Abstract
Purpose
The present study was aimed to determine whether endoscopist specialty is associated with high-quality endoscopy.
Materials and Methods
We prospectively collected endoscopy quality related data based on the Endoscopy Quality Rating Scale (EQRS) of 277 endoscopy units in a hospital setting from the National Cancer Screening Program of Korea in 2009. Gastroenterology medical professors (n=154) from university hospitals visited each endoscopy unit and graded the unit according to the EQRS. The scores from the EQRS were analyzed and compared in relation to endoscopy training during residency and endoscopy subspecialist certification.
Results
After excluding data from 3 endoscopy units, EQRS data from 274 endoscopy units were analyzed: 263 esophagogastroduodenoscopy (EGD) screening units and 90 colonoscopy screening units. There were no significant differences in the scores of EQRS with respect to endoscopy training during residency (p=no significance), except for scores of EGDs for "Facility and Equipment" (p=0.030). However, EQRS scores were significantly higher in the endoscopy units where endoscopy subspecialists performed the endoscopies than those where Endoscopy Subspecialists did not perform the endoscopies (p<0.05, except p=0.08 for the "Process" criteria of EGD).
High-quality endoscopy ensures that patients receive with minimal risk their indicated procedure, correct and clinically relevant diagnoses, as well as properly performed therapy.1 In order to ensure high-quality endoscopy, it is essential to identify important clinical determinants that influence endoscopy quality.
According to each endoscopist, endoscopic diagnosis for the same lesions may differ. In clinical practice, the impact of endoscopists on high-quality endoscopy is underappreciated, and scores for endoscopy quality relative to endoscopist specialty are seldom measured. In Korea, certified endoscopy subspecialists and endoscopy training during residency are very likely to play an important role in high-quality endoscopy; however, this issue has not been addressed. The objective of this study was to determine whether endoscopist specialty is associated with high-quality endoscopy based on the Endoscopy Quality Rating Scale (EQRS) in Korea.
This study prospectively collected data from endoscopy units in a hospital setting from September 1st to December 31st 2009; data from the EQRS of the National Cancer Screening Program (NCSP) in Korea were used. The scores of each endoscopy unit based on the EQRS were analyzed in relation to endoscopist specialty. Endoscopist specialty was classified according to endoscopy training during residency and endoscopy subspecialist certification. In Korea, most Internal Medicine and Family Practice trainees must complete several months of endoscopy training before finishing their residency program. Endoscopy subspecialty is certifiable after dedicated endoscopy training for 12 months with a minimum of 1000 cases of supervised esophagogastroduodenoscopy (EGD) and 150 cases of supervised colonoscopy, as well as after passing standard examination.2 If there were two or more endoscopists in a single endoscopy unit with different quality ratings, the endoscopy unit was rated according to the highest rating achieved among the endoscopists, based on the assumption that highly rated endoscopists may have an impact on the quality of each endoscopy unit.
NCSP recommends biennial stomach cancer screening for adults older than 40 years by EGD and/or an upper gastrointestinal series. NCSP also recommends annual fecal occult blood tests for adults over 50 years old and colonoscopies for those with a positive fecal occult blood test. In 2009, a total of 379 endoscopy units in a hospital setting (i.e., hospitals having a minimum of 30 inpatient beds) were classified as target units for quality improvement by NCSP. Among them, 302 endoscopy units participated in a self-reported on-line assessment, and 277 units (73.1%) were targeted for field assessment. Due to a lack of objectivity EQRS data collected from the on-line self assessment were not used in this study. Endoscopy units in a hospital setting that surpassed 200 EGDs monthly or 15 colonoscopies annually, based on data from the Korean Statistical Office, were enrolled for field assessment. To improve recognition of endoscopist for EQRS, orientation manuals for EQRS were sent to each endoscopy unit and many education seminars were conducted, including six nationwide education sessions and Korean Society Gastrointestinal Endoscopy (KSGE) seminars. Furthermore, an online instruction program for EQRS was also developed to supplement the orientation.2
Gastroenterology medical professors (n=154) from university hospitals were commissioned for the project. In order to minimize inter-observer bias, an orientation program focusing on methodology and guidelines was conducted before starting the project. For objective evaluation, two observers visited each endoscopy unit to evaluate all criteria together. Medical records, endoscopic images, and endoscopy-related documents from each endoscopy unit were evaluated for EQRS; direct inspections of endoscopic procedures and/or inspections of simulated patients were also made for some criteria of EQRS that could not be investigated by documents alone.
The EQRS was created in 2009 as a quality improvement and assessment tool for gastrointestinal endoscopy in Korea by a task force team of NCSP. The taskforce team for the development of EQRS comprised members of the Committee for Prevention and Screening of Cancer from the National Cancer Center and the Committee for Endoscopy Quality Improvement and Ethics from the KSGE. Through a review of previous literature on endoscopy quality3-7 along with more than 20 meetings with leading experts to agree upon criteria of the EQRS, criteria which were reflective of endoscopy quality were established in a numerically weighted format. Criteria concerning patient safety, documentation precision, and standardized reprocessing were weighted more heavily than those concerning facilities and equipment, which may depend on the economic status of individual endoscopy units. Finally, 35 items for EGD and 39 items for colonoscopy from the EQRS were selected and used in this project as a measure of endoscopy quality.
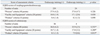
There were a total of 35 items for EGD: 15 for "Process", 9 for "Facilities and Equipment", and 11 for "Product" criteria (Table 1).6 The criteria for the quality of "Process" included items concerning the care of patients before and after EGD, the process of EGD and its documentation, the safety of conscious sedative endoscopy, and the standard reprocessing of the EGD. The criteria for the quality of "Facilities and Equipment" included items concerning instruments, equipment, endoscopy-related documents, and picture quality of the EGD. The criteria for the quality of "Product" included items concerning the integrity of endoscopy reports, H. pylori tests based on indications, and attendance to endoscopy quality related lectures. There were a total of 39 items for colonoscopy: 16 for "Process", 11 for "Facilities and Equipment", and 12 for "Product" criteria (Table 2).7 Criterions were generally similar to those for EGD but with some additional criteria. The criteria for the quality of "Process" included pre-procedural checks for bowel preparation and recording of duration of colonoscopy including withdrawal time. The presence of restrooms and changing rooms for colonoscopy was added to the criteria for the quality of "Facilities and Equipment". The recording of bowel preparation and cecal intubation rate were additionally evaluated for "Product" quality.
All data were presented as numbers (percentage) of patients or as means (standard deviation). The scores of EQRS according to endoscopist specialty were compared using t-tests or the Mann-Whitney U-test. For subgroup analysis, the scores of each criterion of EQRS were also compared between endoscopy subspecialist and non-endoscopy subspecialist groups using t-tests or the Mann-Whitney U-test. In all cases, p≤0.05 was considered statistically significant. All statistical analyses were performed with the SPSS statistical software, version 13.0 (SPSS Inc., Chicago, IL, USA).
The data for 274 endoscopy units out of 277 were analyzed in this study after excluding 3 units with missing data. Among 274 endoscopy units, 182 endoscopy units conducted EGDs only, 11 endoscopy units conducted colonoscopies only, and remaining 81 endoscopy units conducted both EGDs and colonoscopies. As a result, EGD data from 263 endoscopy units were analyzed after excluding 11 endoscopy units that conducted colonoscopies only. Colonoscopy data from 90 endoscopy units were also analyzed after excluding 182 endoscopy units that conducted EGDs only and 2 units with incomplete data collection.
The results of EQRS from the NCSP are shown in Table 3. The vast majority of endoscopy units performed both EGD and colonoscopy with high-scores of EQRS. The mean total score of EQRS was 64.0±6.3 points for EGD units and 62.7±5.6 for colonoscopy units. The scores of EQRS for EGD were 37.2±3.7 for "Process" criteria; 17.9±1.9 for "Facility and Equipment" criteria; and 7.8±1.5 for "Product" criteria. The scores of EQRS for colonoscopy were 36.1±3.0 for "Process" criteria; 18.6±1.3 for "Facility and Equipment" criteria; and 8.0±1.3 for "Product" criteria. The percentage of endoscopy units that did not earn over 50% of the total score of EQRS for EGD were 0.4%, 2.7%, and 0.0% with respect to "Procedure", "Facility and Equipment", and "Product" criteria, respectively. By contrast, none of the endoscopy units earned less than 50% of the total score of EQRS for colonoscopy.
Most EGDs were performed by endoscopists with EGD training during residency in 239 EGD units (90.9%), and colonoscopies were performed by endoscopists with colonoscopy training during residency in 86 colonoscopy units (95.6%) (Table 3). Endoscopy subspecialists performed EGDs in 46% of EGD units (121/263 units) and colonoscopies in 54.4% of colonoscopy units (49/90 units). Endoscopy training during residency did not have a statistically significant effect on improvement in quality of endoscopy (Table 4). However, the scores of EQRS for endoscopy subspecialists were significantly higher than those without endoscopy subspecialty, with respect to nearly all criteria (except for the score of EGD "Process" criteria) (Table 5). In detail, the scores of EQRS for endoscopy subspecialists were significantly higher than those without endoscopy subspecialist certification with respect to following criterions: documentation of endoscopic findings; equipment with higher picture quality; participation in endoscopy quality education; better technical examinations, such as retroflexed or closer observation, recording of the second portion of the duodenum or cecum; recording of colonoscopy procedure time with withdrawal time of more than 6 minutes; and equipment with resuscitation or therapeutic instruments.
High-quality endoscopy may depend on endoscopist specialty, which may be essential for improving the quality of endoscopy. This study may be of particular interest because nationwide endoscopy quality data were collected by visiting endoscopy units, and the analysis of EQRS scores according to endoscopist specialty was made for the first time. To our knowledge, this is the first study to address endoscopist specialty in relation to endoscopy quality.
In this study, a greater number of colonoscopists than gastroscopists underwent endoscopy training during their residency. Furthermore, there were a greater number of endoscopy subspecialists among colonoscopists than gastroscopists. This might be explained by the fact that the degree of specialization for endoscopists to perform colonoscopy is higher than that required for EGD. In this study, training during residency did not have a significant effect on high-quality endoscopy; however, certified endoscopy subspecialists were associated with higher scores of EQRS. This suggests that the minimal extent of endoscopy training during residency does not influence the quality of endoscopy. However, certified endoscopy subspecialty completed by systematic supervised endoscopy training is instrumental in high-quality endoscopy. The supervised endoscopy training that forms a part of the endoscopy subspecialist certification requirements in Korea might contribute a considerable effect on high-quality endoscopy. In our study, endoscopy subspecialists had significantly higher scores for EQRS regarding criteria for the documentation of endoscopic findings, equipment with higher image quality, attendance to endoscopy quality related lectures, better performance during technical examinations, and equipment with resuscitation or therapeutic instruments. It may be possible that endoscopy subspecialists may earn higher scores due to better facilities; however, there were no significant differences in regards to criteria of "Facilities and Equipment" between the two groups.
The issue of endoscopist specialty and quality of endoscopy has been previously addressed in a few Western studies.8-10 In a population-based study of 12487 patients newly diagnosed with colorectal cancer who had a normal colonoscopy within 3 years prior to their diagnosis, the risk of interval colorectal cancers was higher if the colonoscopy was performed by an internist or family physician than if it was performed by a gastroenterologist (p<0.001).8 Rabeneck, et al.9 reported a population-based cohort study of 110402 Ontarians aged 50-80 years old who had negative complete colonoscopies and were followed for up to 15 years. A multivariate analysis for evaluating the risk factors for a new diagnosis of colorectal cancer after a negative colonoscopy revealed that patients whose colonoscopies were performed by non-gastroenterologists had a significantly increased risk of developing subsequent colorectal cancer (p<0.001). These studies may suggest that endoscopist specialty is important for high-quality endoscopy; such findings are consistent with ours. As there may be significant differences in the clinical outcomes and performances among endoscopists,10 gastrointestinal endoscopies should be performed by qualified endoscopists.
There may potentially be some discrepancy in the diagnostic rates with various interpretations of the same findings by different levels of endoscopist specialty.10 The basic and objective criteria that can be proposed for endoscopist specialty is a number of supervised endoscopies.11 As an optimum number of EGD examinations, the American Society for Gastrointestinal Endoscopy (ASGE) recommends at least 130 cases of supervised EGD training;11 the KSGE recommends at least 1000 cases because stomach cancer is more prevalent in Korea than in Western countries.2 For an optimum number of colonoscopies for colonoscopy training, the ASGE and KSGE recommend at least 140 and 150 cases of supervised colonoscopy, respectively.2,11,12 In a prospective multicenter study from Korea, competence in technically efficient screening and diagnostic colonoscopies generally requires experience of more than 150 cases.12 These results provide evidence that structured and supervised endoscopy training may be necessary for endoscopist specialty and high-quality endoscopy performance. However, it is not easy to check for the actual number of supervised endoscopies performed. Therefore, endoscopy subspecialist certification and endoscopy training during residency were presented for the supervised endoscopy training in this study, as supervised endoscopy training could be guaranteed during residency and endoscopy subspecialist training in Korea. For example, endoscopy subspecialist trainees in Korea dedicated endoscopy training for a minimum of 1000 cases of supervised EGD and 150 cases of supervised colonoscopy during their trainings. That's the reason why certified endoscopy subspecialist and endoscopy training during residency were used as indicators for the endoscopist specialty in the current study.
Our study has some limitations. There may be a selection bias because only a portion of endoscopy units were selected and surveyed. For example, endoscopy units that fell short of the designated criteria or that took place in office clinic setting were not included in this study. The extent to which our results apply to all units is still unknown; however, we tried to overcome this bias by surveying endoscopy units nationwide. In addition, the acceptability and utility of the EQRS used in this study were not previously validated. Therefore, validation work is necessary to determine which EQRS are truly reflective of endoscopy quality.
To the best of our knowledge, this study is the first one in English highlighted that endoscopist specialty is an important determinant of high-quality endoscopy. Furthermore, endoscopy subspecialists may lead to higher quality of endoscopy in Korea.
Figures and Tables
Table 2
Endoscopy Quality Rating Scale (EQRS) for Colonoscopy from the National Cancer Screening Program

ACKNOWLEDGEMENTS
This study was supported by a Grant-in-Aid for Cancer Research and Control from the National Cancer Center of Korea (#0960400-1).
We are grateful to all the medical professors, endoscopy units and staff, and endoscopists who participated in this study; without their help, this project would not have been possible. We are also indebted to H.K. Lim and J.E. Kim for their help in collecting data.
References
1. Faigel DO, Pike IM, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Gastrointest Endosc. 2006. 63:4 Suppl. S3–S9.

2. Korean Society Gastrointestinal Endoscopy (KSGE) seminars. Accessed April 13, 2011. Available from: URL: http://www.gie.or.kr.
3. Cohen J, Safdi MA, Deal SE, Baron TH, Chak A, Hoffman B, et al. Quality indicators for esophagogastroduodenoscopy. Gastrointest Endosc. 2006. 63:4 Suppl. S10–S15.

4. Faigel DO, Pike IM, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for gastrointestinal endoscopic procedures: an introduction. Am J Gastroenterol. 2006. 101:866–872.

5. Rex DK, Petrini JL, Baron TH, Chak A, Cohen J, Deal SE, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2006. 63:4 Suppl. S16–S28.

6. Hahm MI, Choi KS, Lee HY, Jun JK, Oh D, Park EC. Who participates in the gastric cancer screening and on-time rescreening in the National Cancer Screening Program? A population-based study in Korea. Cancer Sci. 2011. 102:2241–2247.

7. Lee KS, Oh DK, Han MA, Lee HY, Jun JK, Choi KS, et al. Gastric cancer screening in Korea: report on the national cancer screening program in 2008. Cancer Res Treat. 2011. 43:83–88.

8. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabeneck L. Rates of new or missed colorectal cancers after colonoscopy and their risk factors: a population-based analysis. Gastroenterology. 2007. 132:96–102.

9. Rabeneck L, Paszat LF, Saskin R. Endoscopist specialty is associated with incident colorectal cancer after a negative colonoscopy. Clin Gastroenterol Hepatol. 2010. 8:275–279.

10. Chen SC, Rex DK. Endoscopist can be more powerful than age and male gender in predicting adenoma detection at colonoscopy. Am J Gastroenterol. 2007. 102:856–861.

11. Principles of training in gastrointestinal endoscopy. From the ASGE. American Society for Gastrointestinal Endoscopy. Gastrointest Endosc. 1999. 49:845–853.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download