Abstract
Materials and Methods
From December 2005 to February 2006, a prospective, double-blind study was performed involving 90 patients who had undergone a total knee arthroplasty. Patients were randomly divided into three equal groups (n = 30). Demographic data, including age, height, weight, knee score, visual analogue scale (VAS), and range of flexion were evaluated preoperatively. Before wound closure, patients were given intra-synovial injections of the following solutions: patients in group I received 40 mL of 300 mg ropivacaine with 1 : 200,000 epinephrine and 5 mg morphine; patients in Group II received 40 mL of 300 mg ropivacaine with epinephrine; and patients in Group III received 50 mL normal saline as a control. All patients received an epidural patient-controlled analgesia (PCA) for 24 postoperative hours. Analgesic efficacy was evaluated using the VAS at intervals of 2, 4, 6, 12, 24, 32, 40, and 48 hours postoperatively. During this period, the side effects, the dosage of rescue analgesia required, and the range of knee flexion were recorded for each group.
Total knee arthroplasty is a major orthopaedic operation associated with considerable postoperative pain. Several analgesic techniques are used for pain management, including a peripheral nerve blockade, non-steroidal anti-inflammatory drugs, and narcotics administered orally, intramuscularly, intravenously, or via a patient-controlled analgesia (PCA) pump. Each of these therapies may be used alone or in combination.1 Gupta et al.2 found significant though minor pain reduction for up to 24 hours postoperatively after intra-articular administration of morphine. Intra-articular injection of bupivacaine and epinephrine decreased the need for narcotics and increased the range of motion after knee replacement.3 Kligman et al.4 reported that intra-synovial injection, as compared to intra-articular injection, provided better pain relief for patients who underwent an arthroscopic meniscectomy. To our knowledge, however, no attempts have been made to study the effects of intra-synovial injection of local anesthesia and morphine in patients following a total knee replacement.
We chose ropivacaine for local anesthesia because it showed a lower incidence of cardiotoxicity than bupivacaine.5 The aim of this study was to evaluate the analgesic efficacy of ropivacaine (alone or with morphine) injected into synovial tissue after a total knee arthroplasty.
From December 2005 to February 2006, a prospective study was conducted involving 90 patients (78 women, 12 men) who had undergone primary total knee arthroplasty. Prior to enrollment, all patients gave their informed written consent. Exclusion criteria included and age greater than 80 years, body weight over 100 kg, grade IV or higher in American Society of Anesthesiologist (ASA), alcohol or narcotics abuse, and patient hypersensitivity to morphine or local anesthesia. The LCS prosthesis (Depuy Int, Leeds, UK) was chosen for total knee arthroplasty except in 14 cases that had a severe deformity. In those cases, the NexGen prosthesis (Zimmer, Warsaw, IN, USA) was used for patients exhibiting flexion contracture over 30 degrees, or had varus or valgus deformity over 15 degrees. Patients were randomly divided into three equal groups (n = 30). Randomization was achieved by using a sequential pool based on a table of randomized numbers. Demographic characteristics were examined preoperatively and included criteria such as height, weight, gender, ASA, diagnosis, Hospital for Special Surgery (HSS) knee score, Knee Society Score (KSS) knee score, visual Analogue Scale (VAS) score, and range of flexion.
All patients received combined anesthesia. The spinal anesthesia was 8 to 10 mg of 0.5% isobaric tetracaine. The epidural infusion pump used 225 mg of 0.225% ropivacaine, 0.1 mg of sufentanyl, 0.005 mg/kg of naloxone, and 0.9% normal saline to make the 100 mL solution. The PCA device was designed to deliver a dose of 2 mL/hour, with an "on-demand" bolus of 0.5 mL every 15 minutes. Surgery was initiated when pinprick anesthesia was achieved at the T10 dermatomal level. A midline incision and parapatellar arthrotomy was made using standard surgical techniques. Following instrumented bone resection, total knee components were fixed. Soft tissue balancing and patellar tracking were assessed and corrected. Before closure of the wound, the following solutions were injected into 10 separate areas around the synovium: patients in Group I received 40 mL of 300 mg ropivacaine with 0.25 mL of 1 : 200,000 epinephrine, 0.5 mL of 5 mg morphine, and 9.25 mL of 0.9% normal saline; patients in Group II received 40 mL of 300 mg ropivacaine with 0.25 mL of 1 : 200,000 epinephrine, and 9.75 mL of 0.9% normal saline; and patients in Group III received 50 mL of 0.9% normal saline as a control. The intra-synovial medications were administered by the senior author, who was blind to the contents of the solution. After injection, a wound drain was placed near the medial aspect of the joint space. The tourniquet and drain clamp were released after the skin wound was sutured.
Postoperatively, residual sensory levels were checked hourly using the pinprick method. The spinal anesthesia sensory blockade on the knee disappeared completely within two hours of the surgery in all patients. Perioperative management included standard antibiotic prophylaxis, a PCA pump, and rescue analgesia. The incidence of booster PCA was recorded for 24 hours before removal of the PCA device. The amount of intravenously injected tramadol (used for rescue analgesia) was recorded. Analgesic efficacy was evaluated by noting the VAS at 2, 4, 6, and 12 hours postoperatively at a resting state, and at 24, 32, 40, and 48 hours postoperatively at resting and exercising states. During this period, side effects and the range of flexion were recorded for each group. The patients and investigators who participated in the postoperative assessment were masked to the patients' group assignments and treatments. Weight bearing and ambulation were started within 24 hours postoperatively.
The differences among the three groups were analyzed using a Fisher's exact test, Pearson chi-square test and one-way analysis of variance (ANOVA). If a significant difference was found, the Tukey's HSD test was used to detect the differences among the groups. The differences were considered to be significant if p < 0.05. The SPSS 13.0 ps.exe statistical program was used for the analysis (SPSS Inc, Chicago, IL, USA).
Demographic characteristics were similar among the three groups. However, there was a significantly higher preoperative HSS knee score in Group III as compared to Group II (p = 0.034) (Table 1).
In resting status (at 2, 4, 6, 12, 24, 32, 40 and 48 hours postoperatively), there were no significant differences in the VAS between three groups (p > 0.05) (Table 2). In exercising status (at 24, 32, 40 and 48 hours postoperatively), there were also no significant differences in the VAS (p > 0.05) (Table 3).
The mean dosages (± standard deviation) of tramadol used as rescue analgesia on the day of the operation were as follows: 30 ± 40 mg in Group I, 30 ± 30 mg in Group II, and 40 ± 60 mg in Group III (p = 0.607). The dosages on the first postoperative day prior to epidural PCA removal were 25 ± 40 mg in Group I, 40 ± 45 mg in Group II, and 40 ± 55 mg in Group III (p = 0.285). The dosages on the first postoperative day after epidural PCA removal were 25 ± 30 mg in Group I, 35 ± 40 mg in Group II, and 30 ± 30 mg in Group III (p = 0.522). The dosages on the second postoperative day were 30 ± 45 mg in Group I, 20 ± 40 mg in Group II, and 25 ± 50 mg in Group III (p = 0.522). There were no significant differences in the tramadol dosage among the groups beyond post-op day two.
The mean incidence (± standard deviation) of booster PCA use before epidural catheter removal was 29.7 ± 10.6 in Group I, 32.7 ± 11.0 in Group II, and 33.8 ± 7.4 in Group III. There was no significant difference among thee groups (p = 0.249).
Regarding the side effects, 14 patients in Group I, 12 patients in Group II, and 12 patients in Group III experienced nausea within 48 hours of the surgery. There was no significant difference in the incidence of nausea among the three groups (p = 0.833). The mean incidence of emesis within 48 hours of the surgery was 0.7 for Group I, 0.4 for Group II, and 0.3 for Group III. There was no significant difference in incidence of emesis among the three groups (p = 0.270). Complications such as hematoma, infection, or perioperative fracture were not present in any of the cases.
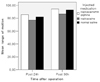
The mean range of flexion (± standard deviation) at 24 hours postoperatively was 85.7 ± 29.7 degrees in Group I, 77.0 ± 39.6 in Group II, and 82.0 ± 23.7 in Group III (p = 0.569). At 36 hours postoperatively, the mean range of flexion was 94.3 ± 28.6 degrees in Group I, 86.5 ± 36.2 degrees in Group II, and 93.0 ± 24.8 degrees in Group III (p = 0.564) (Fig. 1). There were no significant differences among three groups.
An epidural PCA is not always appropriate following a major operation despite its strong analgesic effects, especially in patients who have had previous surgery in the lumbar area, are severely obese, or have a concurrent bleeding diathesis.6-9 Intra-articular injection of medication such as morphine or local anesthesia for postoperative pain control is commonly studied in the setting of arthroscopic surgeries.10-12 Recently, pain management that included intra-articular injection after a major surgery has been studied, despite some studies demonstrating an analgesic effect akin to that of placebo.13-17
Ropivacaine and morphine were used as analgesics in this study. Ropivacaine (1-propyl-2', 6'-pipecoloxylidide hydrochloride) is a new, long acting, local anesthetic. Although chemically related to bupivacaine, studies have shown ropivacaine to produce less cardiac and central nervous system toxicity than bupivacaine. It also produces a similar degree of sensory block, but with less motor block than bupivacaine.18
Intra-articular local anesthesia, combined with morphine and ketorolac, has been found to have a synergistic effect on pain relief following arthroscopic procedures.11 When the morphine is administrated into local inflammatory tissue such as a joint, it produces analgesia by acting on local opioid receptors in the inflammatory tissue, thus inhibiting the transmission of nociceptive signals out of the local tissue.19-21 A small dose of naloxone added to an epidural PCA does not affect the opioid receptors around the knee.22 However, in this study, ropivacaine with morphine did not show any analgesic advantage over placebo (p > 0.05). Even though there was a short time interval between the intra-synovial injection and tourniquet release, the interval was sufficient enough to achieve the analgesic effect.23 The mean onset of motor and sensory blockade by ropivacaine was within six minutes of administration.24
Intra-synovial injection was used in this study because it was more effective than intra-articular injection for analgesia. To our knowledge, no prospective double-blind study has been conducted involving intra-synovial ropivacaine (either alone or with morphine) injection for pain relief after total knee arthroplasty. There was a similar study by Busch et al.25 on periarticular multimodal injections including ropivacaine, ketorolac, epimorphine and epinephrine which showed less requirement for rescue analgesics than placebo.
There are several limitations to this study. First, there is the possibility that the analgesic effect of the intra-synovial injection of ropivacaine was masked by the epidural PCA during the first 24 hours. Thus, it would be useful to study the pure effect of ropivacaine injected intra-synovially, without the presence of an epidural PCA. That said, our goal was to determine if these was any additional benefit of ropivacaine injected intra-synovially combined with an epidural PCA, and we found none. Second, there is no available data regarding the appropriate dosage of ropivacaine in major surgeries (such as a knee replacement); there is only data for minor surgeries, such as tonsillectomies or menisectomies. In this study, 300 mg of ropivacaine was used to manage the pain after arthroscopic knee surgery.10
In conclusion, ropivacaine, alone or with morphine injected intra-synovially added to an epidural PCA has no additional benefits in regard to analgesic efficacy, rescue analgesics, the incidence of side effects, or the range of flexion after total knee arthroplasty.
Figures and Tables
Fig. 1
Knee range of flexion (degree), 24 and 36 hours postoperatively. Statistical analysis was done using a one-way ANOVA.
References
1. Botte MJ, Gellman H, Meyer RS, Tafolla SE, Hoenecke HR Jr, Brage ME, et al. Local and regional anesthesia for the management of pain in orthopaedic surgery. Instr Course Lect. 2000. 49:523–540.
2. Gupta A, Bodin L, Holmstrom B, Berggren L. A systemic review of the peripheral analgesic effects of intraarticular morphine. Anesth Analg. 2001. 93:761–770.
3. Badner NH, Bourne RB, Rorabeck CH, MacDonald SJ, Doyle JA. Intra-articular injection of bupivacaine in knee-replacement operations. Results of use for analgesia and for preemptive blockade. J Bone Joint Surg Am. 1996. 78:734–738.
4. Kligman M, Bruskin A, Sckliamser J, Vered R, Roffman M. Intra-synovial, compared to intra-articular morphine provides better pain relief following knee arthroscopy menisectomy. Can J Anaesth. 2002. 49:380–383.
5. Graf BM, Abraham I, Eberbach N, Kunst G, Stowe DF, Martin E. Differences in cardiotoxicity of bupivacaine and ropivacaine are the result of physiochemical and stereoselective properties. Anesthesiology. 2002. 96:1427–1434.
6. DeWeese FT, Akbari Z, Carline E. Pain control after knee arthroplasty: intraarticular versus epidural anesthesia. Clin Orthop. 2001. 392:226–231.
7. Singelyn FJ, Deyaert M, Joris D, Pendeville E, Gouverneur JM. Effects of intravenous patient-controlled analgesia with morphine, continuous epidural analgesia, and continuous three-in-one block on postoperative pain and knee rehabilitation after unilateral total knee arthroplasty. Anesth Analg. 1998. 87:88–92.
8. Horlocker TT, Hebl JR, Kinney MA, Cabanela ME. Opioid-free analgesia following total knee arthroplasty-a multimodal approach using continuous lumbar plexus (psoas compartment) block, acetaminophen, and ketorolac. Reg Anesth Pain Med. 2002. 27:105–108.
9. Capdevila X, Barthelet Y, Biboulet P, Ryckwaert Y, Rubenovitch J, d'Athis F. Effects of perioperative analgesic technique on the surgical outcome and duration of rehabilitation after major knee surgery. Anesthesiology. 1999. 91:8–15.
10. Ng HP, Nordstrom U, Axelsson K, Peniola AD, Gustav E, Ryttberg L, et al. Efficacy of intra-articular bupivacaine, ropivacaine, or a combination of ropivacaine, morphine, and ketorolac on postoperative pain relief after ambulatory arthroscopic knee surgery: a randomized double-blind study. Reg Anesth Pain Med. 2006. 31:26–33.
11. Gupta A, Axelsson K, Allvin R, Liszka-Hackzell J, Rawal N, Althoff B, et al. Postoperative pain following knee arthroscopy: the effects of intra-articular ketorolac and/ or morphine. Reg Anesth Pain Med. 1999. 24:225–230.
12. Stein C, Comisel K, Haimerl E, Yassouridis A, Lehrberger K, Herz A, et al. Analgesic effect of intraarticular morphine after arthroscopic knee surgery. N Engl J Med. 1991. 325:1123–1126.
13. Ritter MA, Koehler M, Keating EM, Faris PM, Meding JB. Intra-articular morphine and/or bupivacaine after total knee replacement. J Bone Joint Surg Br. 1999. 81:301–303.
14. Hoenecke HR Jr, Pulido PA, Morris BA, Fronek J. The efficacy of continuous bupivacaine infiltration following anterior cruciate ligament reconstruction. Arthroscopy. 2002. 18:854–858.
15. Tanaka N, Sakahashi H, Sato E, Hirose K, Ishii S. The efficacy of intra-articular analgesia after total knee arthroplasty in patients with rheumatoid arthritis and in patients with osteoarthritis. J Arthroplasty. 2001. 16:306–311.
16. Mauerhan DR, Campbell M, Miller JS, Mokris JG, Gregory A, Kiebzak GM. Intra-articular morphine and/or bupivacaine in the management of pain after total knee arthroplasty. J Arthroplasty. 1997. 12:546–552.
17. Lombardi AV Jr, Berend KR, Mallory TH, Dodds KL, Adams JB. Soft tissue and intra-articular injection of bupivacaine, epinephrine, and morphine has a beneficial effect after total knee arthroplasty. Clin Orthop. 2004. 428:125–130.
18. Bader AM, Datta S, Flanagan H, Covino BG. Comparison of bupivacaine- and ropivacaine-induced conduction blockade in the isolated rabbit vagus nerve. Anesth Analg. 1989. 68:724–727.
19. Stein C, Hassan AH, Lehrberger K, Giefing J, Yassouridis A. Local analgesic effect of endogenous opioid peptides. Lancet. 1993. 342:321–324.
20. Stein C, Hassan AH, Przewlocki R, Gramsch C, Peter K, Herz A. Opioids from immunocytes interact with receptors on sensory nerves to inhibit nociception in inflammation. Proc Natl Acad Sci U S A. 1990. 87:5935–5939.
21. Bartho L, Stein C, Herz A. Involvement of capsaicin-sensitive neurones in hyperalgesia and enhanced opioid antinociception in inflammation. Naunyn Schmiedebergs Arch Pharmacol. 1990. 342:666–670.
22. Choi JH, Lee J, Choi JH, Bishop MJ. Epidural naloxone reduced pruritus and nausea without affecting analgesia by epidural morphine in bupivacaine. Can J Anesth. 2000. 47:33–37.
23. Whitford A, Healy M, Joshi GP, McCarroll SM, O'Brien TM. The effect of tourniquet release time on the analgesic efficacy of intraarticular morphine after arthroscopic knee surgery. Anesth Analg. 1997. 84:791–793.
24. Klein SM, Greengrass RA, Steele SM, D'Ercole FJ, Speer KP, Gleason DH, et al. A comparison of 0.5% bupivacaine, 0.5% ropivacaine, and 0.75% ropivacaine for interscalene brachial plexus block. Anesth Analg. 1998. 87:1316–1319.
25. Busch CA, Shore BJ, Bhandari R, Ganapathy S, MacDonald SJ, Bourne RB, et al. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006. 88:959–963.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download