Abstract
Purpose
This study aimed to evaluate the preventive effects of Camellia sinensis var. assamica (CSVA) on diabetic nephropathy in in vitro and in vivo models.
Materials and Methods
MDCK cells were incubated with 1 mM of oxalate with or without different concentrations of CSVA, then MTT and malondialdehyde (MDA) assays were performed to investigate the preventive effects of CSVA on oxalate-induced cytotoxicity and oxidative stress. Thirty male db/db mice were divided into three groups. Group 1 were fed AIN-93G ad libitum; group 2 were fed AIN-93G mixed with 10% fermented CSVA ad libitum; group 3 were fed AIN-93G mixed with 10% non-fermented CSVA ad libitum. The mice were sacrificed 14 weeks later, and the serum glucose level, 24-hour urine chemistry, and morphological changes in the kidneys were examined.
Results
As CSVA concentrations increased, viable MDCK cells increased in concentration. MDA production decreased over time in the CSVA treated group. The creatinine clearance of group 3 was lower than those of groups 1 and 2. The amount of urine microalbumin and protein in group 1 were higher than those in groups 2 and 3. Also, more glomerulus basement membrane foot processes were preserved in groups 2 and 3.
Diabetic nephropathy is a microvascular complication of diabetes mellitus associated with significant morbidity and mortality.1 Because alterations to glomerular structures are irreversible, the primary goal of management for patients with diabetic nephropathy is to prevent disease progression to end stage renal disease. Therefore, strict control of blood pressure as well as maintaining normal glucose and lipid levels are important for preserving renal function.2 However, it is well known that attempts to control these factors are not sufficient for the prevention of progression of diabetic nephropathy. Thus, many investigators have started to study the effects of traditional medicines, folk remedies, and herbal medicines to identify novel agents that might be effective managing diabetic complications, especially diabetic nephropathy.3-7
Recently, interest in green tea as a promising agent for the prevention or reduction of risk for many human diseases has increased worldwide. With regard to preventing diabetic complications, the antioxidant activity of green tea might play an important role. In this study, we aimed to evaluate the preventive effects of Camellia sinensis var. assamica (CSVA), traditionally consumed as a health-promoting beverage in Korea, on diabetic nephropathy in both in vitro and in vivo models. In addition, we classified CSVA as a fermented or non-fermented leaf in the in vivo protocol and evaluated whether the preventive effects on diabetic nephropathy differed according to the degree of fermentation.
Non-fermented CSVA were obtained from CSVA in Gimhae, Korea. Twenty grams of CSVA leaves were extracted with 400 mL of 100% methanol in a round-bottom flask equipped with a condenser. The temperature of extraction was kept at boiling temperature and the extraction mixture was constantly stirred with a magnetic bar. After two hours of extraction, the extraction mixture was cooled, the vacuum filtered (0.45 µm), and the methanol evaporated under the vacuum at 40℃.
MDCK cells (American Type Culture Collection, Washington D.C, USA) were cultured in a Dulbecco's modified Eagle medium (Invitrogen, Carlsbad, CA, USA) supplemented with 10% fetal bovine serum (Sigma-Aldrich, St. Louis, MO, USA) at 37℃, in air containing 5% CO2.
MDCK cells were subcultured in 96-well plates and grown to 70-80% confluence. The cells were then exposed to 1 mM of sodium oxalate (Alfa Aesar, Ward Hill, MA, USA) to induce renal cell damage and various concentrations of CSVA extract (0, 10, and 25 µg/L) for 24 hours. Subsequently MTT (0.1 mg, 50 µL of 2 mg/mL) in phosphate-buffered saline was added, followed by incubation for four hours at 37℃. Optical densities were measured on a microplate reader (Becton Dickinson Labware, Franklin Lakes, NJ, USA) at 540 nm.
MDCK cells were exposed to 1 mM of sodium oxalate for various periods of time (30, 60, and 120 minutes) with or without 50 µg/L of CSVA extract. The lipid peroxidation levels were then evaluated by measuring the MDA as described by Wong, et al.8
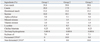
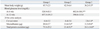
All surgical and experimental procedures were approved by the Seoul National University Institutional Animal Care and Use Committee (SNUIACUC, No. 08-0213) and conducted between November 2008 and February 2009. Thirty male C57BL/Ks db/db mice were divided into three groups by random sampling methods after adaptation to their new environment for one week. Group 1 (n=10) were fed AIN-93G ad libitum. Group 2 (n=10) were fed AIN-93G mixed with 10% fermented CSVA ad libitum. Group 3 (n=10) were fed AIN-93G mixed with 10% non-fermented CSVA ad libitum. Table 1 shows the composition of the basal and experimental diets in each group.
We monitored the total amounts of food and water intake and the body weight of the mice every week. At 6 and 12 weeks of oral intake, blood was collected from the tail-vein and fasting blood glucose levels were measured using Accu-Chek Performa blood glucose monitoring system (glucometer) (Roche Diagnostics, Pleasanton, CA, USA). After 14 weeks of the designated oral intake, 24-hour urine was collected from each mouse in their metabolic cages. We evaluated several factors to assess the effects of CSVA on diabetic nephropathy. These factors included the results of the 24-hour urine analysis, which measured creatinine clearance (Ccr), amount of microalbumin, and total protein. In addition, we examined the histology of the kidneys of all experimental mice to determine the effects of CSVA on the morphology of diabetic nephropathy. For these examinations, all mice were sacrificed using the cardiac puncture technique after fasting for 12 hours. The kidneys were carefully removed after the abdominal cavity was opened. The fatty tissue was gently removed from the renal parenchyma and the kidneys were weighed. For the histological examination under an electron microscope, we excised 1×1 mm of cortical tissue from each kidney and immediately fixed the samples in 2.5% glutaraldehyde in 0.1 M sodium cacodylate buffer at 4℃ for 4 hours and wash them twice (each time for 1 hour) with 0.1 M buffer. Then, we performed secondary fixation in 2% osmium tetroxide in 0.2 M buffer for 1 hour and rinsed twice (each time for 5 min) in 0.2 M buffer and multistep dehydration in 70%, 90% and 100% ethanol. After propylene oxide infiltration, epoxy resin was treated for overnight and embedded with freshly prepared resin. Finally, the specimens were polymerized at 60℃ for 48 hours. Following the E-firm block formation, ultrathin sections (60 nm) were obtained and subjected to electron staining, meaning double staining with uranyl acetate for 30 min and lead citrate for 10 min; the specimens were then viewed on transmission electron microscopy (JEM-1200EX, JEOL, Tokyo, Japan) operating at 120 kV, which was documented by the digital imaging. The remnant renal tissues were then placed in formalin for paraffin block formation. The paraffin blocks were sectioned and then stained with hematoxylin and eosin (H&E). The tissues were then carefully examined by Olympus SZX7 stereomicroscope (Olympus, Tokyo, Japan) with a plain objective.
The Statistical Package for the Social Sciences (SPSS), version 11.0 (SPSS Inc., Chicago, IL, USA) was used for the statistical analysis. All experimental results were analyzed using ANOVA and Dunnett's test and are reported as mean values±standard deviation. p<0.05 was accepted as statistically significant.
The number of viable MDCK cells significantly decreased by 40% after exposure to 1 mM of sodium oxalate as compared to the control group (Fig. 1). In contrast, the number of MDCK cells increased as the concentration of CSVA increased, as noted by the fraction of viable MDCK cells: 62.9%, 66.0%, and 75.1% in order (Fig. 1) (p<0.05).
The MDA production increased with time in the sodium oxalate-treated group. In contrast, in the group with co-exposure to CSVA extracts, MDA levels decreased with time until 60 minutes, then increased slightly after 120 minutes (Fig. 2) (p<0.05).
The mean body weights of the three experimental groups were 45.7±2.3 g, 42.5±6.4 g, and 36.2±5.5 g, respectively. The mean body weight of group 3 was significantly lower than the other two groups (p<0.05) (Table 2).
After 6 weeks of oral intake, the mean serum glucose level of the control group was higher than that of the CSVA-treated group (528.9±83.5 mg/dL versus 402.0±100.3 mg/dL, p<0.05) (Table 2). However, after 12 weeks of oral intake, there was no statistical difference in the mean serum glucose level between the control and CSVA-treated groups (457.5±191.5 mg/dL versus 390.8±115.0 mg/dL, p>0.05) (Table 2).
The Ccr of group 3 was 2.8±1.6 µL/min; this result indicated a significant decrease in the Ccr in group 3 compared to those in groups 1 and 2 (p<0.05) (Table 2). The amounts of microalbumin and protein in the 24-hour urine of group 1 were significantly higher than those of groups 2 and 3 (20.8±5.7 µg versus 11.6±5.6 µg and 11.5±9.6 µg in the 24-hour microalbumin excretion; 73.3±25.2 µg versus 21.4±9.2 µg and 24.1±14.0 µg in total protein excretion, p<0.05) (Table 2).
Fig. 3 shows the mean weight of the kidneys. Groups 2 and 3 had significantly decreased kidney weights (the sum of right and left; 0.45±0.04 g, 0.36±0.03 g, and 0.34±0.03 g in groups 1, 2 and 3, respectively, p<0.05). Optic microscopy showed no significant differences in the architecture of the glomerulus basement membrane (GBM). However, the electron microscope showed that more GBM foot processes were preserved in groups 2 and 3, and especially group 3 had a greater number of foot processes than group 2, while group 1 had loss of all of GBM foot processes (Fig. 4).
Hyperglycemia is strongly associated with diabetic complications. Effective control of hyperglycemia is an important goal of treatment and prevention.9 However, there are few effective agents that prevent the development of diabetic nephropathy, although strict control of hyperglycemia is possible with the use of several diabetic treatments.10,11 Recently, green tea has been the focus of great interest due to its beneficial properties for the prevention and treatment of human disease. Several epidemiology and experimental studies have provided evidence that green tea has antioxidant activity, anticarcinogenic potential, and preventive effects towards cardiovascular disease.4-7 However, there is still controversy regarding the beneficial effects of green tea on diabetic nephropathy.
Renno, et al.3 recently showed that green tea had long-term beneficial effects on diabetic nephropathy in an animal model. They reported that green tea catechins improved levels of serum glucose and glycosylated protein as well as the urine parameters. Ryu, et al.12 did not find that green tea had beneficial effects on serum glucose levels or insulin resistance in their study. However, these conflicting findings might be due to differences in doses, amounts of green tea, time of exposure and type of green tea as well as the degree of hyperglycemia and the methods of experimentation.
There are two basic varieties of green tea; CSVA, a large-leaf, tall and quick-growing tree well-suited to very warm climates, and Camellia sinensis var. sinensis, a small-leaf, slower-growing bush that can withstand colder climates. Green tea produced from CSVA has been known to have higher polyphenol content (30%) than green tea from Camellia sinensis var. sinensis (20%).13 However, most of studies have focused on Camellia sinensis var. sinensis. To our knowledge, ours is the first study to show the preventive effect of CSVA on diabetic nephropathy.
We showed that CSVA prevented oxalate-induced cytotoxicity and oxidative stress in in vitro experiments. Viable MDCK cells proliferated after the administration of CSVA extracts, up to about 15%, under conditions of oxalate exposure. In addition, the MDA levels in the CSVA extract-treated group decreased with time until 60 minutes. Consistent with these results, Jeong, et al.14 reported that green tea administration reduced oxalate induced free-radical stress in NRK-52E cells. Several studies have reported the anti-oxidative effects of green tea even in Parkinson's disease and atherosclerosis, which have been associated with free-radical damage.4-6
We demonstrated that administration of CSVA for 6 weeks lowered serum glucose levels, indicating the beneficial effect of CSVA on glucose tolerance in the early period of intake. However, after 12 weeks of feeding, serum glucose levels did not statistically differ between the control and the CSVA treated groups. This finding might be explained by some experiments that showed that insulin resistance improved gradually and developed to control serum glucose levels effectively with age in diabetic mice.7,15
The results of our study showed that there was less urinary protein excretion in the experimental group than in the control group. These findings suggest that administration of CSVA reduced the amount of proteinuria, which is consistent with the findings of several previous investigations into the beneficial effects of green tea on proteinuria.16,17
Unexpectedly, the 24-hour Ccr and the total kidney weight were significantly higher in the control group than in the CSVA, especially non-fermented, treated groups. However, more GBM foot processes were preserved in the CSVA treated group. This paradoxical finding might be attributed to a hyperfiltration phenomenon caused by loss of the GBM. Glomerular filtration rate, kidney size, and plasma renal flow were found to be supra-normal in young diabetes patients as compared to the non-diabetes controls.18 It was hypothesized that alterations to glomerular microcirculation would lead to single nephron injury; remnant nephrons would compensate with increases in pressures and flows; and that a self-perpetuating cycle of renal injury would be established.19
In addition, we found that non-fermented CSVA was more effective with regards to controlling body weight, Ccr, and histological changes in diabetic nephropathy than fermented CSVA. This suggests that fermentation of CSVA might attenuate the beneficial effects on body weight control, Ccr and histological changes. With regard to molecular mechanisms, several investigations have demonstrated that the health effects of green tea are attributed to its polyphenol components such as catechins.14,20 The four major catechins are (-)-epigallocatechin-3-gallate (EGCG), which is the most abundant of all catechins, (-)-epigallocatechin, (-)-epicatechin-3-gallate, and (-)-epicatechin. EGCG has received a great deal of interest because it is thought to be the most potent catechin in terms of reducing oxidative stress and scavenging reactive oxygen radicals, thereby potentially preventing the development of long-term complications of diabetes.15,21,22 However, Tu, et al.23 demonstrated that the total catechin concentration in green tea decreased by 37% in the first 24 hours of fermentation and had decreased by 57.3% by the end of the fermentation. Based on this finding, we can speculate that better experimental results from the non-fermented CSVA group might come from changing the ingredients of green tea during fermentation.
Finally, several parameters used in this study, such as MTT assay, weight of kidneys, albuminuria, and the EM images of foot process effacement may not be enough to show the obvious preventive effect of CSVA on diabetic nephropathy and to elicit the significant correlation between in vitro and in vivo study. Thus, we may not conclude that the CSVA has definite preventive effects on diabetic nephropathy; rather, we may say that CSVA has beneficial tendencies regarding prevention of diabetic nephropathy. We consider this study to be a pilot study for the preventive effect of CSVA on diabetic nephropathy. More definitive evidence is needed in in vitro and in vivo models in further studies using several parameters, such as urinary 8-OH-deoxyhuanosine, 8-iso-PGEF2a, HbA1c levels, and EM examination of GBM thickening and mesangial volume increase.
In conclusion, the results of the present study demonstrate that CSVA is associated with preventive effects in oxalate- induced cytotoxicity and production of lipid peroxidation in an in vitro setting. Furthermore, CSVA has beneficial preventive tendencies with regard to early stage diabetic nephropathy, acting by preventing glomerular hyperfiltration, hypertrophic changes, and subsequent protein loss in the urine.
Figures and Tables
Fig. 1
MDCK cell viability on the concentration of CSVA following exposure to sodium oxalate (*p<0.05). MDCK, Madin-Darby canine kidney; CSVA, Camellia sinensis var. assamica.
Fig. 2
MDA levels following exposure to sodium oxalate and CSVA according to time (*p<0.05 and **p<0.01 ). MDA, malondialdehyde; CSVA, Camellia sinensis var. assamica.

Fig. 4
Electron microscopy (EM) of GBM (glomerulus basement membrane): (A) Group 1 is the control group. (B) Group 2 is the fermented Camellia sinensis var. assamica (CSVA)-treated group. (C) Group 3 is the non-fermented CSVA-treated group. The black arrows show the GBM foot process.

ACKNOWLEDGEMENTS
We acknowledge the financial support for this study from Technology Development Program for Agriculture and Forestry, Ministry for Agriculture, Forestry and Fisheries, Republic of Korea.
References
1. Soldatos G, Cooper ME. Diabetic nephropathy: important pathophysiologic mechanisms. Diabetes Res Clin Pract. 2008. 82:Suppl 1. S75–S79.

2. Giunti S, Barit D, Cooper ME. Diabetic nephropathy: from mechanisms to rational therapies. Minerva Med. 2006. 97:241–262.
3. Renno WM, Abdeen S, Alkhalaf M, Asfar S. Effect of green tea on kidney tubules of diabetic rats. Br J Nutr. 2008. 100:652–659.

4. Cabrera C, Artacho R, Giménez R. Beneficial effects of green tea--a review. J Am Coll Nutr. 2006. 25:79–99.

5. Crespy V, Williamson G. A review of the health effects of green tea catechins in in vivo animal models. J Nutr. 2004. 134:3431S–3440S.

6. Son GM, Bae SM, Chung JY, Shin DJ, Sung TS. Antioxidative Effect on the Green Tea and Pu-erh Tea Extracts. Korean J Food and Nutr. 2005. 18:219–224.
7. Thielecke F, Boschmann M. The potential role of green tea catechins in the prevention of the metabolic syndrome - a review. Phytochemistry. 2009. 70:11–24.

8. Wong SH, Knight JA, Hopfer SM, Zaharia O, Leach CN Jr, Sunderman FW Jr. Lipoperoxides in plasma as measured by liquid-chromatographic separation of malondialdehyde-thiobarbituric acid adduct. Clin Chem. 1987. 33:214–220.

9. Unger J. Diagnosis and management of type 2 diabetes and prediabetes. Prim Care. 2007. 34:731–759.

10. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993. 329:977–986.
11. Chang HY, Wallis M, Tiralongo E. Use of complementary and alternative medicine among people living with diabetes: literature review. J Adv Nurs. 2007. 58:307–319.

12. Ryu OH, Lee J, Lee KW, Kim HY, Seo JA, Kim SG, et al. Effects of green tea consumption on inflammation, insulin resistance and pulse wave velocity in type 2 diabetes patients. Diabetes Res Clin Pract. 2006. 71:356–358.

13. Chan EWC, Lim YY, Chew YL. Antioxidant activity of Camellia sinensis leaves and tea from a lowland plantation in Malaysia. Food Chem. 2007. 102:1214–1222.

14. Jeong BC, Kim BS, Kim JI, Kim HH. Effects of green tea on urinary stone formation: an in vivo and in vitro study. J Endourol. 2006. 20:356–361.

15. Igarashi K, Honma K, Yoshinari O, Nanjo F, Hara Y. Effects of dietary catechins on glucose tolerance, blood pressure and oxidative status in Goto-Kakizaki rats. J Nutr Sci Vitaminol (Tokyo). 2007. 53:496–500.

16. Yamabe N, Yokozawa T, Oya T, Kim M. Therapeutic potential of (-)-epigallocatechin 3-O-gallate on renal damage in diabetic nephropathy model rats. J Pharmacol Exp Ther. 2006. 319:228–236.

17. Yokozawa T, Nakagawa T, Oya T, Okubo T, Juneja LR. Green tea polyphenols and dietary fibre protect against kidney damage in rats with diabetic nephropathy. J Pharm Pharmacol. 2005. 57:773–780.

18. Christiansen JS, Gammelgaard J, Frandsen M, Parving HH. Increased kidney size, glomerular filtration rate and renal plasma flow in short-term insulin-dependent diabetics. Diabetologia. 1981. 20:451–456.

19. Zatz R, Brenner BM. Pathogenesis of diabetic microangiopathy. The hemodynamic view. Am J Med. 1986. 80:443–453.

20. Li JJ, Kwak SJ, Jung DS, Kim JJ, Yoo TH, Ryu DR, et al. Podocyte biology in diabetic nephropathy. Kidney Int Suppl. 2007. S36–S42.

21. Guo Q, Zhao B, Li M, Shen S, Xin W. Studies on protective mechanisms of four components of green tea polyphenols against lipid peroxidation in synaptosomes. Biochim Biophys Acta. 1996. 1304:210–222.

22. Zaveri NT. Green tea and its polyphenolic catechins: medicinal uses in cancer and noncancer applications. Life Sci. 2006. 78:2073–2080.

23. Tu YY, Xia HL, Watanabe N. The changes of catechins during the fermentation of green tea. Prikl Biokhim Mikrobiol. 2005. 41:652–655.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download