Abstract
Purpose
To analyze the effectiveness of anterior pelvic plating and subsequent percutaneous sacroiliac joint screw fixation in patients with unstable pelvic ring injuries.
Materials and Methods
Thirty-two patients were included with twenty-one males and eleven females. The mean age was 41 years (range, 19-76). The mean follow-up period was 51 months (range, 36-73). According to AO-OTA classification, there were 11 cases of B2 injuries, 8 cases of B3 injuries, 9 cases of C1 injuries, 2 cases of C2 injuries and 2 cases of C3 injuries. In the posterior lesions, there were 20 cases of sacral fractures and 12 cases of sacroiliac joint disruptions or dislocations. Anterior pelvic plating and subsequent percutaneous sacroiliac joint fixation were performed.
Results
The clinical results were 16 cases of excellent, 10 cases of good, 4 cases of moderate and 2 cases of poor functional results. The 2 cases out of 7 moderate reductions had poor functional results with residual neurologic symptoms. The radiological results were 16 cases of anatomic, 9 cases of nearly anatomic and 7 cases of moderate reduction. All patients were healed except 3 cases of nonunion at the pubic ramus. The complications encountered were 3 cases of screw loosening, 2 cases of anterior plate breakage and 1 case of postoperative infection.
Unstable pelvic ring injuries are uncommon which are mainly caused by high energy injuries. They result in extensive disruption of the pelvis and high rates of mortality and late morbidity. They are frequently associated with various types of combined injuries. The conservative treatment of these injuries has been disappointing. Early rigid fixation and anatomical reduction of the pelvic ring are recommended to reduce mortality and allow early ambulation.1 The complicated vertical shear type of injury or an unstable lateral compression injury or external rotational instability requires anatomical reduction, anteriorly and posteriorly. Displaced unstable pelvic ring injuries are commonly associated with disruption of the osteoarticular junction of the sacroiliac joint, and stable fixation of sacroiliac joint is technically demanding while the stability of posterior pelvic ring is more important than that of anterior ring.
Anterior fixation can be stabilized by plating, which is the method of choice however, the surgical options for fixation of posterior lesion is still controversial. Plating or sacral bars have been widely used for posterior lesion but they need wide exposure which may be susceptible to infection and postoperative complications. In view of these problems, the percutaneous sacroiliac joint screw fixation is far less invasive technique than those of previous options which can be applied to sacroiliac joint disruption and sacral fractures commonly encountered in unstable pelvic ring injuries.
The purpose of our study was to evaluate the effectiveness of anterior pelvic plating and subsequent percutaneous sacroiliac joint screw fixation in patients with unstable pelvic ring injuries.
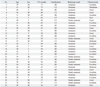
Thirty-two patients with unstable pelvic ring injuries who were followed more than 3 years were included. There were 21 males and 11 females with the mean age of 41 years (range, 19-76). The mean follow-up period was 51 months (range, 36-73) (Table 1). The mechanisms of injury were traffic accident in 20, fall from a height in 9 and crashed from falling objects in 3 cases. Seventeen patients (53%) out of 32 patients had associated injuries or other site fractures.
Initial radiologic assessments were anterior-posterior and inlet-outlet views of pelvis. Three dimensional pelvis CT scan was routinely performed to obtain more information about fracture pattern and operative plan. According to AO-OTA classifications,2 11 cases of B2, 8 cases of B3, 9 cases of C1, 2 cases of C2 and 2 cases of C3. In the posterior lesions, there were 20 cases of sacral fractures (6 in type I and 14 in type II in the Denis3 classification) and 12 of sacroiliac joint disruptions or dislocations. Six patients had existing neurologic symptoms at the time of injury.
The mean duration from injury to surgery was 4.2 days (range, 0-11). Eight patients (25%) were operated within post-injury 24 hours. Twenty-two patients (69%) were operated within post-injury 10 days. We tried to stabilize the pelvic fractures as early as possible. Remaining 2 patients (6%) who were operated post-injury at 11 days were delayed due to severe combined injuries and intolerable conditions for surgery at the time of injury.
All patients were operated under general anesthesia on radiolucent table in a supine position. The leg on the injured side was draped freely, and both hips and knees were slightly flexed to relax the iliopsoas muscle. Our preferred surgical approach was the modified Stoppa4 approach. Modified Stoppa approach is limited, intra-pelvic approach. It leads to access the intra-pelvic aspect of the pelvis and acetabulum which is gained by retraction of the muscular, neurovascular and urologic structures. It offers the direct visualization of medal wall of acetabulum, entire pelvic ring, and sacroiliac joint which facilitates the development and utilization of improved reduction and plating options. Care must be taken not to injure the corona mortis, obturator nerve, and peritoneum. Through this approach, we could open injured site to obtain exact anatomical reduction with the assistance of intra-operative longitudinal traction and closed manipulation. We fixed anterior ring with single pelvic reconstruction plate and tried to fix at least three screws in each fractured segment (Fig. 1).
The posterior ring was indirectly reduced after procedure of anterior ring. Percutaneous sacroiliac joint fixation was performed with same patient's position. After obtaining the true lateral view with fluoroscope guide, the entry point of sacroiliac screw was determined at S1 body. Care should be taken not to injure the sacral canal or foramen with guidance of pelvic inlet and outlet views. After drilling over the guide pin, a single partially threaded cannulated screw (7.0 mm in diameter) with washer was inserted. The screw was long enough to pass the center of the sacral body. The cannulated screw was tightened till the fracture sites were approximately together (Fig. 1).
Postoperatively, passive motion of hip up to 45 degrees was started on the second or third day which was increased to 90 degrees over next 7 days. Active hip motions were started thereafter. Partial weight bearing using walking aids was allowed at postoperative 4-6 weeks. Then, full weight bearing began when a bony union was visible. Periodic follow-up radiographs of the anteroposterior, inlet and outlet views were checked at regular intervals of 4 weeks.
For radiologic assessments, we used the criteria of Matta and Saucedo5 grading system. It was graded as anatomic, nearly anatomic, moderate and poor. The location of sacroiliac screw was graded as adequate or inadequate position by intrusion into sacral canal or sacral foramen or not.
The clinical result was evaluated according to the criteria of Rommens and Hessmann6 which was graded as excellent, good, moderate and poor. We defined excellent or good as a satisfactory result and moderate or poor as an unsatisfactory result.
Statistical analysis was tested by Fisher's exact test and a p-value less than 0.05 was considered to be statistically significant.
All fractures except 3 cases were united within postoperative 16 weeks (range, 12-20 weeks). Three non-union occurred at anterior pubic ramus. Among them, 1 case of non-union (type C2) occurred with a plate breakage. Since it was asymptomatic, further procedure was not needed. The radiological results were 16 cases of anatomic, 9 cases of nearly anatomic and 7 cases of moderate. In the 7 cases of moderate reductions, 2 cases were inadequate reduction of posterior ring with persisting residual neurologic symptoms. The maximum average of displacement was 15.8 mm in 12 cases of sacroiliac joint disruptions or dislocations. It improved to 5.3 mm, postoperatively.
The clinical results revealed 26 cases of satisfactory (16 of excellent and 10 of good), and 6 cases of unsatisfactory results (4 of moderate and 2 of poor). In relation to radiological results, 25 cases which were above nearly anatomic reductions had satisfactory results, and 6 cases of moderate reductions had unsatisfactory clinical results (p<0.05). There were 2 cases of residual neurologic symptoms which coincided with unsatisfactory functional results.
With regard to postoperative complications, there were 3 cases of screw loosening (2 cases of anterior plate and 1 case of sacroiliac screw), 2 cases of anterior plate breakage and 1 case of postoperative infection. In 2 cases of screw loosening from anterior plate, re-operation was not needed since they were asymptomatic. One case of sacroiliac screw loosening showed mild loosening. Then, further management was not necessary. Among 2 cases of anterior plate breakage, 1 case was combined with non-union. One case of post-operative infection was healed with thorough debridement without plate removal.
The pelvic ring plays many important roles not only in accommodating the intra-pelvic organs but also bearing body weight and providing support to trunk and spinal column. It is, therefore, very essential to stabilize and restore the oval-shaped osseo-ligamentous structure of the pelvic ring. Several authors reported the results of conservative treatment including external fixation and surgical interventions.6-9 Most of stable pelvic ring injuries do not necessarily need surgical interventions and they are satisfactorily cured with conservative treatment. However, treatment of unstable pelvic ring injuries by conservative treatments needs a long hospital day and can lead to inaccurate reduction with high mortality rate.10 Surgical treatments, therefore, are advocated since they can promote early rehabilitation and decrease many complications.11
External fixation can be a kind of good option for pelvic ring injuries, and it can be applied rapidly and early in pelvic ring disruption. However, external fixation alone is not sufficient to stabilize the posterior lesion, and additional method must be needed. Open reduction and internal fixation which is more constructive treatment modality, can result in a satisfactory outcomes.5,6 In unstable pelvic ring injuries, anterior fixation alone may not be sufficient to reduce the posterior injury, and the additional fixation of the posterior lesion is recommended, especially vertical shear injuries.12 Sacral bars have many advantages for sacral fractures and sacroiliac joint dislocations. However, there is a risk of over-compression with nerve injury. Furthermore, bilateral ends of bar are so prominent that it can result in discomfort to patients.13 Anterior plating of sacroiliac joint can fix sacroiliac joint, however, surgical approach is limited and can injure 5th lumbar nerve root.14 Posterior plating of sacroiliac joint through posterior approach has the same biomechanical stability as sacral bars, but it can cause adverse effects such as bleeding, wound problem and postoperative infection.
The sacroiliac joint screw fixation can be applied to both sacral fractures and sacroiliac joint disruption. It is also minimally invasive technique with percutaneous fixation, and postoperative complications can be minimal. Furthermore, sacroiliac joint screw can be applied after anterior plating without changing patient's position as in our study.
To obtain an anatomical reduction of rotationally unstable pelvic ring injury, anterior plating can be a good surgical option.15 This is also important in vertically unstable pelvic ring injuries, since a satisfactory reduction of the posterior ring is the first step toward an accurate fixation of the sacroiliac screw. We strongly believe that anatomical reduction and satisfactory anterior plating can make sacroiliac joint screw fixation much easier. Unstable pelvic ring injuries have a tendency to re-displace if only the posterior ring is fixed. Anterior plate fixation is known to lower the rate of malunion.13 Sagi, et al.16 reported that anterior plating for the vertically unstable pelvis increases the stability of the fixation construct, and that there were no cases of further displacement after initial fixation and high rate of satisfactory results was obtained.
We obtained 7 cases of moderate reduction which were all type C pelvic ring injuries. Among them, 6 cases showed unsatisfactory clinical result except 1 case of good result. We believe that severities of initial injury are closely co-related with radiologic and clinical results.13,17 It has been assumed that residual neurologic symptom is an another causative factor affecting clinical outcome. Denis, et al.3 reported that nerve injuries of type C pelvic ring injuries are more severe than those in type B. There were 2 cases of persistent residual neurologic symptoms in this study which showed poor clinical results.
In conclusion, anterior pelvic plating combined with percutaneous sacroiliac joint screw fixation is effective treatment options for unstable pelvic ring injuries since it has shown a high rate of functional success and a low complication rate.
Figures and Tables
Fig. 1
(A and B) Plain radiograph and 3-D reconstructive CT scan of pelvis show bilateral ramus fractures, left-sided sacral fracture (type I) and right-sided iliac fracture. (C) Immediate postoperative X-ray shows anterior pelvic plating and sacroiliac joint screw fixation. Anatomical reduction is obtained. (D) Final radiograph shows well-maintained and complete union with excellent clinical result. CT, computed tomography.

References
2. Fracture and dislocation compendium. Orthopaedic Trauma Association Committee for Coding and Classification. J Orthop Trauma. 1996. 10:Suppl 1. v–ix. 1–154.
3. Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988. 227:67–81.
4. Hirvensalo E, Lindahl J, Böstman O. A new approach to the internal fixation of unstable pelvic fractures. Clin Orthop Relat Res. 1993. 28–32.

5. Matta JM, Saucedo T. Internal fixation of pelvic ring fractures. Clin Orthop Relat Res. 1989. 83–97.

6. Rommens PM, Hessmann MH. Staged reconstruction of pelvic ring disruption: differences in morbidity, mortality, radiologic results, and functional outcomes between B1, B2/B3, and C-type lesions. J Orthop Trauma. 2002. 16:92–98.

7. Suzuki T, Shindo M, Soma K, Minehara H, Nakamura K, Uchino M, et al. Long-term functional outcome after unstable pelvic ring fracture. J Trauma. 2007. 63:884–888.

8. Nepola JV, Trenhaile SW, Miranda MA, Butterfield SL, Fredericks DC, Riemer BL. Vertical shear injuries: is there a relationship between residual displacement and functional outcome? J Trauma. 1999. 46:1024–1029.
9. Smith W, Shurnas P, Morgan S, Agudelo J, Luszko G, Knox EC, et al. Clinical outcomes of unstable pelvic fractures in skeletally immature patients. J Bone Joint Surg Am. 2005. 87:2423–2431.

10. Stocks GW, Gabel GT, Noble PC, Hanson GW, Tullos HS. Anterior and posterior internal fixation of vertical shear fractures of the pelvis. J Orthop Res. 1991. 9:237–245.

11. Burgess AR, Eastridge BJ, Young JW, Ellison TS, Ellison PS Jr, Poka A, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990. 30:848–856.
12. Kellam JF, McMurtry RY, Paley D, Tile M. The unstable pelvic fracture. Operative treatment. Orthop Clin North Am. 1987. 18:25–41.
13. Keating JF, Werier J, Blachut P, Broekhuyse H, Meek RN, O'Brien PJ. Early fixation of the vertically unstable pelvis: the role of iliosacral screw fixation of the posterior lesion. J Orthop Trauma. 1999. 13:107–113.

14. Leighton RK, Waddell JP. Techniques for reduction and posterior fixation through the anterior approach. Clin Orthop Relat Res. 1996. 115–120.

15. Tornetta P 3rd, Dickson K, Matta JM. Outcome of rotationally unstable pelvic ring injuries treated operatively. Clin Orthop Relat Res. 1996. 147–151.

16. Sagi HC, Ordway NR, DiPasquale T. Biomechanical analysis of fixation for vertically unstable sacroiliac dislocations with iliosacral screws and symphyseal plating. J Orthop Trauma. 2004. 18:138–143.

17. Pohlemann T, Angst M, Schneider E, Ganz R, Tscherne H. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993. 7:107–117.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download