Abstract
Purpose
The incidence of Candida bloodstream infections (BSI) has increased over the past two decades. The rank order of occurrence and the susceptibility to antifungals of the various Candida species causing BSI are important factors driving the establishment of empirical treatment protocols; however, very limited multi-institutional data are available on Candida bloodstream isolates in Korea.
Materials and Methods
We investigated the susceptibility to azole antifungals and species distribution of 143 Candida bloodstream isolates recovered from eight university hospitals over a six-month period. Minimal inhibitory concentrations (MICs) of fluconazole, itraconazole, and voriconazole for each isolate were determined by the broth microdilution method of the Clinical and Laboratory Standards Institute (CLSI).
Results
The Candida
species recovered most frequently from the blood cultures was C. albicans (49%), followed by C. parapsilosis (22%), C. tropicalis (14%), and C. glabrata (11%). The MIC ranges for the Candida isolates were 0.125 to 64 µg/mL for fluconazole, 0.03 to 2 µg/mL for itraconazole, and 0.03 to 1 µg/mL for voriconazole. Overall, resistance to fluconazole was found in only 2% of the Candida isolates (3/143), while the dose-dependent susceptibility was found in 6% (8/143). The resistance and dose-dependent susceptibility of itraconazole were found in 4% (6/143) and 14% (20/143) of the isolates, respectively. All bloodstream isolates were susceptible to voriconazole (MIC, ≤ 1 µg/mL).
The incidence of Candida bloodstream infections (BSI) has increased substantially over the past two decades. Candida species are the fourth most frequent source of BSI, accounting for 8-15% of all cases of hospital-acquired sepsis in the USA.1 In Korea, the incidence of Candida-related BSI has been reported to be about 0.012 per 100 admissions in two university hospitals.2 The increased incidence of Candida-related BSI is most likely associated with the growing population of patients undergoing chemotherapy, transplant surgery, and intensive care support.3,4 Candida-related BSI have emerged as a major challenge for hospital patients because they are associated with high morbidity, prolonged hospital stays, high attributable mortality (~40%), and substantial health care costs.1
The rank order of occurrence and antifungal susceptibility of the various species of Candida that cause BSI are important for establishing empirical treatment protocols.5,6 There has been increased concern regarding the possible changes in species distributions and azole susceptibility of Candida bloodstream isolates due to the widespread use of fluconazole over the past decade.4,5 In fact, several surveillance programs have documented variations in these parameters among institutions, localities, and countries.4,5,7-12 In Korea, a nationwide antimicrobial resistance surveillance on clinically relevant bacteria has been conducted since 1997.13 However, a multi-institutional survey of Candida-related BSI has not been performed in Korea, even though fluconazole use has increased significantly over the past ten years.
In this study, the distribution of Candida bloodstream isolates in Korea was analyzed, and the antifungal susceptibility of the isolates to fluconazole, itraconazole, and voriconazole was determined. This is the first nationwide surveillance study of BSI-causing Candida isolates to be conducted in Korea.
During a six-month period from November 2004 to April 2005, Candida bloodstream isolates were prospectively collected at the eight university hospitals in Korea: Chonnam National University Hospital (Gwangju), Yonsei University Medical Center (Seoul), Asan Medical Center (Seoul), Inje University Sanggye Paik Hospital (Seoul), Wonju Christian Hospital (Wonju), Ajou University Hospital (Suwon), Chonbuk National University Hospital (Jeonju), and Pusan National University Hospital (Busan). All isolates were recovered from blood cultures at each of the participating institutions by using their routine culture methods. For all 193 Candida bloodstream isolates that were collected, both the species identification and the antifungal susceptibility testing were performed at the Chonnam National University Hospital. Of these organisms, a total of 143 bloodstream isolates were included in the study in order to analyze the species distribution and for the antifungal susceptibility testing. These organisms were recovered from 138 patients; with five of the patients having two different Candida species identified. Of the 138 patients, 40 (29%) had two or more blood cultures that were positive for the same Candida species, but only one Candida species isolate (the first isolate) from each patient was included. Species identification was based on colony morphology by using CHROMagar Candida (BBL, Becton Dickinson, Sparks, MD, USA) at 35℃, microscopic morphology on cornmeal-Tween 80 agar, and the use of a commercial system (API 20C; bioMérieux, Marcy L'Etoile, France, or the Vitek 2 system; Vitek 2 ID-YST, bioMérieux).
Susceptibility to antifungals was tested by a broth microdilution assay according to the methods of the Clinical and Laboratory Standards Institute (CLSI, document M-27 A2),14 using the following drugs: fluconazole (Pfizer, Inc., New York, NY, USA), itraconazole (Janssen Pharmaceutica, Beerse, Belgium), and voriconazole (Pfizer Global Research & Development, Sandwich, UK). The RPMI-1640 medium without bicarbonate was prepared with L-glutamine and buffered at pH 7.0 with 0.165-M morpholinopropanesulfonic acid (MOPS). Each yeast inoculum suspension was prepared using a spectrophotometer in order to obtain a final concentration of 0.5-2.5 × 103 cells/mL. The trays were incubated in air at 35℃, and the minimal inhibitory concentration (MIC) endpoints were read visually after 48 h. To eliminate the effects of trailing growth, spectrophotometric end points for fluconazole, itraconazole, and voriconazole were also determined after 48 h. Visual and spectrophotometric end points were defined as the lowest drug concentrations that resulted in a prominent decrease in growth and a 50% reduction in optical density, respectively, when compared to the data of the drug-free growth control well.14-16 Quality control was performed by testing the Candida strains recommended by CLSI,14 which were the C. parapsilosis ATCC 22019 and the C. krusei ATCC 6258.
The interpretive susceptibility criteria used for fluconazole and itraconazole were the same as those specified by the CLSI.14 For fluconazole, MICs ≤ 8 µg/mL were considered susceptible, while MICs between 16 and 32 µg/mL were considered susceptible dependent upon dose (SDD), and MICs ≥ 64 µg/mL were considered resistant. Isolates of C. krusei are considered resistant to fluconazole, irrespective of the MIC. For itraconazole, MICs ≤ 0.125 µg/mL were considered susceptible, MICs between 0.25 and 0.5 µg/mL were regarded as SDD, and MICs ≥ 1 µg/mL were considered resistant. For voriconazole, the tentative interpretive breakpoints recently established for its use with Candida species were used (i.e., susceptible, ≤ 1 µg/mL; SDD, 2 µg/mL; and resistant, ≥ 4 µg/mL).17
The frequency of BSI due to various Candida species in the eight different hospitals is shown in Table 1. Among the 143 isolates collected from the 138 patients, 49% were C. albicans, 22% were C. parapsilosis, 14% were C. tropicalis, 11% were C. glabrata, 2% were C. guilliermondii, and 1% was C. krusei. While the predominant species in all but one hospital (hospital G) was the C. albicans, the species distribution of the isolates varied among the hospitals. For example, the frequency of BSI due to C. albicans varied considerably, ranging from 64% (hospital B) to 33% (hospital A) (p < 0.05). In general, however, C. parapsilosis was the most common non-albicans species. In fact, it was the most common isolate in one hospital (hospital G) and the second most common isolate in six of the eight hospitals. C. glabrata was the most common cause (equal to C. albicans) of BSI in only one hospital (hospital A, 33%), and C. tropicalis was the third-or fourth-ranked species in most of the hospitals.
The antifungal susceptibility to fluconazole, itraconazole, and voriconazole was determined for a total of 193 Candida bloodstream isolates from 138 patients. In 40 patients with serial bloodstream isolates of the same Candida species, all strains from the same patient had the same or similar MICs of fluconazole, itraconazole and voriconazole. The in vitro triazole susceptibility results of the 143 isolates from 138 patients (including 133 patients with one Candida species isolate and five patients with two different Candida species isolates) are shown in Table 2. The fluconazole MICs for all of the isolates ranged from 0.125 to 64 µg/mL. The fluconazole MIC90 of the four most common species, C. albicans, C. parapsilosis, C. tropicalis, and C. glabrata, were 0.5, 2, 1, and 32 µ/mL, respectively. All isolates of C. albicans and C. tropicalis were susceptible to fluconazole. Among the 32 C. parapsilosis isolates, two were fluconazole SDD while the others were susceptible. Of 16 C. glabrata isolates, 6% (1/16) were fluconazole resistant, and 38% (6/16) were SDD. Overall, resistance to fluconazole was found in only 2% (3/143) of the Candida isolates (one C. glabrata strain and two C. krusei strains), and dose-dependent susceptibility was found in 6% (8/143) of all the isolates.
The MICs of all bloodstream isolates ranged from 0.03 to 2 µg/mL for itraconazole and from 0.03 to 1 µg/mL for voriconazole. The itraconazole MIC90s for C. albicans, C. parapsilosis, C. tropicalis, and C. glabrata were 0.06, 0.125, 0.25, and 2 µg/mL, respectively. Itraconazole resistance and SDD were observed for 4% (6/143) and 14% (20/143) of the Candida isolates, respectively. Of 16 C. glabrata isolates, 38% (6/16) of them were itraconazole-resistant and 56% (9/16) were SDD. All C. albicans isolates were susceptible to itraconazole. Voriconazole was highly active (MIC90, 0.25 µg/mL) against all of the Candida isolates tested. The MIC50 and MIC90 of voriconazole against C. glabrata were 0.25 and 0.5 µg/mL, respectively. The voriconazole MICs of the two C. krusei isolates were 0.25 and 0.5 µg/mL. Based on our putative breakpoints, all of the isolates were susceptible to voriconazole (MIC ≤ 1 µg/mL).
The treatment of Candida-related BSI was considerably enhanced by the introduction of fluconazole in 1990;18 however, since the introduction of azoles, an increase in the prevalence of C. glabrata and C. krusei bloodstream isolates with reduced susceptibilities to triazole antifungals has been reported, and acquired azole resistance of C. albicans isolates (e.g., in mucosal diseases in acquired immunodeficiency syndrome) has become a major concern.19,20 In this study, the species distribution and azole antifungal susceptibility of Candida species isolates recovered from patients with BSI at eight university hospitals in Korea during a six-month period were evaluated.
Although the non-albicans Candida species represent more than half of all candidemic cases, this study determined that C. albicans is the most frequent etiologic agent of candidemia in Korea. This finding, together with data from other countries,7-11,21,22 confirms that C. albicans is still a leading cause of Candida-related BSI worldwide. Nevertheless, the prevalence of C. albicans (49%) in this study was significantly lower than that in Canada (59%) (p < 0.05); however, it was similar to the prevalence found in Latin America (47%).21 Japan has the lowest reported frequency of C. albicans (41%) among BSI isolates.23
While C. glabrata is the second most common Candida species associated with BSI in the United States (18%) and Canada (20%),21 the C. glabrata-related candidemia represented only 11% of the candidemic episodes in this study, which is comparable to rates reported in Europe (13%) and Latin America (8%).21,24 In addition, the frequency of isolation of intrinsically azole-resistant C. krusei was low (1%) in our study. The higher frequency of C. glabrata and C. krusei in the United States and Canada may be explained in part by their extensive use of relatively low doses of fluconazole (< 400 mg/day).5
In this study, C. parapsilosis was the most common non-albicans species identified, which is consistent with the data from Japan,23 Canada, and South America.25 C. parapsilosis has become increasingly important as a cause of catheter-related BSI,26,27 and its infections are often associated with hyperalimentation due to breaches in catheter care or infection control practices.7,27-29 Pappas et al.30 described the predominance of C. parapsilosis fungemia in children, and they suggested that the high prevalence of C. parapsilosis in children may reflect the aggressive use of intravascular devices to treat neonates. Shin et al.27 also reported that the increased incidence of candidemia due to C. parapsilosis was mainly from central venous catheter-related candidemia that occurs in non-neutropenic patients receiving total parenteral nutrition.
Pfaller et al.21 reported variation in the rank order and frequency of different Candida species over time and by the geographic area. Our study also showed variation in the rank order of occurrence of various BSI-causing species of Candida among different hospitals in Korea. Differences in patient populations, underlying diseases, antifungal therapies, and infection control practices, in addition to other hospital-specific factors, may account for the variation.2
Our data pertaining to fluconazole and itraconazole MICs for four common Candida species (C. albicans, C. parapsilosis, C. glabrata, and C. tropicalis) were similar to those reported in countries participating in the SENTRY Antimicrobial Surveillance Program.5,25 The percent resistance to both fluconazole and itraconazole of each Candida species were also comparable to what was reported in the SENTRY study5,25 (p > 0.05).
Among the species of Candida associated with BSI in this study, resistance to fluconazole and itraconazole was largely limited to the isolates of C. glabrata and C. krusei. The MIC50s of all three azoles for C. glabrata were higher than those observed for most of the other species. The C. glabrata was the main causative agent of BSI in only one of the eight hospitals. The elevated frequency of C. glabrata-related BSI in this particular hospital is worth noting, because of the propensity of this species to develop resistance upon exposure to azole antifungals.31 Therefore, fluconazole may not be the initial therapy of choice for such infections until the susceptibility test results are known, and it may not be an appropriate choice at all in extremely ill patients.32
In this study, none of the C. parapsilosis isolates were azole-resistant; however, two isolates showed decreased susceptibility to both fluconazole (MIC range from 16 to 32 µg/mL) and itraconazole (MIC range from 0.25 to 0.5 µg/mL). The explanation for this is unknown at this time. These findings highlight the need to study the resistance mechanisms of these isolates and to continue our study with a larger number of Candida isolates.
Only a small proportion of the Candida isolates tested in our study showed azole resistance. Voriconazole was quite effective against all Candida species tested, which is in agreement with other reports.33,34 The percentages of fluconazole- and itraconazole-resistant organisms causing candidemia were low (2% and 4%, respectively). None of the C. albicans, C. parapsilosis, or C. tropicalis strains was resistant to triazoles. In addition, 94% (15/16) of the C. glabrata isolates in this study were inhibited by fluconazole at concentrations of 32 µg/mL or less, and thus may still respond to the recommended doses of this agent (≥ 400 mg/day).35 These findings have important implications for the management of Candida-related BSI, especially given that fluconazole is widely used for the treatment of uncomplicated candidemia.36 The negligible incidence of fluconazole resistance among our Candida isolates supports the current belief that antifungal susceptibility testing should not be routinely performed for such common Candida species such as C. albicans, C. parapsilosis, and C. tropicalis; however, it may be required for patients who fail to respond to the initial therapy or who develop breakthrough candidemia while receiving fluconazole prophylaxis.32
In summary, we have shown that the C. albicans is the predominant species in Korean hospitals, and that the azole-resistant BSI-related isolates of Candida are still rare in Korea. These data suggest that the azole antifungals, including fluconazole, remain highly effective agents against most major Candida isolates in Korea. However, we also found variability in the frequency of C. glabrata as a cause of BSI among different hospitals, and decreased susceptibility of a few isolates of C. parapsilosis to fluconazole. Therefore, continuous national surveillance programs are needed in order to identify possible changes in the species distribution and antifungal susceptibility patterns of Candida that may occur due to the increased use of antifungal agents in Korea.
Figures and Tables
Table 1
Species Distribution of Candida Bloodstream Isolates in Each of the Eight Hospitals in Korea
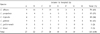
Table 2
Comparison of MICs of Three Antifungal Agents Against 143 Bloodstream Isolates of Candida

*R and SDD, resistant and susceptible-dose dependent, by using the interpretive breakpoint criteria of the CLSI.14
†Isolates of C. krusei are considered resistant to fluconazole, irrespective of the MIC.
References
1. Edmond MB, Wallace SE, McClish DK, Pfaller MA, Jones RN, Wenzel RP. Nosocomial bloodstream infections in United States hospitals: a three-year analysis. Clin Infect Dis. 1999. 29:239–244.

2. Shin JH, Kim MN, Shin DH, Jung SI, Kim KJ, Cho D, et al. Genetic relatedness among Candida tropicalis isolates from sporadic cases of fungemia in two university hospitals in Korea. Infect Control Hosp Epidemiol. 2004. 25:634–640.

3. Verduyn Lunel FM, Meis JF, Voss A. Nosocomial fungal infections: candidemia. Diagn Microbiol Infect Dis. 1999. 34:213–220.

4. Kao AS, Brandt ME, Pruitt WR, Conn LA, Perkins BA, Stephens DS, et al. The epidemiology of candidemia in two United States cities: results of a population-based active surveillance. Clin Infect Dis. 1999. 29:1164–1170.

5. Pfaller MA, Diekema DJ, Jones RN, Sader HS, Fluit AC, Hollis RJ, et al. International surveillance of bloodstream infections due to Candida species: frequency of occurrence and in vitro susceptibilities to fluconazole, ravuconazole, and voriconazole of isolates collected from 1997 through 1999 in the SENTRY antimicrobial surveillance program. J Clin Microbiol. 2001. 39:3254–3259.

6. Hospenthal DR, Murray CK, Rinaldi MG. The role of antifungal susceptibility testing in the therapy of candidiasis. Diagn Microbiol Infect Dis. 2004. 48:153–160.

7. Pfaller MA, Jones RN, Doern GV, Sader HS, Messer SA, Houston A, et al. Bloodstream infections due to Candida species: SENTRY antimicrobial surveillance program in North America and Latin America, 1997-1998. Antimicrob Agents Chemother. 2000. 44:747–751.

8. St Germain G, Laverdière M, Pelletier R, Bourgault AM, Libman M, Lemieux C, et al. Prevalence and antifungal susceptibility of 442 Candida isolates from blood and other normally sterile sites: results of a 2-year (1996 to 1998) multicenter surveillance study in Quebec, Canada. J Clin Microbiol. 2001. 39:949–953.

9. Cuenca-Estrella M, Rodriguez D, Almirante B, Morgan J, Planes AM, Almela M, et al. In vitro susceptibilities of bloodstream isolates of Candida species to six antifungal agents: results from a population-based active surveillance programme, Barcelona, Spain, 2002-2003. J Antimicrob Chemother. 2005. 55:194–199.

10. Samra Z, Yardeni M, Peled N, Bishara J. Species distribution and antifungal susceptibility of Candida bloodstream isolates in a tertiary medical center in Israel. Eur J Clin Microbiol Infect Dis. 2005. 24:592–595.

11. da Matta DA, de Almeida LP, Machado AM, Azevedo AC, Kusano EJ, Travassos NF, et al. Antifungal susceptibility of 1000 Candida bloodstream isolates to 5 antifungal drugs: results of a multicenter study conducted in Säo Paulo, Brazil, 1995-2003. Diagn Microbiol Infect Dis. 2007. 18:399–404.
12. Mokaddas EM, Al-Sweih NA, Khan ZU. Species distribution and antifungal susceptibility of Candida bloodstream isolates in Kuwait: a 10-year study. J Med Microbiol. 2007. 56:255–259.

13. Lee K, Lim CH, Cho JH, Lee WG, Uh Y, Kim HJ, KONSAR group, et al. High prevalence of ceftazidime-resistant Klebsiella pneumoniae and increase of imipenem-resistant Pseudomonas aeruginosa and Acinetobacter spp. in Korea: a KONSAR program in 2004. Yonsei Med J. 2006. 47:634–645.

14. Clinical and Laboratory Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. 2002. 2nd ed. Wayne, PA: Clinical and Laboratory Standards Institute;Approved standard M27-A2.
15. Yi JY, Shin JH, Lee KW, Yong DE, Chae MJ, Suh SP, et al. Evaluation of spectrophotometric broth microdilution method to determine the fluconazole MIC of the Candida Species. Korean J Lab Med. 2002. 22:253–259.
16. Arthington-Skaggs BA, Jradi H, Desai T, Morrison CJ. Quantitation of ergosterol content: novel method for determination of fluconazole susceptibility of Candida albicans. J Clin Microbiol. 1999. 37:3332–3337.

17. Pfaller MA, Diekema DJ, Rex JH, Espinel-Ingroff A, Johnson EM, Andes D, et al. Correlation of MIC with outcome for Candida species tested against voriconazole: analysis and proposal for interpretive breakpoints. J Clin Microbiol. 2006. 44:819–826.

18. Rex JH, Walsh TJ, Sobel JD, Filler SG, Pappas PG, Dismukes WE, et al. Practice guidelines for the treatment of candidiasis. Infectious Diseases Society of America. Clin Infect Dis. 2000. 30:662–678.
19. Voss A, Kluytmans JA, Koeleman JG, Spanjaard L, Vandenbroucke-Grauls CM, Verbrugh HA, et al. Occurrence of yeast bloodstream infections between 1987 and 1995 in five Dutch university hospitals. Eur J Clin Microbiol Infect Dis. 1996. 15:909–912.

20. Abi-Said D, Anaissie E, Uzun O, Raad I, Pinzcowski H, Vartivarian S. The epidemiology of hematogenous candidiasis caused by different Candida species. Clin Infect Dis. 1997. 24:1122–1128.

21. Pfaller MA, Diekema DJ. International Fungal Surveillance Participant Group. Twelve years of fluconazole in clinical practice: global trends in species distribution and fluconazole susceptibility of bloodstream isolates of Candida. Clin Microbiol Infect. 2004. 10:11–23.

22. Krcméry V Jr, Kovacicová G. Longitudinal 10-year prospective survey of fungaemia in Slovak Republic: trends in etiology in 310 episodes. Slovak Fungaemia study group. Diagn Microbiol Infect Dis. 2000. 36:7–11.
23. Takakura S, Fujihara N, Saito T, Kudo T, Iinuma Y, Ichiyama S. National surveillance of species distribution in blood isolates of Candida species in Japan and their susceptibility to six antifungal agents including voriconazole and micafungin. J Antimicrob Chemother. 2004. 53:283–289.

24. Collin B, Clancy CJ, Nguyen MH. Antifungal resistance in non-albicans Candida species. Drug Resist Update. 1999. 2:9–14.
25. Pfaller MA, Jones RN, Doern GV, Sader HS, Hollis RJ, Messer SA. International surveillance of bloodstream infections due to Candida species: frequency of occurrence and antifungal susceptibilities of isolates collected in 1997 in the United States, Canada, and South America for the SENTRY Program. The SENTRY Participant Group. J Clin Microbiol. 1998. 36:1886–1889.

26. Shin JH, Shin DH, Song JW, Kee SJ, Suh SP, Ryang DW. Electrophoretic karyotype analysis of sequential Candida parapsilosis isolates from patients with persistent or recurrent fungemia. J Clin Microbiol. 2001. 39:1258–1263.

27. Shin JH, Kee SJ, Shin MG, Kim SH, Shin DH, Lee SK, et al. Biofilm production by isolates of Candida species recovered from nonneutropenic patients: comparison of bloodstream isolates with isolates from other sources. J Clin Microbiol. 2002. 40:1244–1248.

28. Levin AS, Costa SF, Mussi NS, Basso M, Sinto SI, Machado C, et al. Candida parapsilosis fungemia associated with implantable and semi-implantable central venous catheters and the hands of healthcare workers. Diagn Microbiol Infect Dis. 1998. 30:243–249.

29. Pfaller MA, Jones RN, Messer SA, Edmond MB, Wenzel RP. National surveillance of nosocomial blood stream infection due to species of Candida other than Candida albicans: frequency of occurrence and antifungal susceptibility in the SCOPE Program. SCOPE Participant Group. Surveillance and Control of Pathogens of Epidemiologic. Diagn Microbiol Infect Dis. 1998. 30:121–129.

30. Pappas PG, Rex JH, Lee J, Hamill RJ, Larsen RA, Powderly W, et al. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and paediatric patients. Clin Infect Dis. 2003. 37:634–643.

31. Sanguinetti M, Posteraro B, Fiori B, Ranno S, Torelli R, Fadda G. Mechanisms of azole resistance in clinical isolates of Candida glabrata collected during a hospital survey of antifungal resistance. Antimicrob Agents Chemother. 2005. 49:668–679.

32. Hajjeh RA, Sofair AN, Harrison LH, Lyon GM, Arthington-Skaggs BA, Mirza SA, et al. Incidence of bloodstream infections due to Candida species and in vitro susceptibilities of isolates collected from 1998 to 2000 in a population-based active surveillance program. J Clin Microbiol. 2004. 42:1519–1527.

33. Pfaller MA, Messer SA, Hollis RJ, Jones RN, Diekema DJ. In vitro activities of ravuconazole and voriconazole compared with those of four approved systemic antifungal agents against 6,970 clinical isolates of Candida spp. Antimicrob Agents Chemother. 2002. 46:1723–1727.

34. Tortorano AM, Rigoni AL, Biraghi E, Prigitano A, Viviani MA; The FIMLIA-ECMM Candidaemia Study Group. The European Confederation of Medical Mycology (ECMM) survey of candidaemia in Italy: antifungal susceptibility patterns of 261 non-albicans Candida isolates from blood. J Antimicrob Chemother. 2003. 52:679–682.

35. Rex JH, Pfaller MA, Galgiani JN, Bartlett MS, Espinel-Ingroff A, Ghannoum MA, et al. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and Candida infections. Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. Clin Infect Dis. 1997. 24:235–247.

36. Rex JH, Rinaldi MG, Pfaller MA. Resistance of Candida species to fluconazole. Antimicrob Agents Chemother. 1995. 39:1–8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download