Abstract
Purpose
The optimal treatment regimen for Mycobacterium avium complex (MAC) lung disease has not yet been fully established. We evaluated the efficacy of standardized combination antibiotic therapy and the factors that might affect unfavorable microbiologic responses in patients with MAC pulmonary disease.
Materials and Methods
This retrospective study reviewed data from 96 patients (56 females; median age 59 years) treated with newly diagnosed MAC lung disease between January 2003 and December 2006.
Results
All patients received standardized combination antibiotic therapy, consisting of clarithromycin, rifampicin, and ethambutol. Streptomycin was additionally given in 72 patients (75%) for a median duration of 4.5 months. The overall favorable microbiologic response rate was 79% (76/96); 20 patients (21%) had unfavorable microbiologic responses, including failure to sputum conversion (n = 13), relapse (n = 3), and MAC-related death (n = 4). A positive sputum acid-fast bacillus smear at the start of treatment was an independent predictor of an unfavorable microbiologic response.
In many countries, including Korea, Mycobacterium avium complex (MAC), which includes Mycobacterium avium and Mycobacterium intracellulare, is the most common etiology of lung disease caused by nontuberculous mycobacteria (NTM).1,2 Currently, the accepted standard therapy for patients with MAC lung disease involves the use of a macrolide-based multidrug regimen that consists of a macrolide (clarithromycin or azithromycin), a rifamycin (rifampicin or rifabutin), and ethambutol with or without initial use of streptomycin or amikacin.3,4 However, available data on macrolide-based therapy demonstrate that successful eradication of MAC pulmonary infection is achieved in only 60% of human immunodeficiency virus (HIV)-negative patients.5
In Korea, the Korean Academy of Tuberculosis and Respiratory Diseases recommends a combination antibiotic therapy that includes daily clarithromycin, rifampicin, and ethambutol with or without initial use of streptomycin.6 At our institution, we typically prescribe this triple-drug regimen for the treatment of MAC lung disease. Furthermore, streptomycin has actively been used in patients with radiographically extensive or cavitary disease, especially when accompanied by positive sputum smears.7 In the present study, we evaluated the efficacy of this standardized combination antibiotic therapy and the factors that might affect unfavorable microbiologic responses in patients with MAC pulmonary disease.
We retrospectively reviewed the medical records of all patients treated for MAC lung disease at the Samsung Medical Center (a 1,250-bed referral hospital in Seoul, South Korea) between January 2003 and December 2006. During this period, 248 patients were newly diagnosed with MAC lung disease. All patients met the diagnostic criteria for NTM lung disease according to standards set by the American Thoracic Society in 1997.3 No patients had previously been treated for MAC lung disease before visiting our hospital.
NTM lung disease may progress very slowly. Furthermore, some patients do not require treatment, whereas others require combination antibiotic therapy, including parenteral agents. After discussing this information with patients, we implemented an observation period of at least 6-12 months with no antibiotic treatment. When the disease was clearly recognized as being progressive, patients received a standardized combination antibiotic therapy following hospitalization. In patients with substantial symptoms and/or advanced or progressive radiographic abnormalities, antibiotic therapy was initiated immediately.8
Out of 248 patients with MAC lung disease, 121 patients (49%) did not receive antibiotic therapy, and 127 patients (51%) received combination antibiotic therapy by the end of September 2008. Of these 127 patients who initiated combination antibiotic therapy, 31 patients were excluded because they had received antibiotic therapy for less than 12 months at the time of analysis. These included MAC-unrelated death (n = 3), default (n = 12), transfer out (n = 5), and still on treatment (n = 11). However, 3 patients who died of MAC lung disease were included in the study, even though they were on less than 12 months of antibiotic therapy. Therefore, a total of 96 patients were included in the study. Permission was obtained from the institutional review board of Samsung Medical Center to review and publish information from the patients' records. Informed consent was waived because of the retrospective nature of the study.
Smears for microscopic examination were prepared from concentrated specimens and stained with auramine-rhodamine. Smears were then examined under a fluorescent microscopy. Samples positive for acid-fast bacilli (AFB) were reviewed after staining by using the carbol fuchsin staining method. The results of smear microscopy were reported semiquantitatively. A positive smear was defined as one with > 1 AFB per 100 high-power fields.9
Respiratory specimens were decontaminated using N-acetyl-L-cysteine/2% NaOH, and processed specimens were plated on 3% Ogawa medium (Shinyang, Seoul, Korea). Inoculated tubes were incubated at 37℃ and then inspected weekly for 8 weeks. All AFB isolates were assessed to distinguish between M. tuberculosis and NTM with a commercially available polymerase chain reaction-based assay system (MTB-ID, M&D Inc., Wonju, Korea). NTM species were identified using a polymerase chain reaction and restriction fragment length polymorphism methods based on the rpoB gene, as described previously (Myco-ID, M&D Inc., Wonju, Korea).2
Clarithromycin susceptibility was tested at the Korean Institute of Tuberculosis. Minimal inhibitory concentrations of clarithromycin were determined using the broth microdilution method and interpreted according to the Clinical and Laboratory Standards Institute guidelines.10 Isolates with minimal inhibitory concentrations of 32 µg/mL or greater were considered resistant.10 Methods for determining broth microdilution minimal inhibitory concentration were not established in Korea during the early study period, therefore, isolates recovered from only 68 of 96 patients (71%) could be tested for susceptibility to clarithromycin.
Chest radiography and high-resolution computed tomography (HRCT) findings were classified as showing either upper lobe cavitary disease or nodular bronchiectatic disease.11-13 A combination of cavities, consolidation, and pleural thickening in the upper lobes was considered upper lobe cavitary disease, regardless of whether reticulonodular opacities were present. Bilateral bronchiectasis and nodular changes that were observed predominantly in the middle and lower lung zones without visible cavities in the upper lobes were considered nodular bronchiectatic disease. When the disease did not belong to either the upper lobe cavitary or the nodular bronchiectatic forms, it was deemed unclassifiable.11-13 Initial and available follow-up HRCT scans were reviewed by two of the authors (Sim YS and Park HY). Differences in observed findings were resolved by consensus based on five radiographic features: cavitary disease, bronchiectasis, nodules, consolidation, and tree-in-bud appearance.14
All patients who began antibiotic therapy received a standardized combination antibiotic therapy consisting of clarithromycin (1,000 mg/day), rifampicin (450 mg for patients who were < 50 kg or 600 mg for patients who were ≥ 50 kg), and ethambutol (25 mg/kg for 2 months, then 15 mg/kg/day).3 These drugs were administered on a daily basis. Streptomycin was given intramuscularly at 10-15 mg/kg (500-1,000 mg) three times per week for the first 3-6 months, as far as tolerated in patients with AFB smear-positive sputum or cavitation on chest radiography. This regimen usually continued for a total treatment duration of 24 months, including at least 12 months after sputum culture conversion. Sputum smear and culture examinations were performed monthly for the first six months and then at two- to three-month intervals until the end of treatment.
Sputum conversion was defined as three consecutive negative cultures within 6 months, with the time of conversion defined as the date of the first negative culture. If patient could not expectorate sputum during the treatment duration, the sputum was considered to have converted to negative. Sputum relapse was defined as two consecutive positive cultures after sputum conversion.15,16
For the purpose of these analyses, a favorable microbiologic response was defined as sputum conversion and maintenance of negative sputum cultures for more than 12 months. An unfavorable microbiologic response was defined as follows: 1) no sputum conversion, 2) initial sputum conversion with sputum relapse, or 3) death related to MAC lung disease.
Because a majority of the data did not follow a normal distribution, all results presented herein are expressed as the median and interquartile range (IQR) or the number (percentage) of patients. Categorical variables were analyzed using the Pearson χ2-test or Fisher's exact test. Continuous variables were analyzed using a Mann-Whitney U-test. Multiple logistic regression was performed to assess the effects of independent factors on final treatment outcome (excluding uncertain outcomes). Variables with a p value less than 0.2 in the univariate analysis were considered for the multivariate analysis. All P values were two-sided, with p < 0.05 considered to be statistically significant. Analyses were executed using PASW, version 17.0 for Windows (SPSS Inc, Chicago, IL, USA)
A total of 96 patients [40 males and 56 females, median age 59 years (IQR, 52-68 years)] with MAC lung disease who had received combination antibiotic therapy were included in the study. None of the 96 patients showed positive for HIV. Patient characteristics are summarized in Table 1. All patients had respiratory symptoms such as purulent sputum (n = 90; 94%), cough (n = 84; 88%), or hemoptysis (n = 28; 29%). Etiologic organisms included M. intracellulare in 56 patients (58%) and M. avium in 40 patients (42%). A total of 66 patients (69%) had a positive AFB smear at the time of antibiotic therapy initiation. Cavities (either single or multiple) were visible on chest radiography in 37 patients (39%). Finally, 61 patients (64%) had the nodular bronchiectatic form, 25 patients (26%) had the upper lobe cavitary form, and 10 patients (10%) had unclassifiable variants.
Drug susceptibility tests were performed as described previously on MAC isolates recovered from 68 patients, and none of the MAC isolates showed resistance to clarithromycin.
The median duration of antibiotic therapy was 24 months (IQR, 18-24 months). Streptomycin was given to 72 patients (75%) for median 4.5 months (IQR, 3-6 months).
In all, 28 patients (29%) changed treatment regimens due to side-effects. Of these, 23 (24%) stopped taking ethambutol due to decreased visual acuity or skin rash after a median duration of 6 months (IRQ, 3-12 months). A reduction in the dose of clarithromycin to 500 mg/day was required in 10 patients due to gastrointestinal disturbance after a median duration of 1.6 months (IRQ, 0.2-4.2 months). Five patients experienced side-effects associated with both ethambutol and clarithromycin.
Surgical resection was performed on eight patients (8%). The indications for surgery included a lack of sputum conversion (n = 6) and complications such as recurrent hemoptysis despite negative sputum conversion (n = 2). Pulmonary resections included lobectomy in three patients, segmentectomy in two patients, lobectomy plus segmentectomy in one patient, lobectomy plus wedge resection in one patient, and pneumonectomy in one patient. Negative sputum culture conversion was achieved in six patients.
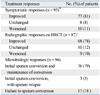
As shown in Table 2, response rates were 81%, based on symptoms, and 78% based on HRCT findings. At the start of treatment, the median ESR was 45.0 mm/hr (IQR, 28.5-75.0 mm/hr). ESR levels decreased to a median of 14.0 mm/hr (IQR, 7.0-34.0 mm/hr) after 12 months of treatment (p < 0.001).
Among the 96 patients with MAC lung disease who received combination antibiotic therapy, the initial sputum conversion rate was 82% (79/96) and the median time until sputum conversion was one month (IQR, 1-2 months). Of the 79 patients who showed initial sputum conversion, 61 patients completed antibiotic treatment and were followed for a median of 6.5 months (IQR, 3.0-12.3 months). Sputum relapse occurred after treatment completion in three patients (5, 9, and 16 months after treatment completion, respectively). Eighteen patients remained on the treatment for 19.2 months (IQR, 16.1-22.5 months) at the time of analysis. Therefore, the overall favorable microbiologic response rate was 79% (76/96). Twenty patients (21%) had unfavorable microbiologic responses, including failure to sputum conversion (n = 13), relapse (n = 3), and MAC-related death (n = 4).
Based on the clinical variables included in the univariate comparison between favorable and unfavorable microbiologic response groups, the final multiple logistic regression model revealed that a positive sputum AFB smear at the start of treatment (odds ratio, 9.60; 95% confidence interval, 1.02-90.19; p = 0.048) was independently associated with an unfavorable microbiologic response (Table 3).
We investigated the efficacy of standardized combination antibiotic therapy for the treatment of patients with MAC lung disease. Treatment included oral clarithromycin, rifampicin, and ethambutol in combination with the aggressive use of intramuscular streptomycin during the initial treatment period. The overall favorable microbiologic response rate was 79% (76/96), and we found that a positive sputum AFB smear at the start of treatment was independently associated with an unfavorable microbiologic response.
The optimal treatment regimen for MAC lung disease has yet to be fully established.4,17 Field, et al.5 published a comprehensive literature review of potential treatments for MAC lung disease. Overall, treatment outcomes have improved with the addition of macrolides to the standard regimen; however, the average culture conversion rate from 12 studies using the macrolide-containing regimen was only about 60%.5 In our study, the favorable microbiologic response rate was 79%. This relatively high treatment response rate is comparable to data from previous studies in Japan.18,19 In these Japanese studies, all patients received clarithromycin, rifampicin, and ethambutol daily, and 65-70% of patients were treated with an aminoglycoside such as streptomycin or kanamycin for the initial 2-6 months of therapy. In these studies, long-term conversion rates were more than 80% in patients infected with clarithromycin-susceptible strains.18,19
The role of aminoglycoside as a companion drug is somewhat unclear. Streptomycin may be useful in patients who have a substantial number of extracellular organisms against which streptomycin is highly active. Included in this group are patients with radiographically extensive or cavitary disease and those with strongly positive sputum AFB smears. A recent prospective randomized controlled study of the clinical efficacy of streptomycin in the treatment of MAC lung disease revealed that sputum conversion rates at the completion of therapy were significantly higher in the streptomycin group who received streptomycin intramuscularly three times per week for the initial 3 months of therapy in combination with clarithromycin, rifampicin, and ethambutol.16 In our study, streptomycin was given for a median of 4.5 months (IQR, 3-6 months) in 72 patients (75%). The use of this aggressive treatment strategy depended largely on the patients' characteristics. We used streptomycin in patients with a positive sputum smear and/or cavitary disease. Among the 96 patients, 66 (69%) had a positive AFB smear and 37 (39%) had a cavity (or cavities) visible on chest radiography at the start of antibiotic therapy.
Some small-scale studies suggest that a three-times-weekly regimen that includes clarithromycin or azithromycin may be as effective as a daily regimen.20,21 However, a large prospective trial showed that a three-times-weekly regimen was not effective in producing negative culture conversion.14 Negative culture conversion was achieved in only 13% of patients (4% in the cavitary disease group and 24% in the non-cavitary disease group), although culture improvement rates, i.e., reduction in colony counts, were 44% (20% in the cavitary disease group and 71% in the non-cavitary disease group).14 The Korean Academy of Tuberculosis and Respiratory Diseases recommends a daily antibiotic therapy for MAC lung disease.6 Therefore, all patients in our study who required antibiotic therapy were given a daily regimen according to the national guidelines.
With respect to treatment duration, it is usually recommended that antibiotic therapy be continued for 12 months once the patient converts to a negative culture.3,4 The overall treatment period in our study was typically 24 months. In some studies, however, high relapse rates have been reported despite long-term antibiotic therapy of ≥ 24 months.22 Genotyping research has demonstrated that in patients with nodular bronchiectatic forms of MAC lung disease, multiple and/or repeated infections and frequent recurrence may be due to reinfection with a genetically different strain or relapse with the original strain.23,24 Recent studies have provided evidence that a patient's home environment, e.g., bathrooms, may serve as a continuing source of pulmonary infection caused by MAC.25,26 When patients repeatedly inhale MAC organisms during treatment, the efficacy of antibiotic therapy may be reduced. Future studies examining the clinical relevance of these situations should be performed.
As the American Thoracic Society guidelines pointed out, one of the most difficult questions may be when to start antibiotic therapy in patients with MAC lung disease.3,4 The decision to begin treatment is made by weighing the anticipated benefits and risks. The decision is relatively easy in patients with profound symptoms and destructive lesions; however, the decision is difficult in patients with mild symptoms and non-advanced lesions. Factors that must be considered include the patients' age, whether the symptoms are mild or equivocal, and the presence of comorbities.27 In all cases, close observation is necessary if treatment is not performed.
There are few studies in which patients with certain characteristics show disease progression. One study from Japan found that 60% of patients showed disease progression and 40% of patients were stable during a mean observation period of 28 months.28 In the present study, the conversion rate was significantly higher in smear-negative cases, suggesting that the earlier the treatment starts, the better the outcomes will be. However, prolonged antibiotic treatment may not be necessary in patients in the early stages of infection. This is a real challenge to clinicians in daily practice. Further studies are needed to determine when to start antibiotic therapy.
The present study has many limitations that are inherent to all retrospective, noncomparative studies conducted at a single center. We did not calculate appropriate power or sample size for this study at the design stage. Our restrospective study may have less power (less than 80%) to detect predictors of favorable responses if the expected proportion of favorable response was 0.2, and 95% of the patients with the favorable category of a predictor to favorable response resulted in favorable response, and the candidate predictors are not correlated. As observed therapy was not performed directly for patients with NTM lung disease, the possibility of poor compliance of treatment regimen could not be completely excluded in this retrospective study. In addition, the present study included patients with newly diagnosed MAC lung disease, and no patients were infected with clarithromycin-resistant MAC isolates. Therefore, our high treatment response rates may not be generalized to patients with a previous treatment history or those infected with clarithromycin-resistant isolates. Most importantly, we cannot determine whether a favorable microbiologic response will continue. Of the 76 patients who achieved culture-negative sputum for more than 12 months, 61 completed their antibiotic therapy and underwent follow-up for a median of only 6.5 months. Longer follow-up times are necessary to fully assess disease relapse over time.
In conclusion, standardized combination antibiotic therapy consisting of clarithromycin, rifampicin, and ethambutol with or without initial use of streptomycin is effective in treating patients with newly diagnosed MAC lung disease. Further studies are needed to address several issues regarding optimal timing of antibiotic therapy, treatment regimens, and treatment duration.
Figures and Tables
Table 1
The Clinical and Radiographic Characteristics of 96 Patients with Mycobacterium avium Complex Lung Disease

ACKNOWLEDGEMENTS
This work was supported by a grant of the Korea Science and Engineering Foundation (R01-2008-000-20839-0).
References
1. Marras TK, Daley CL. Epidemiology of human pulmonary infection with nontuberculous mycobacteria. Clin Chest Med. 2002. 23:553–567.
2. Koh WJ, Kwon OJ, Jeon K, Kim TS, Lee KS, Park YK, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest. 2006. 129:341–348.

3. Medical Section of the American Lung Association. Diagnosis and treatment of disease caused by nontuberculous mycobacteria. This official statement of the American Thoracic Society was approved by the Board of Directors, March 1997. Am J Respir Crit Care Med. 1997. 156:S1–S25.
4. Griffith DE, Aksamit T, Brown-Elliott BA, Catanzaro A, Daley C, Gordin F, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med. 2007. 175:367–416.

5. Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004. 126:566–581.

6. Korean Academy of Tuberculosis and Respiratory Diseases (KATRD). KATRD. Nontuberculous mycobacterial lung disease. Guideline of management of tuberculosis. 2005. Seoul: KATRD;136–146.
7. Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci. 2005. 20:913–925.

8. Jeon K, Kwon OJ, Lee NY, Kim BJ, Kook YH, Lee SH, et al. Antibiotic treatment of Mycobacterium abscessus lung disease: a retrospective analysis of 65 patients. Am J Respir Crit Care Med. 2009. 180:896–902.

9. Diagnostic Standards and Classification of Tuberculosis in Adults and Children. This official statement of the American Thoracic Society and the Centers for Disease Control and Prevention was adopted by the ATS Board of Directors, July 1999. This statement was endorsed by the Council of the Infectious Disease Society of America, September 1999. Am J Respir Crit Care Med. 2000. 161:1376–1395.
10. Clinical and Laboratory Standards Institute. Document No. M24-A. Susceptibility testing of mycobacteria, nocardiae, and other aerobic actinomycetes; Approved Standard. 2003. Wayne, PA: CLSI.
11. Chung MJ, Lee KS, Koh WJ, Lee JH, Kim TS, Kwon OJ, et al. Thin-section CT findings of nontuberculous mycobacterial pulmonary diseases: comparison between Mycobacterium avium-intracellulare complex and Mycobacterium abscessus infection. J Korean Med Sci. 2005. 20:777–783.

12. Koh WJ, Yu CM, Suh GY, Chung MP, Kim H, Kwon OJ, et al. Pulmonary TB and NTM lung disease: comparison of characteristics in patients with AFB smear-positive sputum. Int J Tuberc Lung Dis. 2006. 10:1001–1007.
13. Kitada S, Kobayashi K, Ichiyama S, Takakura S, Sakatani M, Suzuki K, et al. Serodiagnosis of Mycobacterium avium complex pulmonary disease using an enzyme immunoassay kit. Am J Respir Crit Care Med. 2008. 177:793–797.

14. Lam PK, Griffith DE, Aksamit TR, Ruoss SJ, Garay SM, Daley CL, et al. Factors related to response to intermittent treatment of Mycobacterium avium complex lung disease. Am J Respir Crit Care Med. 2006. 173:1283–1289.

15. Kobashi Y, Matsushima T. The effect of combined therapy according to the guidelines for the treatment of Mycobacterium avium complex pulmonary disease. Intern Med. 2003. 42:670–675.

16. Kobashi Y, Matsushima T, Oka M. A double-blind randomized study of aminoglycoside infusion with combined therapy for pulmonary Mycobacterium avium complex disease. Respir Med. 2007. 101:130–138.

17. Kasperbauer SH, Daley CL. Diagnosis and treatment of infections due to Mycobacterium avium complex. Semin Respir Crit Care Med. 2008. 29:569–576.

18. Tanaka E, Kimoto T, Tsuyuguchi K, Watanabe I, Matsumoto H, Niimi A, et al. Effect of clarithromycin regimen for Mycobacterium avium complex pulmonary disease. Am J Respir Crit Care Med. 1999. 160:866–872.

19. Fujikane T, Fujiuchi S, Yamazaki Y, Sato M, Yamamoto Y, Takeda A, et al. Efficacy and outcomes of clarithromycin treatment for pulmonary MAC disease. Int J Tuberc Lung Dis. 2005. 9:1281–1287.
20. Griffith DE, Brown BA, Cegielski P, Murphy DT, Wallace RJ Jr. Early results (at 6 months) with intermittent clarithromyc-inincluding regimens for lung disease due to Mycobacterium avium complex. Clin Infect Dis. 2000. 30:288–292.

21. Griffith DE, Brown BA, Girard WM, Griffith BE, Couch LA, Wallace RJ Jr. Azithromycin-containing regimens for treatment of Mycobacterium avium complex lung disease. Clin Infect Dis. 2001. 32:1547–1553.

22. Kobashi Y, Matsushima T. The microbiological and clinical effects of combined therapy according to guidelines on the treatment of pulmonary Mycobacterium avium complex disease in Japan - including a follow-up study. Respiration. 2007. 74:394–400.

23. Wallace RJ Jr, Zhang Y, Brown BA, Dawson D, Murphy DT, Wilson R, et al. Polyclonal Mycobacterium avium complex infections in patients with nodular bronchiectasis. Am J Respir Crit Care Med. 1998. 158:1235–1244.

24. Wallace RJ Jr, Zhang Y, Brown-Elliott BA, Yakrus MA, Wilson RW, Mann L, et al. Repeat positive cultures in Mycobacterium intracellulare lung disease after macrolide therapy represent new infections in patients with nodular bronchiectasis. J Infect Dis. 2002. 186:266–273.

25. Nishiuchi Y, Maekura R, Kitada S, Tamaru A, Taguri T, Kira Y, et al. The recovery of Mycobacterium avium-intracellulare complex (MAC) from the residential bathrooms of patients with pulmonary MAC. Clin Infect Dis. 2007. 45:347–351.

26. Nishiuchi Y, Tamura A, Kitada S, Taguri T, Matsumoto S, Tateishi Y, et al. Mycobacterium avium complex organisms predominantly colonize in the bathtub inlets of patients' bathrooms. Jpn J Infect Dis. 2009. 62:182–186.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download