Abstract
Purpose
Nemaline myopathy (NM) is a clinical heterogeneous congenital myopathy characterized by the presence of subsarcolemmal or cytoplasmic rod-like structures that call nemaline bodies in the muscle fibers. The purpose of this study was to investigate the clinical diversity and pathological features of Korean patients with NM.
Materials and Methods
Eight patients underwent analyses of clinical manifestations by a structured protocol. Diagnoses were established by a muscle biopsy.
Results
Two patients had the typical congenital type, which exhibited neonatal hypotonia and delayed motor milestone, and five patients had the childhood onset type, which exhibited mild gait disturbance as a first symptom. One patient had the adult onset type, which showed acute respiratory failure. Limb weakness was proximal-dominant occurred in six patients. Hyporeflexia was observed in most patients. Elongated faces and high arched palates and feet were also observed. On light microscopy, the nemaline bodies were observed in type 1 and 2 fibers. All patients showed type 1 predominance and atrophy. In the two cases in which ultrastructural studies were performed, typical nemaline rods and disorganized myofibrillar apparatus were detected.
Conclusion
In conclusion, the eight Korean patients in this study with NM shared common clinical expressions such as proximal limb weakness, reduced deep tendon reflex, and dysmorphic features. This study, however, showed that clinical heterogeneity ranged from typical congenital, mildly affected childhood to the adult onset form with acute respiratory failure. The pathological findings in this study were in accordance with those of other previous reports.
Nemaline myopathy (NM) is an uncommon congenital muscle disease with an incidence of 0.02 per 1,000 live births.1 According to the degree of muscle weakness, severity, and age at onset, five forms have been clinically defined by the European Neuromuscular Center (ENMC) International Consortium on NM.2-4 Five clinical subtypes (severe, intermediate, typical congenital, mild childhood, and adult onset) reflect the clinical heterogeneity of this disease. The most common classical form is characterized by onset in early infancy or childhood with hypotonia or general weakness predominantly affecting facial, axial, and proximal limb muscles. The course is typically static or only slowly progressive, and the degree of cardiorespiratory involvement is the main prognostic factor.5 Cases are often sporadic, but some exhibit either autosomal recessive or dominant patterns of inheritance. The characteristic pathognomic feature is the presence of intrasarcolemmal rods, which are seen on light microscopy visualized with modified Gomori trichrome stains, and electron dense nemaline bodies of Z-band origin on ultrastructural examination.6 Usually, the rods are present in the type 1 fibers, and the proportion of fibers that contain rods can also vary among individuals.2 Another important histopathologic feature frequently observed in NM is type 1 predominance.
Over the past few years, several cases have been reported in Korea but little attention has been given to the clinicopathological features of NM. The purpose of this study is to investigate the clinical diversity and pathological features of Korean patients with NM.
A total of 8 patients were included in this retrospective investigation and diagnosed with NM at our hospital between 1993 and 2006. Diagnosis was based on clinical examination, course of the disease, family history, serum creatine kinase levels, electromyography, and muscle biopsy. Study protocol data collected from each patient included: 1) detailed personal history (age at onset, initial symptom or sign, developmental delay, and clinical course), 2) clinical presentations (distribution of muscle weakness and atrophy, progression pattern, cardiac or respiratory involvement, dysphagia, and mental retardation), 3) dysmorphic features (pseudohypertrophy, high arched palate and foot, elongated face, and spinal deformity), 4) laboratory data (serum creatine kinase, electromyography and nerve conduction velocity, muscle biopsy), and 5) muscle power (manual muscle testing).
All patients underwent an open biopsy of the deltoids or biceps under local or general anesthesia. Muscle samples were frozen in liquid nitrogen immediately after removal and stored at -70℃ and remained so until time of use. Transverse serial frozen muscle sections were stained with hematoxylin and eosin (H&E), modified Gomori trichrome, adenosine triphosphatase (ATPase, at pH 9.4, 4.6, and 4.3), and nicotinamide adenine dinucleotide (NADH)-tetrazolium reductase (TR) stains.
Details of each patient are shown in Table 1. Six male and two female patients were investigated. The age at the time of the muscle biopsy varied from 14 to 43 years. Two patients were familial cases and the others were sporadic.
Five patients were infants or children when lower limb weakness began without delayed motor milestone. Two patients, however, had congenital mild hypotonia and weakness during the neonatal period. One (patient No. 2) of two patients with neonatal hypotonia and weakness started to walk unassisted at 36 months of the age and the other (patient No. 3) began at 7 years. In only one patient, dyspnea was the first symptom that began during adulthood without preceding symptoms, and acute respiratory insufficiency developed within the course of two months. Mental development was normal in all patients. These 5, 2, and 1 patients were classified as childhood onset, typical congenital, and adult onset types, respectively, according to the ENMC International Consortium on NM.
The lower extremities were most often initially affected by limb weakness and distribution of muscle weakness was remarkably in proximal parts. However, one patient was weaker in distal limbs than proximal and both were equal on manual muscle testing. Weakness in the neck flexor and facial muscles was observed in two typical congenital patients and the one adult onset patient.
High arched palates (n = 6), high arched feet (n = 5), and elongated faces (n = 4) were observed as dysmorphic features. Most patients exhibited reduced tendon reflexes, and scoliosis was observed in one patient. Other orthopedic abnormalities such as arthrogryposis were not found. Cardiomyopathy and opthalmoplegia were not exhibited. The clinical course was static or slowly progressive except for the adult onset patient.
A nerve conduction study showed normal results in most of the patients. A needle electromyography study showed a combination of small brief motor unit action potentials with reduced recruitment in six patients as well as denervating potential in two of these. Two patients showed normal findings. The mean serum creatine kinase level was 107 IU/L (range 25-369 IU/L).
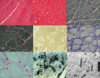
Muscle biopsies of all 8 patients showed similar changes. Microscopic examination revealed normal fascicular architecture with no endomysial or perimysial fibrosis and adipose tissue infiltration (Fig. 1A). There was a mild variation in fiber size without central localization nuclei. Modified Gomori trichrome stains showed characteristic purple-colored rods in the cytoplasm and subsarcolemmal region, which were more prominent in type 1 fibers (Fig. 1B and C). Type 1 fiber predominance was observed in all patients, which was accompanied by selective type 1 fiber atrophy in seven patients (Fig. 1D and E). Nemaline rods were confined to type 1 fibers in five of the eight biopsies in which fiber type distribution of rods was determined (Fig. 1F and G). Rods were never confined to type 2 fibers. Type 2 fiber predominance was not seen. Intranuclear rods were not identified in any case. There was no evidence of central cores, minicores, central nuclei, reducing bodies, or target fibers in any of the eight patients. In the two cases where ultrastructural studies were done, typical nemaline rods and disorganized myofibrillar apparatus were detected (Fig. 1H and I).
NM was originally described independently by Shy, et al.8 and Conen, et al.7 in 1963 as a non-progressive myopathy with a distinctive morphologic abnormality designated as myogranules or rods of thread-like fibrous material. NM shares common clinical expressions such as proximal limb weakness, slow progression, and characteristic dysmorphic features shown with other congenital myopathies. NM can be categorized into five subtypes on the basis of its clinical features as follows: by the pattern of weakness, age at onset, or respiratory involvement. Thus, clinical presentations of NM are heterogeneous. The typical form of NM is usually autosomal recessive and it presents with congenital or infantile hypotonia, weakness, and often feeding difficulties are present during the neonatal period or first year of life.9 In cases with profound weakness and hypotonia during the neonatal period, strength often improves with age, leading to delayed attainment of gross motor skills but most of these patients are able to lead an independent life. Severe and intermediate congenital forms may have severe weakness and hypotonia with a rapidly progressive course leading to respiratory failure.10 Of mild childhood forms, the mildest end of the spectrum are patients with similar clinical findings to the typical forms, but with a childhood onset of symptoms.11 At later ages, these mild cases can be indistinguishable from typical cases with the age at onset as the only differentiating factor.11 There is also a progressive adult onset form that represents a separate, quite heterogeneous group of patients in terms of clinical presentation with an onset in the third to sixth decade. The adult onset form is characterized by rather selective acute or subacute respiratory dysfunction without preceding symptoms with sporadic or autosomal recessive inheritance.12
Our study also showed clinical diversity of NM. Two patients had the typical congenital type of NM which exhibited neonatal hypotonia and delayed motor milestones, and five patients had the childhood onset type which exhibited mild proximal lower extremity weakness as a first symptom. One patient had the adult onset type which showed acute respiratory failure. There was a marked overlap in clinical features between two typical and five childhood type patients, but delayed motor milestones, facial involvement, weakness of neck flexor muscle, and neonatal hypotonia presented characteristically in typical congenital patients.
The seven typical congenital and childhood onset patients exhibited static or slowly progressive clinical courses. Although these subtypes have been described to be benign clinical courses, there are a number of reports describing patients with progressive muscle weakness and respiratory failure.13 In NM, early mortality was not invariably due to hypotonia or severe weakness but respiratory insufficiency.3 Therefore, baseline and follow-up pulmonary function testing should be performed.
In considering muscle pathology, analysis of the biopsies in our patients revealed that light microscopy is a reliable method for the diagnosis of NM. Nemaline rods are best demonstrated in frozen sections stained with the modified trichrome technique, in which they appear as reddish-purple granules measuring 2-7 µm in length.
Our series also showed typical nemaline rods which were more prominent in type 1 fibers. There were fiber size variations and type 1 fiber predominance with selective type 1 fiber atrophy. Nemaline rods were confined to type 1 fibers in more than half the number of our cases. On the other hand we did not find rods confined to type 2 fibers.
It is known that rods are found predominantly in type 1 fibers and affected fibers are often somewhat smaller than normal.6 As in other congenital myopathies, the proportion of fiber types deviated and type 1 predominance is frequently observed.14 Studies performed on consecutive biopsies suggested a transformation of fiber type based on the disappearance of type 2 fibers with age.13 Type 1 fiber predominance has been suggested as a primary cause of muscle weakness in NM.15 Accordingly, a correlation exists between the severity of clinical manifestations and alterations in size and proportion of type 1 myofibers.6
The number of fibers containing rods and the number of rods vary widely between patients and even between different muscles in individual cases.16 In the vast majority of cases the rods are located exclusively in the cytoplasm, and approximately 10% of the cases also show intranuclear deposit.17 Although we could not find intranuclear rods in our cases, prior reports suggested that the intranuclear rods are associated with early presentation, more rapid progression, and a worse prognosis.10,16,18,19 However, rod location within fibers or the subsarcolemmal region and the number of rods do not correlate with the clinical severity or course of illness.16,17
Genetically, disease-causing mutations have recently been identified in five different genes, all of which encode protein components of muscle thin filaments as follows: α-tropomyosin (TPM3),20 nebulin (NEB),21 α-actin (ACTA1),22 β-tropomyosin (TPM2),23 and troponin T1 (TNNT1).24 Genes for these proteins have been localized and mutations are fully characterized.11,25 Nebulin gene mutations are seen most commonly in autosomal recessive cases and these patients present as typical congenital NM.21 Some authors demonstrated with linkage studies that nebulin gene mutations at 2q21.2-q22 are responsible for 50% of the cases of NM.21 TPM3 mutations have been described in rare cases of dominant and recessive cases of NM, and rarely are TPM2 and TNNT1 also implicated.20 ACTA1 mutations at 1q42 are reported to comprise 10% of the cases of NM,22 and are more common in severe cases of NM.1
There are also several cases in the literature of acquired illnesses resulting in nemaline rod myopathy, and there appears to be a strong association with HIV infection.26,27 In the presence of HIV, the virus itself may trigger reactions that cause de novo genetic mutations resulting in nemaline formation.28 The reported HIV prevalence rate among adults aged in 15-49 years in Korea is below 0.1%.29
In conclusion, the eight Korean patients with NM shared common clinical expressions such as proximal limb weakness, reduced deep tendon reflex, and dysmorphic features. This study, however, showed that clinical heterogeneity ranged from typical congenital, mildly affected childhood to adult onset forms with acute respiratory failure. The characteristic pathological findings of nemaline rods and type 1 predominance were in accordance with those of previous reports as well. To further characterization, genetic analysis will be necessary.
Figures and Tables
Fig. 1
Pathologic findings of nemaline myopathy. (A and B) Hematoxylin and eosin staining (×50, ×100) reveals mild to moderate fiber size variation. Nemaline rods are not seen. (C and D) Numerous subsarcolemmal and cytoplasmic rods are apparent on a modified Gomori-trichrome stain (×100, ×200). (E) ATPase stain at pH 4.3 (×100) illustrates marked type 1 fiber predominance and hypotrophy. (F and G) NADH-TR stain (×200) shows selective type 1 fiber atrophy and modified Gomori-trichrome stain (×400) demonstrates selective rod formation in hypotrophic type 1 fibers. (H and I) Electron micrograph shows nemaline rods in cytoplasm and disorganized sarcomeric architecture with focal myofibrillar disarray.
References
1. Agrawal PB, Strickland CD, Midgett C, Morales A, Newburger DE, Poulos MA, et al. Heterogeneity of nemaline myopathy cases with skeletal muscle alpha-actin gene mutations. Ann Neurol. 2004. 56:86–96.

2. Wallgren-Pettersson C, Laing NG. Report of the 83th ENMC International Workshop: 4th Workshop on Nemaline Myopathy, 22-24 September 2000, Naarden, The Netherlands. Neuromuscul Disord. 2001. 11:589–595.
3. Ryan MM, Schnell C, Strickland CD, Shield LK, Morgan G, Iannaccone ST, et al. Nemaline myopathy: a clinical study of 143 cases. Ann Neurol. 2001. 50:312–320.

4. Wallgren-Pettersson C, Laing NG. Report of the 70th ENMC International Workshop: nemaline myopathy, 11-13 June 1999, Naarden, The Netherlands. Neuromuscul Disord. 2000. 10:299–306.

5. Jungbluth H, Sewry CA, Muntoni F. What's new in neuromuscular disorders? The congenital myopathies. Eur J Paediatr Neurol. 2003. 7:23–30.

6. Katirji B, Kaminski HJ, Preston DC, Ruff RL, Shapiro BE. Bodensteiner JB, Riggs JE, Schochet SS, editors. Neuromuscular disorders in clinical practice. Congenital myopathies. 2002. 1st ed. Woburn: Butterworth-Heinemann;1114–1127.
7. Conen PE, Murphy EG, Donohue WL. Light and electron microscopic studies of "myogranules" in a child with hypotonia and muscle weakness. Can Med Assoc J. 1963. 89:983–986.
8. Shy GM, Engel WK, Somers JE, Wanko T. Nemaline myopathy. A new congenital myopathy. Brain. 1963. 86:793–810.
9. Shimomura C, Nonaka I. Nemaline myopathy: comparative muscle histochemistry in the severe neonatal, moderate congenital, and adult-onset forms. Pediatr Neurol. 1989. 5:25–31.

10. Rifai Z, Kazee AM, Kamp C, Griggs RC. Intranuclear rods in severe congenital nemaline myopathy. Neurology. 1993. 43:2372–2377.

11. Sanoudou D, Beggs AH. Clinical and genetic heterogeneity in nemaline myopathy--a disease of skeletal muscle thin filaments. Trends Mol Med. 2001. 7:362–368.

12. Gyure KA, Prayson RA, Estes ML. Adult-onset nemaline myopathy: a case report and review of the literature. Arch Pathol Lab Med. 1997. 121:1210–1213.
13. Nonaka I, Ishiura S, Arahata K, Ishibashi-Ueda H, Maruyama T, Ii K. Progression in nemaline myopathy. Acta Neuropathol. 1989. 78:484–491.

14. Gurgel-Giannetti J, Reed UC, Marie SK, Zanoteli E, Fireman MA, Oliveira AS, et al. Rod distribution and muscle fiber type modification in the progression of nemaline myopathy. J Child Neurol. 2003. 18:235–240.
15. Volpe P, Damiani E, Margreth A, Pellegrini G, Scarlato G. Fast to slow change of myosin of nemaline myopathy: electrophoretic and immunologic evidence. Neurology. 1982. 32:37–41.
16. Ryan MM, Ilkovski B, Strickland CD, Schnell C, Sanoudou D, Midgett C, et al. Clinical course correlates poorly with muscle pathology in nemaline myopathy. Neurology. 2003. 60:665–673.

17. Kaimaktchiev V, Goebel H, Laing N, Narus M, Weeks D, Nixon R. Intranuclear nemaline rod myopathy. Muscle Nerve. 2006. 34:369–372.
18. Barohn RJ, Jackson CE, Kagan-Hallet KS. Neonatal nemaline myopathy with abundant intranuclear rods. Neuromuscul Disord. 1994. 4:513–520.

19. Goebel HH, Piirsoo A, Warlo I, Schofer O, Kehr S, Gaude M. Infantile intranuclear rod myopathy. J Child Neurol. 1997. 12:22–30.

20. Laing NG, Wilton SD, Akkari PA, Dorosz S, Boundy K, Kneebone C, et al. A mutation in the alphatropomyosin gene TPM3 associated with autosomal dominant nemaline myopathy. Nat Genet. 1995. 9:75–79.

21. Pelin K, Hilpelä P, Donner K, Sewry C, Akkari PA, Wilton SD, et al. Mutations in the nebulin gene associated with autosomal recessive nemaline myopathy. Proc Natl Acad Sci U S A. 1999. 96:2305–2310.

22. Nowak KJ, Wattanasirichaigoon D, Goebel HH, Wilce M, Pelin K, Donner K, et al. Mutations in the skeletal muscle alpha-actin gene in patients with actin myopathy and nemaline myopathy. Nat Genet. 1999. 23:208–212.

23. Donner K, Ollikainen M, Ridanpää M, Christen HJ, Goebel HH, de Visser M, et al. Mutations in the beta-tropomyosin (TPM2) gene--a rare cause of nemaline myopathy. Neuromuscul Disord. 2002. 12:151–158.

24. Johnston JJ, Kelley RI, Crawford TO, Morton DH, Agarwala R, Koch T, et al. A novel nemaline myopathy in the Amish caused by a mutation in troponin T1. Am J Hum Genet. 2000. 67:814–821.

26. Chahin N, Selcen D, Engel AG. Sporadic late onset nemaline myopathy. Neurology. 2005. 65:1158–1164.

27. de Sanctis JT, Cumbo-Nacheli G, Dobbie D, Baumgartner D. HIV-associated nemaline rod myopathy: role of intravenous immunoglobulin therapy in two persons with HIV/AIDS. AIDS Read. 2008. 18:90–94.
28. Colmegna I, Koehler JW, Garry RF, Espinoza LR. Musculoskeletal and autoimmune manifestations of HIV, syphilis and tuberculosis. Curr Opin Rheumatol. 2006. 18:88–95.

29. Shin JW, Park RJ, Aum SS, Choi TY. Analysis of anti-HIV positive rates and false-positive cases in a tertiary care hospital - single institute study. Korean J Blood Transfus. 2009. 20:40–45.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download