass in postmenopausal women with rheumatoid arthritis: comparison with axial measurements. Br J Rheumatol. 1997. 36:43–49.

13. Laan RF, van Riel PL, van de Putte LB. Bone mass in patients with rheumatoid arthritis. Ann Rheum Dis. 1992. 51:826–832.

14. Van Bezooijen RL, Van Der Wee-Pals L, Papapoulos SE, Löwik CW. Interleukin 17 synergises with tumour necrosis factor alpha to induce cartilage destruction in vitro. Ann Rheum Dis. 2002. 61:870–876.

15. Lubberts E, Koenders MI, van den Berg WB. The role of T-cell interleukin-17 in conducting destructive arthritis: lessons from animal models. Arthritis Res Ther. 2005. 7:29–37.
16. Taylor PC. Anti-TNFalpha therapy for rheumatoid arthritis: an update. Intern Med. 2003. 42:15–20.

17. Torikai E, Kageyama Y, Takahashi M, Nagano A. The effect of methotrexate on bone metabolism markers in patients with rheumatoid arthritis. Mod Rheumatol. 2006. 16:350–354.

18. Korczowska I, Hrycaj P, Lacki JK. Does infliximab decrease bone turnover in rheumatoid arthritis patients. Joint Bone Spine. 2003. 70:398–400.

19. Kageyama Y, Kobayashi H, Kato N. Infliximab treatment reduces the serum levels of interleukin-23 in patients with rheumatoid arthritis. Mod Rheumatol. 2009. 19:657–662.

20. Greenspan SL, Parker RA, Ferguson L, Rosen HN, Maitland-Ramsey L, Karpf DB. Early changes in biochemical markers of bone turnover predict the long-term response to alendronate therapy in representative elderly women: a randomized clinical trial. J Bone Miner Res. 1998. 13:1431–1438.

21. Ravn P, Clemmesen B, Christiansen C. Alendronate Osteoporosis Prevention Study Group. Biochemical markers can predict the response in bone mass during alendronate treatment in early postmenopausal women. Bone. 1999. 24:237–244.

22. Kageyama Y, Takahashi M, Torikai E, Suzuki M, Ichikawa T, Nagafusa T, et al. Treatment with anti-TNF-alpha antibody infliximab reduces serum IL-15 levels in patients with rheumatoid arthritis. Clin Rheumatol. 2007. 26:505–509.

23. Yago T, Nanke Y, Ichikawa N, Kobashigawa T, Mogi M, Kamatani N, et al. IL-17 induces osteoclastogenesis from human monocytes alone in the absence of osteoblasts, which is potently inhibited by anti-TNF-alpha antibody: a novel mechanism of osteoclastogenesis by IL-17. J Cell Biochem. 2009. 108:947–955.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download