Abstract
Purpose
Laminectomy is generally the treatment of choice for removal of spinal tumors. However, it has been shown that laminectomy may cause instability due to damage of posterior elements of the spinal column, which may induce subsequent kyphosis in the future. Therefore, to reduce the risk of deformity and spinal instability after laminectomy, hemilaminectomy has been used. However, the medium to long-term effects of hemilaminectomy on spinal sagittal alignment is not well understood. The present study was performed to evaluate the clinical outcomes, including spinal sagittal alignment of patients, associated with spinal cord tumors treated by surgical excision using hemilaminectomy.
Materials and Methods
Twenty hemilaminectomy operations at our institute for extramedullary or extradural spinal cord tumors in 19 patients were evaluated retrospectively with an average follow-up of 85 months (range, 40-131 months). Neurological condition was evaluated using the improvement ratio of the Japanese Orthopaedic Association Score (JOA score) for cervical, thoracic myelopathy, or back pain, and sagittal alignment by sagittal Cobb angle of the hemilaminectomied area.
Results
The mean improvement ratio of neurological results was 56.7% in the cervical spine (p < 0.01, n = 10), 26.3% in the thoracic spine (not significant, n = 5), and 48.6% in the lumbar spine (NS, n = 5). The sagittal Cobb angle was 4.3 ± 18.0° in the preoperative period and 5.4 ± 17.6° at the latest follow-up, indicating no significant deterioration.
A spinal tumor is defined as a growth of cells (mass) within or surrounding the spinal cord. In cases in which compression of the spinal cord is severe and the risk of neurological deterioration increases, surgery is needed to relieve the compression. Bilateral laminectomy is generally the treatment of choice for removal of spinal tumors.1-3 However, it has been shown that laminectomy may cause instability due to damage of posterior elements of the spinal column, which may induce subsequent kyphosis in the future.3-7 Therefore, to reduce the risk of deformity and spinal instability after laminectomy, hemilaminectomy has been used.1,8-11 However, the medium to long-term effects of hemilaminectomy on spinal sagittal alignment are not well understood. Therefore, the present study was performed to evaluate the clinical outcomes, including spinal sagittal alignment of patients, associated with spinal cord tumors treated by surgical excision using hemilaminectomy.
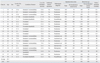
Nineteen patients (9 female and 10 male) with spinal cord tumors treated surgically by hemilaminectomy (20 operations) at our institute between 1997 and 2004 were followed-up and reviewed in a prospective study (Table 1). The mean ± SD age at the time of surgery was 42.3 ± 16.4 years (range, 14-74 years), and the mean ± SD follow-up period was 85 ± 30 months (range, 40-131 months). One patient underwent hemilaminectomy twice for removal of tumors at the cauda equina and cervical region. All patients reported local or radiating pain or sensory or motor disturbance of the extremities and were diagnosed as having spinal cord tumors by enhanced and plain magnetic resonance imaging (MRI). Hemilaminectomy was selected for resection of tumors with clear borders and extramedullary or extradural dorsal and unilateral lesions. Tumors located anteriorly to the spinal cord and tumors appearing malignant radiologically were removed by total laminectomy, which provided a better view and safer removal of the tumors.
The tumors were observed in the following regions: cervical in 9 cases (45.0%), cervicothoracic in 1 (5.0%), thoracic in 5 (25.0%), and lumbar in 5 (25.0%). The locations of the tumors were extradural in 60.0% (n = 12) and intradural/extramedullary in 40.0% (n = 8) (Table 1).
Surgery was performed when imaging modalities showed that the tumors had grown, or when patients had a sensory or motor disorder. There were no obvious differences in timing of surgery compared with other reports.
All operations were performed by two surgeons belonging to our institution. A midline incision was made with the patient in the prone position. Resection of bone and ligaments was restricted to the side of the tumor. The vertebral arch was drilled under a microscope using a high-speed drill. The flavum was removed until the contralateral root or dural curve was exposed. The spinous process and its base, the contralateral lamina including the flavum and muscle were preserved (Fig. 1).12
The numbers of hemilaminectomied laminae were 2 in 12 cases, 3 in 4 cases, 4 in 2 cases, 6 in 1 case, and 7 in 1 case, with an average of 2.9 ± 1.4 (Table 1).
Pathological diagnoses using specimens from resected tumors were identified (Table 1).
To evaluate the invasiveness of the operations, the amount of blood loss during surgery and the duration of surgery were noted. These values were standardized by the number of hemilaminectomied laminae (Table 1).
Radicality of resection was assessed by the surgeons as complete resection or incomplete resection. Cases of incomplete resection were classified into unexpectedly incomplete and predictably incomplete resection.9
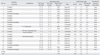
Neurological status was evaluated using the Japanese Orthopaedic Association Scores (JOA score) for cervical myelopathy (JOA-C),13,14 thoracic myelopathy (JOA-T),15-17 and back pain (JOA-B).18,19 The JOA-C, JOA-T, and JOA-B were recorded within one month before surgery and at the final follow-up. The increases in these scores, i.e., the difference between the final and preoperative scores, were also evaluated. A full score of JOA-C was defined as 17 points: 8 for upper and lower motor functions, 6 for sensory functions, and 3 for bladder-rectal function (Table 2). JOA-T, consisting of 11 points, was obtained after subtracting the parameters on the upper extremities from the JOA-C (Table 2). A full score of JOA-B was defined as 29 points: 9 for 3 subjective symptoms, 6 for 3 clinical signs, and 14 for 7 activities of daily living (Table 3). The improvement ratio of these scores,17 which indicates the degree of normalization after surgery, was calculated as follows:
Improvement ratio of JOA-C: (postoperative score - preoperative score) × 100 / [17 (full score) - preoperative score] (%)
Improvement ratio of JOA-T: (postoperative score - preoperative score) × 100 / [11 (full score) - preoperative score] (%)
Improvement ratio of JOA-B: (postoperative score-preoperative score) × 100 / [29 (full score) -preoperative score] (%)
Changes in the neurological status were classified into three grades: improved, unchanged, and worsened.
Cobb sagittal angle between the vertebral bodies at the upper and lower ends of the area of hemilaminectomy was measured on plain X-ray films preoperatively and at the final follow-up.
Pathological examination revealed neurinoma in 12 cases (54.5%), arachnoid cyst in 3 (13.6%), neurofibroma in 2 (10.0%, n = 2), meningioma in 1 (5.0%), chondroma in 1 (5%), and ependymoma in 1 (5%) (Table 1).
The duration of surgery was 225 ± 105 min (average ± SD). When divided by the number of hemilaminectomied levels, the duration was 89 ± 48 min. The amount of blood loss during surgery was 416 ± 392 g. When divided by the number of hemilaminectomied levels, the amount of blood loss was 172 ± 190 g (Table 1).
Radicality of resection was "complete" in 16 patients (80.0%) and "predictably incomplete" in 4 patients (20.0%). There were no "unexpected incomplete" resections. The four patients with predictably incomplete resections were those with dumbbell-shaped tumors; three of these patients underwent additional resections using the anterior approach. These patients, however, did not require any form of instrumented fusion (Table 4). Patient No.13 had a huge arachnoid cyst from T3 to T8, compressing the spinal cord. Total removal of this cyst required multilevel hemilaminectomy from T2 to T8. Conversion to conventional laminectomy was not required in any of the cases in the present study.
Three complications were recorded. In Case 10 (chondroma, C1-3 levels), slight subluxation at C1-2 occurred after the operation. However, the subluxation was asymptomatic. Case 12 suffered from intracranial hypotension syndrome due to cerebrospinal fluid leakage, which was successfully managed conservatively. Case 14 developed vesicorectal disorder after the resection of thoracic neurinoma. At the final follow-up, the symptoms had recovered almost completely (Table 4).
Postoperative neurological status improved in 16 cases (80%), unchanged in 3 (15%), and worsened in 1 (5%). Case 14 suffering from vesicorectal dysfunction showed worsening of the neurological status. The mean improvement ratio in neurological status scores was 49.8% (Table 4). When the scores of the three spinal regions were analyzed separately, we found that the improvement ratios were 56.7% in the cervical spine (p < 0.01), 26.3% in the thoracic spine not significant (NS), and 48.6% in the lumbar spine (NS) (Fig. 2). There were no significant differences in improvement ratios among the three groups (one-way analysis of variance).
The Cobb sagittal angle was 4.3 ± 18.0° lordosis (range, - 36.6° to 35.7°) preoperatively and 5.4 ± 17.6° lordosis (range, - 38.6° to 38.2°) at the final follow-up. The change in the lordotic angle ranged from 2.0° decrease to 9.3° increase, showing no significant changes (Table 2).
There were no cases of tumor recurrence in the postoperative period in this series, and none received adjuvant therapy (Table 2).
In the present study, clinical outcomes of the removal of spinal tumors by hemilaminectomy in 20 cases were reviewed with an average follow-up of 85 months. While several authors have reported the usefulness of this surgical method,1,8-11 medium to long-term follow-up results have rarely been reported. The present results with a medium to long-term follow-up showed a relatively low level of operative invasiveness, good improvement ratio of neurological status, no significant deterioration in spinal sagittal alignment, and no recurrence of tumors. Importantly, as hemilaminectomy was originally adopted for spinal tumor removal due to its possible advantage in preserving the sagittal alignment,20 the present results actually confirmed the advantage of this approach.
To reduce the risk of deformity and spinal instability after laminectomy, Raimondi, et al.2 and Parkinson21 recommended osteoplastic laminectomy, originally described by Bickham,22 to reconstruct the structures of the posterior column. However, this technique is somewhat difficult, and is therefore time consuming,2,21 To avoid subsequent complications in spinal sagittal alignment, the hemilaminectomy approach that can preserve interspinous ligaments, intervertebral joints, and paravertebral muscles of the contralateral side was then indicated for resection of spinal cord tumors.19 Although the usefulness of tumor removal by hemilaminectomy in maintenance of sagittal alignment in cervical regions has been reported previously by Asazuma, et al.20 the present medium to long-term results from cases with hemilaminectomy of a number of different levels and spinal regions with no deterioration in the spinal sagittal alignment represent a significant addition to the literature.
While hemilaminectomy is advantageous in preserving posterior spinal structures, the hemilaminectomy approach provides a relatively narrow view of the spinal intracanalar regions.12 Ozawa, et al.23 noted several limitations and disadvantages of hemilaminectomy in removal of spinal tumors. They suggested that additional foraminotomies and reconstructions using interspinous wiring are necessary for radical resection of dumbbell tumors of Eden type 2 and 3.23 They also suggested that huge tumors with scalloping of vertebrae, midline tumors that require resection and reconstruction of the dural sac, easy bleeding tumors spreading to both sides, malignant lymphomas, and hemangiomas are difficult to manage by hemilaminectomy.23 We agree with this concept and have altered our treatment strategy in accordance with it. Hemilaminectomy would be optimal for tumors with clear borders, extramedullary and extradural tumors, and dorsal and unilateral lesions throughout the spine. In contrast, we chose conventional laminectomy for removal of tumors with unclear borders, and for intramedullary, ventral, and bilateral spreading lesions. We observed a high radicality ratio (80.0%), no incidence of intraoperative conversion from hemilaminectomy to conventional laminectomy, and no postoperative tumor recurrence. Consistent with previous findings,23 the radicality of resection was predictably incomplete in 4 of the 5 patients with dumbbell-shaped tumors. We found cerebrospinal fluid (CSF) leakage resulting from one of the 20 operations (5%), higher than reported in patients who underwent either hemilaminectomy (0.7%) or total laminectomy (3%).14 The CSF leakage we observed in one of our patients was deemed minor and was managed conservatively. Definitions of CSF leakage should be standardized, in order to assess differences in rates of CSF leakage. During preoperative screening, we excluded patients suspected of having malignant tumors or tumors located anteriorly to the spinal cord. Those tumors were surgically removed via total laminectomy. Consequently, we did not convert these patients from hemilaminectomy to total laminectomy during surgery. Pathological analysis showed that all of these tumors were benign. These findings suggest that spinal tumor removal by hemilaminectomy through strict preoperative assessment using imaging modalities9 can guarantee a successful clinical outcome.
There were several limitations in the design of this study. First, in this study, a single cohort that underwent a single surgical strategy was followed-up prospectively. Therefore, a comparative study with similar patients treated using other strategies in a randomized manner must be performed. Second, the mean overall final follow-up period was 85 months, ranging from 40 to 131 months. Evaluations at consistent time periods are required in future studies to obtain more clinically relevant data. Third, the patients in this study were relatively young (median age, 42.3 years), indicating that they are not representative of a generalized patient population. Inclusion of elderly and/or osteopenic patients may have altered our results. Fourth, our patient population was skewed, in having more cervical patients then other regions. A laminectomy lower down in the spine would probably have had more destabilizing effects, thus altering the results of postoperative spinal alignment. Finally, our results may have been more convincing had the patient cohort been more limited relative to the types of tumor.
In conclusion, twenty cases of spinal tumor excision by hemilaminectomy were reviewed. This surgical method provided satisfactory outcomes with a good neurological status, maintenance of sagittal alignment, and little complication over medium to long-term follow-up.
Figures and Tables
Fig. 1
(A) Preoperative MRI of Case 9 showing extradural neurinoma of the upper cervical spine. (B) Postoperative MRI showing tumor resection by hemilaminectomy. Upper panel, Axial image; Lower panel, Sagittal image.

References
1. Eggert HR, Scheremet R, Seeger W, Gaitzsch J. Unilateral microsurgical approaches to extramedullary spinal tumours. Operative technique and results. Acta Neurochir (Wien). 1983. 67:245–253.
2. Raimondi AJ, Gutierrez FA, Di Rocco C. Laminotomy and total reconstruction of the posterior spinal arch for spinal canal surgery in childhood. J Neurosurg. 1976. 45:555–560.

3. Yasuoka S, Peterson HA, Laws ER Jr, MacCarty CS. Pathogenesis and prophylaxis of postlaminectomy deformity of the spine after multiple level laminectomy: difference between children and adults. Neurosurgery. 1981. 9:145–152.

4. Bradford DS. Spinal instability: orthopedic perspective and prevention. Clin Neurosurg. 1980. 27:591–610.

5. Cattell HS, Clark GL Jr. Cervical kyphosis and instability following multiple laminectomies in children. J Bone Joint Surg Am. 1967. 49:713–720.

7. Reimer R, Onofrio BM. Astrocytomas of the spinal cord in children and adolescents. J Neurosurg. 1985. 63:669–675.

8. Bertalanffy H, Mitani S, Otani M, Ichikizaki K, Taya S. Usefulness of hemilaminectomy for microsurgical management of intraspinal lesions. Keio J Med. 1992. 41:76–79.

9. Chiou SM, Eggert HR, Laborde G, Seeger W. Microsurgical unilateral approaches for spinal tumour surgery: eight years' experience in 256 primary operated patients. Acta Neurochir (Wien). 1989. 100:127–133.

10. Oleshkevich FV, Rozhanets NI, Volkovets NN. [Hemilaminectomy in the removal of spinal cord tumors]. Zh Vopr Neirokhir Im N N Burdenko. 1988. 30–32.
11. Sario-glu AC, Hanci M, Bozkuş H, Kaynar MY, Kafadar A. Unilateral hemilaminectomy for the removal of the spinal space-occupying lesions. Minim Invasive Neurosurg. 1997. 40:74–77.

12. Oktem IS, Akdemir H, Kurtsoy A, Koç RK, Menkü A, Tucer B. Hemilaminectomy for the removal of the spinal lesions. Spinal Cord. 2000. 38:92–96.

13. Hosono N, Yonenobu K, Ono K. [Japanese Orthopedic Association: Scoring system for cervical myelopathy]. J Jpn Orthop Assoc. 1994. 68:490–503.
14. Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the japanese orthopaedic association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976). 2001. 26:1890–1894.

15. Yonenobu K, Ebara S, Fujiwara K, Yamashita K, Ono K, Yamamoto T, et al. Thoracic myelopathy secondary to ossification of the spinal ligament. J Neurosurg. 1987. 66:511–518.

16. Fujimura Y, Nishi Y, Nakamura M, Toyama Y, Suzuki N. Long-term follow-up study of anterior decompression and fusion for thoracic myelopathy resulting from ossification of the posterior longitudinal ligament. Spine (Phila Pa 1976). 1997. 22:305–311.

17. Ohnishi K, Miyamoto K, Kanamori Y, Kodama H, Hosoe H, Shimizu K. Anterior decompression and fusion for multiple thoracic disc herniation. J Bone Joint Surg Br. 2005. 87:356–360.

18. Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine (Phila Pa 1976). 2000. 25:1837–1842.

19. Yorimitsu E, Chiba K, Toyama Y, Hirabayashi K. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine (Phila Pa 1976). 2001. 26:652–657.
20. Asazuma T, Nakamura M, Matsumoto M, Chibo K, Toyama Y. Postoperative changes of spinal curvature and range of motion in adult patients with cervical spinal cord tumors: analysis of 51 cases and review of the literature. J Spinal Disord Tech. 2004. 17:178–182.

21. Parkinson D. Replacement laminotomy. Surg Neurol. 1977. 8:277–279.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download