1. Lee G, Attar K, Laniado M, Karim O. Trans-rectal ultrasound guided biopsy of the prostate: nationwide diversity in practice and training in the United Kingdom. Int Urol Nephrol. 2007; 39:185–188. PMID:
17268896.

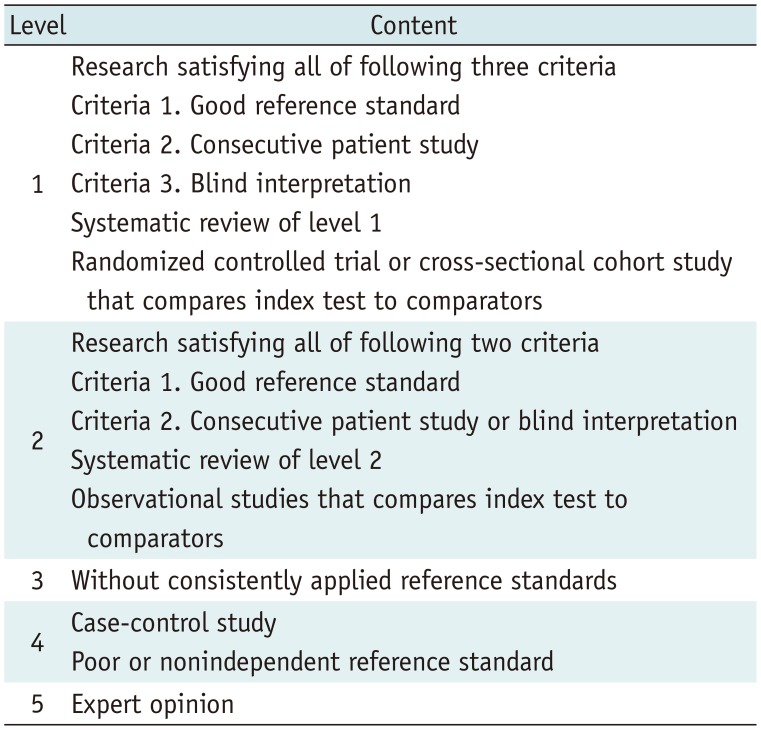
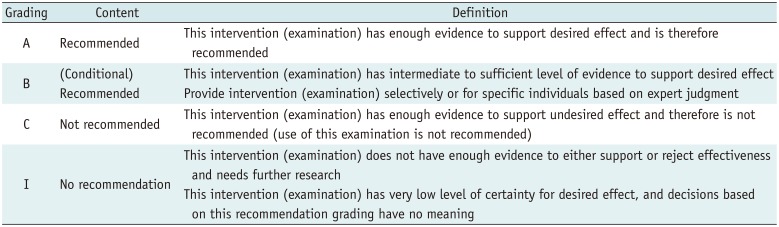
2. Choi SJ, Jeong WK, Jo AJ, Choi JA, Kim MJ, Lee M, et al. Methodology for developing evidence-based clinical imaging guidelines: joint recommendations by Korean Society of Radiology and National Evidence-based Healthcare Collaborating Agency. Korean J Radiol. 2017; 18:208–216. PMID:
28096730.

3. Kim JH, Baek JH, Lim HK, Ahn HS, Baek SM, Choi YJ, et al. Guideline Committee for the Korean Society of Thyroid Radiology (KSThR) and Korean Society of Radiology. 2017 Thyroid Radiofrequency Ablation guideline: Korean Society of Thyroid Radiology. Korean J Radiol. 2018; 19:632–665. PMID:
29962870.

4. Kang MJ, Kim JH, Kim YK, Lee HJ, Shin KM, Kim JI, et al. 2018 Korean clinical imaging guideline for hemoptysis. Korean J Radiol. 2018; 19:866–871. PMID:
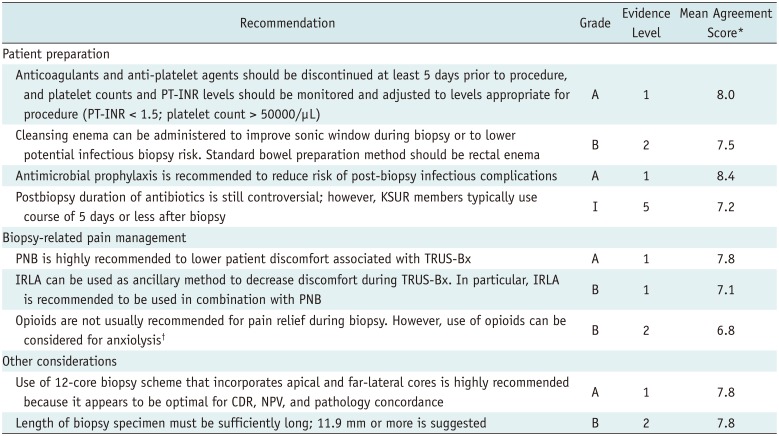
30174475.

5. Loeb S, Vellekoop A, Ahmed HU, Catto J, Emberton M, Nam R, et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013; 64:876–892. PMID:
23787356.

6. El-Hakim A, Moussa S. CUA guidelines on prostate biopsy methodology. Can Urol Assoc J. 2010; 4:89–94. PMID:
20368888.

7. Jaffe TA, Raiff D, Ho LM, Kim CY. Management of anticoagulant and antiplatelet medications in adults undergoing percutaneous interventions. AJR Am J Roentgenol. 2015; 205:421–428. PMID:
26204296.
8. Patel IJ, Davidson JC, Nikolic B, Salazar GM, Schwartzberg MS, Walker TG, et al. Standards of Practice Committee, with Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Endorsement. Consensus guidelines for periprocedural management of coagulation status and hemostasis risk in percutaneous image-guided interventions. J Vasc Interv Radiol. 2012; 23:727–736. PMID:
22513394.

9. Maan Z, Cutting CW, Patel U, Kerry S, Pietrzak P, Perry MJ, et al. Morbidity of transrectal ultrasonography-guided prostate biopsies in patients after the continued use of low-dose aspirin. BJU Int. 2003; 91:798–800. PMID:
12780835.

10. Herget EJ, Saliken JC, Donnelly BJ, Gray RR, Wiseman D, Brunet G. Transrectal ultrasound-guided biopsy of the prostate: relation between ASA use and bleeding complications. Can Assoc Radiol J. 1999; 50:173–176. PMID:
10405650.
11. Ihezue CU, Smart J, Dewbury KC, Mehta R, Burgess L. Biopsy of the prostate guided by transrectal ultrasound: relation between warfarin use and incidence of bleeding complications. Clin Radiol. 2005; 60:459–463. PMID:
15767103.

12. Giannarini G, Mogorovich A, Valent F, Morelli G, De Maria M, Manassero F, et al. Continuing or discontinuing low-dose aspirin before transrectal prostate biopsy: results of a prospective randomized trial. Urology. 2007; 70:501–505. PMID:
17688919.

13. Lindert KA, Kabalin JN, Terris MK. Bacteremia and bacteriuria after transrectal ultrasound guided prostate biopsy. J Urol. 2000; 164:76–80. PMID:
10840428.

14. Carey JM, Korman HJ. Transrectal ultrasound guided biopsy of the prostate. Do enemas decrease clinically significant complications? J Urol. 2001; 166:82–85. PMID:
11435829.

15. Jeon SS, Woo SH, Hyun JH, Choi HY, Chai SE. Bisacodyl rectal preparation can decrease infectious complications of transrectal ultrasound-guided prostate biopsy. Urology. 2003; 62:461–466. PMID:
12946747.

16. Park DS, Oh JJ, Lee JH, Jang WK, Hong YK, Hong SK. Simple use of the suppository type povidone-iodine can prevent infectious complications in transrectal ultrasound-guided prostate biopsy. Adv Urol. 2009; 750598. PMID:
19404480.

17. Kam SC, Choi SM, Yoon S, Choi JH, Lee SH, Hwa JS, et al. Complications of transrectal ultrasound-guided prostate biopsy: impact of prebiopsy enema. Korean J Urol. 2014; 55:732–736. PMID:
25405015.

18. De Nunzio C, Lombardo R, Presicce F, Bellangino M, Finazzi Agro E, Gambrosier MB, et al. Transrectal-ultrasound prostatic biopsy preparation: rectal enema vs. mechanical bowel preparation. Cent European J Urol. 2015; 68:223–228.
19. Zani EL, Clark OA, Rodrigues Netto. Antibiotic prophylaxis for transrectal prostate biopsy. Cochrane Database Syst Rev. 2011; (5):CD006576. PMID:
21563156.

20. Yang M, Zhao X, Wu Z, Xiao N, Lu C. Meta-analysis of antibiotic prophylaxis use in transrectal prostatic biopsy. Zhong Nan Da Xue Xue Bao Yi Xue Ban. 2009; 34:115–123. PMID:
19270350.
21. Schaeffer AJ, Montorsi F, Scattoni V, Perroncel R, Song J, Haverstock DC, et al. Comparison of a 3-day with a 1-day regimen of an extended-release formulation of ciprofloxacin as antimicrobial prophylaxis for patients undergoing transrectal needle biopsy of the prostate. BJU Int. 2007; 100:51–57. PMID:
17552953.

22. Briffaux R, Merlet B, Normand G, Coloby P, Leremboure H, Bruyère F, et al. [Short or long schemes of antibiotic prophylaxis for prostate biopsy. A multicentre prospective randomised study]. Prog Urol. 2009; 19:39–46. PMID:
19135641.
23. Jung SI. Infection in patients undergoing transrectal ultrasound guided prostate biopsy. Korean J Urogenit Tract Infect Inflamm. 2013; 8:20–26.

24. Nash PA, Bruce JE, Indudhara R, Shinohara K. Transrectal ultrasound guided prostatic nerve blockade eases systematic needle biopsy of the prostate. J Urol. 1996; 155:607–609. PMID:
8558671.

25. Tiong HY, Liew LC, Samuel M, Consigliere D, Esuvaranathan K. A meta-analysis of local anesthesia for transrectal ultrasound-guided biopsy of the prostate. Prostate Cancer Prostatic Dis. 2007; 10:127–136. PMID:
17211441.

26. Hergan L, Kashefi C, Parsons JK. Local anesthetic reduces pain associated with transrectal ultrasound-guided prostate biopsy: a meta-analysis. Urology. 2007; 69:520–525. PMID:
17382157.

27. Maccagnano C, Scattoni V, Roscigno M, Raber M, Angiolilli D, Montorsi F, et al. Anaesthesia in transrectal prostate biopsy: which is the most effective technique? Urol Int. 2011; 87:1–13. PMID:
21677420.

28. Lee C, Woo HH. Current methods of analgesia for transrectal ultrasonography (TRUS)-guided prostate biopsy -- a systematic review. BJU Int. 2014; 113:48–56. PMID:
24053451.

29. Izol V, Soyupak B, Seydaoglu G, Aridogan IA, Tansug Z. Three different techniques for administering analgesia during transrectal ultrasound-guided prostate biopsy: a comparative study. Int Braz J Urol. 2012; 38:122–128. PMID:
22397774.

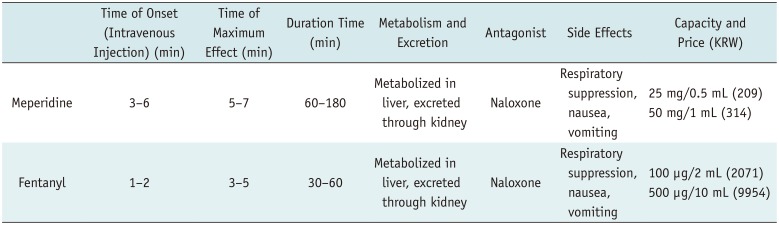
30. Moudouni S, Amine M, Lakmichi A, Dahami Z, Sarf I. UP-02.137. A randomized, controlled trial comparing lidocaine periprostatic nerve block and lidocaine gel intrarectally associated with tramadol per os for transrectal ultrasound guided biopsy of prostate. Urology. 2011; 78:S307.

32. McCormack M, Duclos A, Latour M, McCormack MH, Liberman D, Djahangirian O, et al. Effect of needle size on cancer detection, pain, bleeding and infection in TRUS-guided prostate biopsies: a prospective trial. Can Urol Assoc J. 2012; 6:97–101. PMID:
22511415.

33. Öbek C, Doğanca T, Erdal S, Erdoğan S, Durak H. Core length in prostate biopsy: size matters. J Urol. 2012; 187:2051–2055. PMID:
22498214.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download