Abstract
Purpose
Facial paralysis is an uncommon but significant complication of chronic otitis media (COM). Surgical eradication of the disease is the most viable way to overcome facial paralysis therefrom. In an effort to guide treatment of this rare complication, we analyzed the prognosis of facial function after surgical treatment.
Materials and Methods
A total of 3435 patients with COM, who underwent various otologic surgeries throughout a period of 20 years, were analyzed retrospectively. Forty six patients (1.33%) had facial nerve paralysis caused by COM. We analyzed prognostic factors including delay of surgery, the extent of disease, presence or absence of cholesteatoma and the type of surgery affecting surgical outcomes.
Results
Surgical intervention had a good effect on the restoration of facial function in cases of shorter duration of onset of facial paralysis to surgery and cases of sudden onset, without cholesteatoma. No previous ear surgery and healthy bony labyrinth indicated a good postoperative prognosis.
Conclusion
COM causing facial paralysis is most frequently due to cholesteatoma and the presence of cholesteatoma decreased the effectiveness of surgical treatment and indicated a poor prognosis after surgery. In our experience, early surgical intervention can be crucial to recovery of facial function. To prevent recurrent cholesteatoma, which leads to local destruction of the facial nerve, complete eradication of the disease in one procedure cannot be overemphasized for the treatment of patients with COM.
Facial nerve paralysis is an uncommon but significant complication of chronic otitis media (COM). Although the incidence of facial nerve paralysis has decreased with the use of antibiotics, prevention thereof remains a challenging problem. It has been reported that the frequency of facial nerve paralysis in COM ranges from 0.16 to 5.1%.1-3
Although the mechanism of facial nerve paralysis, as a result of COM, is not fully understood, treatment recommendations have focused on both antibiotic treatment as well as surgery, including myringotomy, mastoidectomy and nerve decompression, in order to reestablish the physiological state of the facial nerve.4-6
Surgical eradication of the disease is the most viable way to overcome facial nerve paralysis; however, there is a lack of data from which to draw significant conclusions on the surgical management thereof. The variance in application of surgical treatment for these patients stems from the lack of predictors for facial nerve paralysis remission.7-10
The present study describes our experience with diverse clinical features of facial nerve paralysis, in an effort to guide treatment of this rare complication. Also, we analyzed prognostic factors, including delay of surgery, extent of disease, presence or absence of cholesteatoma and type of surgery, affecting surgical outcomes.
A total of 3435 patients with COM, with or without cholesteatoma, who underwent canal down mastoidectomy, intact canal wall mastoidectomy or excision via a translabyrinthine approach, throughout a period of 20 years (between January 1988 and December 2008), were analyzed retrospectively. Forty six patients (1.33%) had facial nerve paralysis caused by COM with or without cholesteatoma. Data were collected concerning the patients' age upon presentation, sex, clinical presentation, cholesteatoma location, preoperative and postoperative facial nerve function and follow-up. Computed tomography was obtained in all cases. Magnetic resonance imaging was available in several cases. The severity of facial nerve paralysis was graded using the House-Brackmann (HB) grading system.11
Surgery was performed as early as possible in 46 patients using the transmastoid and translabyrinthine approach. Total removal of the cholesteatoma lesion and management of the facial nerve were performed using various surgical techniques depending on location and severity.
Facial nerve decompression was performed in 42 patients with opening of the epineural sheath, if there was facial nerve edema or redness. Medical therapy in combination with surgery included antibiotic and steroid treatment (60 mg/d initial dose with tapering) in patients with abrupt onset of edema.
Four patients had aggressive cholesteatomas with complete facial nerve paralysis, and facial nerve interruption or replacement with fibrous tissue was found in the operative field. If complete removal of the cholesteatoma was impossible, the injured segment by cholesteatoma was resected and facial nerve endings were revived. Also, fibrous segments were excised followed by facial nerve repair according to the size of the defect.
All patients were informed of possible surgical complications and the limited reversibility of good facial nerve function. Recovery of facial nerve function was assessed no earlier than 1 year after surgical intervention.
Patients who had facial paralysis due to COM were operated on as early as possible in order to remove the pathologic tissue. The severity of facial function, the presence of cholesteatoma, type of onset, age, any previous otologic surgical history and duration from onset had no effect on deciding surgical timing.
For patients who had previously undergone a mastoidectomy procedure to remove cholesteatoma, the complete removal of cholesteatoma was thought to be as equally as important as the preservation of facial function. Exploration of the facial nerve was often difficult due to distorted surgical landmarks and adhesive or fibrotic change caused by previous surgery. Intraoperative facial nerve monitoring can be used to confirm the location of the facial nerve, and the unchanged location of surgical landmarks, including the stylomastoid foramen and the fundus of the internal auditory canal, were used to find the facial nerve.
In cholesteatoma surgery, dissection of the cholesteatomatous matrix from soft tissues, such as the dura, sigmoid sinus, jugular bulb, internal carotid artery including the facial nerve, was conducted carefully with wide bony removal. If complete removal was not possible, resection of the injured segment by cholesteatoma was thought to be the only sure alternative for complete removal of the pathology.
As the dissection and removal of the cholesteatomas approached the semicircular canals and cochlear, we expected that a labyrinthine fistula may be present. Dissection over these areas was performed cautiously and delicately to avoid damage to the inner ear. When a fistula was encountered, removal of the basement membrane from the endosteal lining of the inner ear was conducted, if the removal met no resistance. However, in cases where the basement membrane of squamous epithelium was not easily detached from the endosteal membrane or when it was clear that the fistula was very large, an island of the basement membrane was trimmed away from that which had already been dissected free and left over the fistula until the cholesteatoma could be totally removed from the mastoid and fallopian canal.
Accurate assessment of facial nerve status was obtained intraoperatively. Four different conditions of the facial nerves were observed among the patients, including a compressed but normal segment, a reddish edematous segment, a fibrosed segment and an interrupted nerve.
Edematous and compressed nerves were managed by decompression and removal of the overlying cholesteatoma matrix or infected granulation tissue.
If the facial nerve was found to be interrupted or fibrosed during surgery, the segments involved and adequate margins were cut away. Continuity of the facial nerve was restored by rerouting direct anastomosis, only if the available length of the remaining nerve was sufficient to achieve a tension-free anastomosis or by a graft, if it was impossible.
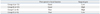
On the basis of post-operative facial function and surgical gain, 46 patients were divided into 4 groups for the detailed analysis of their prognoses.
Facial nerve paralysis of HB Grade II was considered to have good facial function. The gain in facial function was calculated by subtracting the final grading score from the initial grading score. High surgical gain was defined as an improvement in facial function of more than two grades on the HB scale after surgical intervention.
1. Group A (n=11) included patients who had good preoperative facial function and good post-operative facial function. All patients in Group A had well-preserved facial function.
2. Group B (n=23) included patients who had poor preoperative facial function (less the HB Grade II), but had good post-operative facial function. All patients in Group B had much improved facial function.
3. Group C (n=4) included patients who had a gain in facial function of more than two grades on the HB scale after surgery, but had poor post-operative facial function. All patients in Group C had improved but slightly defective facial function.
4. Group D (n=8) included patients who had a gain of facial function less than two grades on the HB scale after surgery and had poor post-operative facial function. All patients in Group D had improved but severely defective facial function.
Ages of the patients with facial paralysis ranged between 19 and 74 years with an average age of 44 years. The male to female ratio was 1 : 1. Two (4%) patients were in the first decade, 4 (9%) in second, 7 (15%) in third, 15 (33%) in fourth, 8 (17%) in fifth, 5 (11%) in sixth, and 5 (11%) in seventh decade of their lives. The duration from the onset of paralysis to surgery ranged from 4 days to 1 year. In 15 patients (33%), the duration was less than 1 week; in 18 patients (39%), it was 1-2 weeks; in 8 (17%), it was 2-4 weeks; in 3 (7%), it was 1-6 months; and in 2 (4%), it was 6-12 months.
The onset of facial nerve paralysis was sudden in 27 patients (59%) and gradual in 19 patients (41%) (slowly progressive pattern worsening within a week). The initial grade of facial nerve paralysis according to the HB grading system was II in eleven patients, III in seven, IV in seven, V in seventeen, VI in four patients.
Sensorineural hearing loss due to labyrinthitis was present in 8 patients (17%), 5 of whom (11%) were totally deaf. The common symptoms associated with facial nerve paralysis were otorrhea in 9 patients, vertigo in 6 patients, tinnitus in 4 patients and otalgia in 3 patients. Twenty-six patients had no associated symptoms.
Twenty-seven patients (59%) had cholesteatoma and nineteen patients (41%) had no cholesteatoma. Twenty four patients (52%) underwent canal wall down mastoidectomy, fourteen patients (30%) underwent intact canal wall mastoidectomy, four patients (9%) underwent modified radical mastoidectomy, and four patients (9%) underwent labyrinthectomy. Forty two (91%) patients underwent facial nerve decompression from the geniculate ganglion to the stylomastoid foramen with or without epineural incision, which was determined after examining the pathologic states of the facial nerve in the surgical field. Two patients (4.5%) underwent direct end-to-end neural anastomosis and two patients (4.5%) underwent neural graft with great auricular nerve after the resection of disease-involved segments.
Intraoperatively, 41 patients (88%) presented fallopian canal destruction or dehiscence, whereas the facial nerve canal was intact in five patients (12%) (none of them had a cholesteatoma). The tympanic segment was the most common site of disease involvement in 38 patients (83%), and of these patients, 14 patients had exposure on the mastoid segment. Two patients had geniculate ganglion exposure, and two other patients had labyrinthine segment exposure. There was a large defect of the mastoid segment in four patients.
All patients had facial nerve paralysis of HB Grade II preoperatively. The mean duration of the onset of paralysis to surgery was 11.0±7.32 days. The onset of facial nerve paralysis was sudden in 8 patients and gradual in 3 patients. There was one patient who had previous ear surgery for COM. Five patients had cholesteatoma and six patients had infected granuloma without cholesteatoma. In addition to destruction of the fallopian canal, destruction of the bony labyrinth was observed in 3 patients, resulting in exposure of the semicircular canal and vestibular membranous labyrinth. The pathologic findings of the facial nerve were edema and redness in 11 patients. The tympanic segment was the most common site of disease involvement in 11 patients. Facial nerve decompression via a transmastoid approach with or without epineural incision was conducted in all cases. All patients had complete recovery of their facial function after surgery with an HB grade of Grade I.
All patients had good recovery of facial function with an HB grade of Grade I or Grade II after surgery. The mean age of the patients was 47.2±6.43 years. The mean duration of the onset of paralysis to surgery was 13.9±7.24 days. The onset of facial nerve paralysis was sudden in 17 patients and gradual in 6 patients. There were six patients who had previous ear surgery for COM.
Eleven patients had cholesteatoma and twelve patients had infected granuloma without cholesteatoma. In addition to destruction of the fallopian canal, destruction of the bony labyrinth was observed in 14 patients. The pathologic findings of the facial nerve were edema and redness in 19 patients and were normal in 4 patients.
The tympanic segment was the most common pathologic segment in 18 patients, 9 patients also had exposure on the mastoid segment and 1 patient on geniculate ganglion. Facial nerve decompression via a transmastoid approach was conducted in all cases.
All patients demonstrated a post-operative facial function of HB Grade III or IV despite much improved facial function (greater than two grades on the HB scale). The mean age of the patients was 39.3±13.2 years. The mean duration of the onset of paralysis to surgery was 4.2±3.7 months. The onset of facial nerve paralysis was gradual in all patients. There were three patients who had previous ear surgery for COM.
All patients had cholesteatoma. In addition to destruction of the fallopian canal, destruction of the bony labyrinth was observed in 3 patients. The pathologic findings of the facial nerve were reddish edema in 3 patients and interruption in 1 patient.
The tympanic segment was the most common site of involvement in all patients, while 2 patients also had exposure on the mastoid segment, 1 patient on labyrinthine segment and 1 patient on geniculate ganglion. Facial nerve decompression via a transmastoid approach was conducted in 2 cases, end-to-end anastomosis in 1 case and nerve graft in 1 case.
All patients did not demonstrate high surgical gain of facial function after surgery (less than two grades on the HB scale). The mean age of the patients was 40.9±8.08 years. The mean duration of the onset of paralysis to surgery was 3.5±2.25 months. The onset of facial nerve paralysis was sudden in 2 patients and gradual in 6 patients. There were four patients who had previous ear surgery for COM.
Seven patients had cholesteatoma and one patient had infected granuloma without cholesteatoma. In addition to destruction of the fallopian canal, destruction of the bony labyrinth was observed in 7 patients. The pathologic findings of the facial nerve were edema in 4 patients, interruption in 1 patient and fibrosis in 2 patients.
Facial nerve decompression via a transmastoid approach was conducted in 6 cases, end-to-end anastomosis in 1 case and nerve graft in 1 case.
Pre-operative facial function was divided into good facial function (HB grade ≤2) and poor facial function (HB grade ≥3). Longer durations of facial dysfunction, increased facial deterioration (p<0.05, chi-square test) and destruction of bony labyrinth were more readily found in patients with poor facial function than in patients with good facial function (p<0.05, unpaired t-test). Other factors including age, previous ear surgery, type of onset and cholesteatoma were not related to the severity of preoperative facial function.
Surgical gain was calculated by subtracting the final HB grading score from initial HB grading score and was evaluated by comparing those with high surgical gain (functional gain of HB grade ≥2) to those with low surgical gain (functional gain of HB grade <2). Surgical intervention had a good effect on restoration of facial function in cases of shorter durations of onset of facial paralysis to surgery (p<0.05, chi-square test) and cases of sudden onset, without cholesteatoma (p<0.05, unpaired t-test). Other factors including age, previous ear surgery and destruction of bony labyrinth proved not to affect the degree of functional gain after surgery.
Postoperative prognosis was defined as good prognosis (postoperative HB grade ≤2) and poor prognosis (postoperative HB grade ≥3). Good postoperative prognosis could be expected in cases of COM with short durations of onset of facial nerve paralysis (p<0.05, chi-square test), absence of previous ear surgery, sudden onset, non-cholesteatomatous inflammatory granulation tissue and healthy bony labyrinth (p<0.05, unpaired t-test). Age was not related to the prognoses after surgery.
When considering facial nerve paralysis caused by COM, several questions arise concerning the management and prognosis thereof, as knowledge on the pathogenesis of otitic facial nerve paralysis is unclear.
Osteitis, bone erosion, external compression, edema and inflammation of the nerve are some of the proposed etiologic factors.8,12 However, the pathologic condition of COM leading to facial nerve paralysis needs to be clarified in order for proper management and greater functional restoration.
Chronic otitis media causing facial nerve paralysis is most frequently due to cholesteatoma. Cholesteatoma was observed in 51/64 patients (80%) with chronic otitis media causing facial paralysis in a study by Savić and Djerić,2 in 14/20 (70%) by Altuntas, et al.13 and in 16/24 (67%) by Yetiser, et al.7 However, our evaluation showed cholesteatoma in 27/46 patients (59%) with facial nerve paralysis, and the severity of facial nerve paralysis due to cholesteatoma varied. Notwithstanding, the presence of cholesteatoma decreased the effectiveness of surgical gain and indicated a poor prognosis after surgery. It is thought that direct inflammation of the nerve, by bacteria or by neurotoxic substances secreted from the cholesteatoma matrix, is the leading factor causing deterioration. Therefore, the complete removal of the cholesteatoma matrix can be helpful not only for better recovery of the injured nerve, but also for prevention of additional ear surgery due to recurrence of the cholesteatoma. Burggraaff, et al.14 reported 13 cases of cholesteatoma that had spread to the cranial cavity and 12 of which had previously undergone a mastoidectomy procedure for the removal of cholesteatoma. In this study, 14/46 patients (33%) had a history of middle ear surgery, and previous ear surgery had led to incomplete restoration of the facial nerve. Complete eradication of cholesteatoma in one procedure is compulsory for the welfare of the facial nerve.
With regard to the duration of onset of facial paralysis to surgery, the surgical timing had been thought to be an important factor as reported by Ikeda, et al.15 Also in our study, the outcome of surgical intervention was closely related to the duration of onset to surgery. Longer durations can cause more severe deterioration of the facial nerve and poor surgical outcomes. Patients with facial paralysis due to COM should be operated on as early as possible, regardless of the severity of facial function, the presence of cholesteatoma, type of onset, age and any previous otologic surgical history.
Facial nerve paralysis due to COM may be either abrupt or gradual in onset. Abrupt onset results from an acute infectious exacerbation superimposed on the COM, while gradual onset typically results from compression from a cholesteatoma or granulation tissue. However, severe dysfunction can also be caused by interruption or fibrosis of the facial nerve. Direct anastomosis or nerve grafts for those with short durations of facial paralysis provide the best chance for recovery of nerve function. Decisions on cutting edges and cleaning uncovered facial nerves should be prudent during the resection of fibrotic or interrupted neural patency. In our experience, careful management with early surgical intervention can has had a decisive effect on the recovery of facial function.
Some authors attempted to remove only the epineurium if it was invaded and always left the perineurium intact, as the perineurium was thought to provide an effective barrier to infection.13 However, we opened the epineurium in a limited area where there was severe redness and edema of the facial nerve with limited exposure as a relieving effect after complete eradication of the infectious origin. None of the cases demonstrated any worsening of due to surgery.
In conclusion, COM resulting in facial nerve paralysis is most frequently due to cholesteatoma, and the presence of cholesteatoma decreased the effectiveness of surgical gain indicating poor prognoses after surgery. The complete removal of the cholesteatoma matrix with long durations of paralysis onset are not helpful for a better recovery of the injured nerve, but rather only to prevent additional ear surgery due to recurrence of the cholesteatoma. Careful management with early surgical intervention has proven to have a decisive effect on the recovery of facial function. To prevent recurrent cholesteatoma, which leads to local destruction of bony labyrinth and facial nerve, complete eradication of the disease in one procedure cannot be overemphasized for the treatment of patients with facial nerve paralysis due to COM.
Figures and Tables
References
1. Pollock RA, Brown LA. Graham MD, House WF, editors. Facial paralysis in otitis media. Disorders of the facial nerve. 1982. New York: Raven Press;221–224.
2. Savić DL, Djerić DR. Facial paralysis in chronic suppurative otitis media. Clin Otolaryngol Allied Sci. 1989. 14:515–517.

3. Kangsanarak J, Fooanant S, Ruckphaopunt K, Navacharoen N, Teotrakul S. Extracranial and intracranial complications of suppurative otitis media. Report of 102 cases. J Laryngol Otol. 1993. 107:999–1004.

4. Fliss DM, Leiberman A, Dagan R. Medical sequelae and complications of acute otitis media. Pediatr Infect Dis J. 1994. 13:1 Suppl 1. S34–S40.

5. Ellefsen B, Bonding P. Facial palsy in acute otitis media. Clin Otolaryngol Allied Sci. 1996. 21:393–395.

6. Elliott CA, Zalzal GH, Gottlieb WR. Acute otitis media and facial paralysis in children. Ann Otol Rhinol Laryngol. 1996. 105:58–62.

7. Yetiser S, Tosun F, Kazkayasi M. Facial nerve paralysis due to chronic otitis media. Otol Neurotol. 2002. 23:580–588.

8. Harker LA, Pignatari SS. Facial nerve paralysis secondary to chronic otitis media without cholesteatoma. Am J Otol. 1992. 13:372–374.
9. Henderson PE, Baldone SC. Facial nerve palsy secondary to acute otitis media. J Am Osteopath Assoc. 1989. 89:207–210.

10. Edmond CV Jr, Antoine G, Yim D, Yoshida G, Gonzalez C. A case of facial diplegia associated with acute bilateral otitis media. Int J Pediatr Otorhinolaryngol. 1990. 18:257–262.

11. House JW, Brackmann DE. Facial nerve grading system. Otolaryngol Head Neck Surg. 1985. 93:146–147.

12. Chu FW, Jackler RK. Anterior epitympanic cholesteatoma with facial paralysis: a characteristic growth pattern. Laryngoscope. 1988. 98:274–279.
13. Altuntas A, Unal A, Aslan A, Ozcan M, Kurkcuoglu S, Nalca Y. Facial nerve paralysis in chronic suppurative otitis media: Ankara Numune Hospital experience. Auris Nasus Larynx. 1998. 25:169–172.

14. Burggraaff B, Luxford WM, Doyle KJ. Neurotologic treatment of acquired cholesteatoma. Am J Otol. 1995. 16:480–485.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download