Abstract
Purpose
A significant number of patients who have experienced previous surgical treatment for an osteoporotic hip fracture experience a subsequent hip fracture (SHF) on the opposite side. This study aims to analyze the risk factors and the correlation between osteoporosis and SHF on the opposite side in order to assess the usefulness of bisphosphonate treatment for the prevention of SHFs.
Materials and Methods
We included 517 patients treated from March 1997 to April 2009 in this study. The inclusion criteria included previous unilateral hip fracture, without osteoporotic treatment, and a T-score less than -3.0 at the time of the fracture. We studied these patients in terms of death, SHF, alcoholism, living alone, dementia, dizziness, health status, osteoporotic treatment after fracture and bone mineral density (BMD). In total, 34 patients experienced a SHF. We selected another 34 patients without a SHF who had similar age, sex, body mass index, BMD, diagnosis, treatment and a follow up period for a matched pair study. We compared these two groups. The average follow up was 8.3 years and 8.1 years, respectively.
Results
The mortality rate of the 517 patients was 138 (27%). The BMD at the time of fracture demonstrated no statistical difference between the two groups (p>0.05). Nine patients (26%) within the SHF group were prescribed Risedronate and 18 patients (53%) received the same treatment in the non-SHF group. There was a statistical relationship with the treatment of osteoporosis (p=0.026). The average BMD of patients with SHF was -5.13 and -5.02 in patients without SHF was (p>0.05).
The incidence of hip fracture is increasing due to an increase in elderly populations. It is expected that 63 million hip fractures will occur globally in 2050, and Melton, et al.1 reported that 6% of males and 17.5% of females will experience hip fracture.2 Hodsman, et al.3 reported that patients with previous hip fractures will experience subsequent hip fractures in the same region. They also suggested that the mortality is 2.7 times higher in these patients than the group without previous fractures.4 There are numerous reports regarding the seriousness of hip fractures; however, it is difficult to find information on the treatment of osteoporosis, which is the leading cause of hip fractures. Bone mineral density (BMD) is the most important factor in predicting the strength of bone, and the risk of fracture is higher when BMD is low and age is higher. Despite this fact, only a few patients receive osteoporotic treatment after evaluation of BMD.5,6 The authors studied patients who were treated for a hip fracture, grouping the patients with subsequent hip fracture (SHF) and those without SHF of the contralateral hip joint. We analyzed the risk factors of SHF and the effect of osteoporosis treatment on the prevention of SHF.
In total, we analyzed 517 patients treated from March 1997 to April 2009. The inclusion criteria included patients who had ipsilateral hip fracture with a T-score of BMD lower than -3.0 and who received no osteoporosis treatment at the time of the incident. Exclusion criteria included patients who had a T-score of BMD more than -3.0, patients who received osteoporosis treatment at the time of the incident, and patients whose cause of hip fracture was not a traffic accident, fall from more than height, or pathologic fracture. The average follow up period was 8.1 years (2-14 years). Patient survival, presence of SHF, alcohol history, marriage status, dementia, dizziness, osteoporosis treatment after fracture, and BMD were collected via the patients' medical records and telephone interviews. BMD tests were performed on all patients 2 weeks after trauma with Dual-energy X-ray absorptiometry (DEXA, Lunar, GE, Milwaukee, WI, USA). An annual follow up was done in 190 patients who underwent osteoporosis treatment. We included 34 patients (6.6%) with a previous history of surgery due to ipsilateral hip fracture and who had SHF on the contralateral side in the SHF group. In order to limit statistical bias using a matched pair study, we also included 34 patients without a contralateral hip fracture in the non-SHF group considering their age, sex, body mass index (BMI), BMD, diagnosis, surgical method, and follow up period. t-tests were performed for the two groups for age, BMI, BMD and follow up period. No statistical difference was found (p>0.05) after a chi-square test on age, diagnosis and surgical method. We also analyzed factors known to cause SHF such as additional fractures, alcohol consumption, solitude habitation, dementia, dizziness, medical condition, and history of osteoporosis treatment.
Ten males and twenty four females had a SHF and their ages at the time of the first fracture was 75.1 (65-86) and 79.3 (68-89) years, respectively, at the time of SHF on average. The interval between the first fracture and the SHF was 4.2 years (8 months-9 years) on average. Among the 34 patients who had a SHF, a femur neck fracture was the first fracture in 17 patients (50%), while 13 patients (38%) experienced an intertrochanteric fracture and 4 patients (12%) experienced a subtrochanteric fracture. Sixteen patients received a total hip replacement arthroplasty (THRA), while 7 patients had dynamic hip screws, 7 patients had intramedullary nails and 4 patients underwent axial pinning. Twenty patients (59%) had a femur neck fracture as a SHF, 10 patients (29%) had an intertrochanteric fracture, and a subtrochanteric fracture was noted in 4 patients (12%). Of these, 18 patients received a THRA, while 6 patients had dynamic hip screws, 6 patients had intramedullary nails and 4 patients underwent axial pinning. A Pearson chi-square test, Mann-Whitney test and a Fisher's exact test were used as statistical methods.
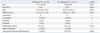
The mortality rate was 27%, as 138 of the 517 patients had died. The average age was 75.8 (56-96) years for 148 males and 369 females with an average BMI of 20.2 (15.1-31.4). In total, 34 patients (6.6%) experienced a SHF, and 76 patients (15%) experienced a trauma other than a hip fracture, alcoholism was noted in 7 patients (1%), 94 patients (18%) lived alone, 41 patients (8%) suffered from dementia, and dizziness was noted in 20 patients (4%). Their American society of anesthesiologists (ASA) physical status was 1.9 [1-4 standard deviation (SD) 0.7] on average. The average T-score at the time of initial trauma was -5.09 (-3.0 - -6.8, SD 0.37), while an average T-score of -5.29 (-2.4 - -6.9, SD 0.35) was recorded at the final follow up. A total of 190 patients (37%) received osteoporosis treatment after the initial fracture and their mean T-score was -5.15 (-3.0 - -6.8, SD 0.35) initially and -4.92 (-2.4 - -6.7, SD 0.41) at the final follow up. The 34 patients who experienced a SHF had an initial T-score of -5.13 (-3.2 - -6.6, SD 0.34), and a T-score of -5.48 (-3.5 - -6.8, SD 0.38) at the time of the SHF. The 483 patients without a subsequent fracture had T-scores of -5.03 (-3.0 - -6.8, SD 0.37) initially and a T-score of -5.28 (-2.4 - -6.9, SD 0.36) at the final follow up (Table 1).
Among the 34 patients with a SHF, 5 patients (15%) experienced a distal radius fracture. There were no reports of alcoholism in cases with a SHF; however, for those that did have a SHF, 5 (15%) were living alone, 3 (9%) had dementia, and 3 (9%) reported dizziness. Their ASA physical status score was 1.8 (1-4, SD 0.7) on average. The group without a SHF comprised 4 cases (12%) of distal radius fractures, 2 cases (6%) of lumbar compression fractures, 6 cases (18%) lived alone, 2 cases (6%) had dementia, 3 cases (9%) reported dizziness and there were no alcoholism cases. Their ASA physical status score was 1.6 (1-4, SD 0.5) on average. The two groups demonstrated no statistical differences for other area fractures, alcoholism, living alone, dementia, dizziness and presence of a medical condition. The initial T-score in the group with SHF was -5.13 (-3.2 - -6.6, SD 0.34), while the non SHF group recorded a T-score of -5.02 (-3.2 - -6.8), which had no statistical difference (p>0.05) (Table 2). Nine patients in the SHF group were prescribed Risedronate, which belongs to the bisphosphonate group, after initial trauma, while 18 patients in the non SHF group received the same medication. This was statistically different between the two groups (p=0.026).
The occurrence of fracture near the hip joint is increasing as the average life span increases due to medical improvement. However, mortality rates and complication rates are very high regardless of technological advances.7-9 Boston10 reported that, in the cases of a first femoral neck fracture, the death rate rose to 13% and 30% in cases of a second fracture. Our own research too demonstrated a high mortality rate ratio of 27%. The mortality rate was high due, first, to the ASA physical status, with scores as low as 1.6 on average in cases of patients with the first fracture. Secondly, we, as a university medical institution, encountered patients mostly with internal complications, who are difficult to treat. Although it is correct to say that the decrease in BMD near the hip joint has a strong correlation with bone strength and fracture status of bones, the following components are also known to be important factors: age, gender, alcohol addiction, history of fracture(s), solitude habitation, dementia and injuries from falls.11-14 Our data did not find any statistical differences for these factors, which are known to affect the recurrence of fractures, between the two groups studied. This is probably due to the low number of the target pool in each group. Jung, et al.15 stated that, while revealing no epidemiological and physical differences in an osteoporosis group with a history of fractures and an osteoporosis group without such history, patients within the range of osteoporosis had a high risk of fracture, even in those without any risk factors, regardless of the existence of the fracture. In 1994, the WHO defined a T-score of equal to or less than -2.5 as osteoporosis and the same T-score with a history of fractures as severe osteoporosis. Currently, domestic medical insurance states that a T-score equal to or less than -3.0 falls within insurance coverage range and this deserves critical review and modification if the characteristics of osteoporosis, of which prevention is more important, are considered. Jang, et al.16 and his associates claimed that the risk of fracture near the hip joint increases if the T-score drops below -1.5, which was at an intersection for each group.17 Our data suggested that the treatment for osteoporosis has not properly been performed, as we encountered 517 hip fracture patients who had never had any medical care or treatment before, even though their T-scores were as low as -5.09 on average at the time of trauma. Problems arise not only with the hip fracture itself due to osteoporosis, but also a resultant long-term stay at the hospital, rehabilitation, and an increase in the mortality rate resulting from localized or systemic complications are of concern.8-10 McClung, et al.18 reported the effectiveness of Risedronate in preventing fractures near the hip joint in a case of an aged woman who was diagnosed with osteoporosis. Bilezikian19 also reported a decrease in fractures near the hip joint in osteoporosis patients administered Risedronate. Our research found a statistically significant result in recurrence prevention of fractures near the hip joint with the use of Risedronate after first-time fractures near the hip joint. Although Kanis, et al.20 and his associates claimed that there is a correlation between a low BMD and recurrence of fractures in all age groups, as age increases, the ratio of morbidity accompanied by other diseases also increases, and this results in less importance of a low BMD that is contributed from many other risk factors of fracture, especially in an old population. In our research, as both groups demonstrated little difference in low BMD and the ratio of morbidity accompanied by other disease and the correlation with other risk factors were relatively low, we were able to verify the effectiveness of treatment with Risedronate in the bisphosphonate group in preventing SHF. There were a few limitations to the current study. First, the source of our data was limited to only one medical institution, so that the number of patients was quite small. We would expect more detailed data and results if we are able to co-work with other medical institutions regarding this subject. Second, we did not identify other causes of fragility fracture in terms of calcium profile, hormonal status, and vitamin D deficiency etc.
In conclusion, there are numerous factors related to decrease of SHF due to osteoporosis. In this study, the effect of treatment with bisphosphonates or Risedronate was superior to others. In the patients with hip fractures, the authors suggest that the treatment of osteoporosis to prevent SHF is as important as primary surgical intervention (Fig. 1).
Figures and Tables
Fig. 1
A 69-year old woman had a subsequent fracture on the left side after a right side intertrochanteric fracture (initial T-score -5.3). (A) Initial radiographs of right hip side intertrochanteric fracture. (B) Postoperative radiograph after a bipolar hemiarthroplasty. (C) Radiographs of subsequent fracture in the left femur neck (T-score -5.7 with patient who did not have treatment for osteoporosis). (D) Postoperative radiograph after a bipolar hemiarthroplasty. The patient started medication for osteoporosis.
References
1. Melton LJ 3rd, Chrischilles EA, Cooper C, Lane AW, Riggs BL. Perspective. How many women have osteoporosis? J Bone Miner Res. 1992. 7:1005–1010.

2. Cooper C, Campion G, Melton LJ 3rd. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992. 2:285–289.

3. Hodsman AB, Leslie WD, Tsang JF, Gamble GD. 10-year probability of recurrent fractures following wrist and other osteoporotic fractures in a large clinical cohort: an analysis from the Manitoba Bone Density Program. Arch Intern Med. 2008. 168:2261–2267.

4. Lee SR, Kim SR, Chung KH, Ko DO, Cho SH, Ha YC, et al. Mortality and activity after hip fracture: a prospective study. J Korean Orthop Assoc. 2005. 40:423–427.

5. Gardner MJ, Brophy RH, Demetrakopoulos D, Koob J, Hong R, Rana A, et al. Interventions to improve osteoporosis treatment following hip fracture. A prospective, randomized trial. J Bone Joint Surg Am. 2005. 87:3–7.
6. Juby AG, De Geus-Wenceslau CM. Evaluation of osteoporosis treatment in seniors after hip fracture. Osteoporos Int. 2002. 13:205–210.

7. Cummings SR, Kelsey JL, Nevitt MC, O'Dowd KJ. Epidemiology of osteoporosis and osteoporotic fractures. Epidemiol Rev. 1985. 7:178–208.

8. Eastwood EA, Magaziner J, Wang J, Silberzweig SB, Hannan EL, Strauss E, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002. 50:1240–1249.

9. Melton LJ, Riggs BL Jr. Kleerekoper M, Krane SM, editors. Further characterization of the heterogeneity of the osteoporotic syndromes. Proceedings of the International Symposium on Clinical Disorders of Bone and Mineral Metabolism. 1989. New York: Mary Ann Liebert, Inc.;145–152.
11. Bell GH, Dunbar O, Beck JS, Gibb A. Variations in strength of vertebrae with age and their relation to osteoporosis. Calcif Tissue Res. 1967. 1:75–86.

12. Carter DR, Hayes WC. Bone compressive strength: the influence of density and strain rate. Science. 1976. 194:1174–1176.

13. Ryg J, Rejnmark L, Overgaard S, Brixen K, Vestergaard P. Hip fracture patients at risk of second hip fracture: a nationwide population-based cohort study of 169,145 cases during 1977-2001. J Bone Miner Res. 2009. 24:1299–1307.

14. Cook PJ, Exton-Smith AN, Brocklehurst JC, Lempert-Barber SM. Fractured femurs, falls and bone disorders. J R Coll Physicians Lond. 1982. 16:45–49.
15. Jung ES, Lee YK, Baek SI. Diffrences of bone mineral density between osteoporotic group with or without compression fracture of the spine. J Korean Soc Fract. 1998. 11:629–633.

16. Jang J, Kim WL, Kang SB, Lee JH, Yoon KS. The relationship of osteoporosis and hip fractures in elderly patients. J Korean Hip Soc. 2008. 20:299–304.

17. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis. Report of a WHO Study Group. World Health Organ Tech Rep Ser. 1994. 843:1–129.
18. McClung MR, Geusens P, Miller PD, Zippel H, Bensen WG, Roux C, et al. Hip Intervention Program Study Group. Effect of risedronate on the risk of hip fracture in elderly women. N Engl J Med. 2001. 344:333–340.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download