Abstract
Objective
To compare the T1-weighted spectral presaturation with inversion-recovery sequences (T1 SPIR) with T2-weighted turbo spin-echo sequences (T2 TSE) on 3T magnetic resonance arthrography (MRA) in the evaluation of the subscapularis (SSC) tendon tear with arthroscopic findings as the reference standard.
Materials and Methods
This retrospective study included 120 consecutive patients who had undergone MRA within 3 months between April and December 2015. Two musculoskeletal radiologists blinded to the arthroscopic results evaluated T1 SPIR and T2 TSE images in separate sessions for the integrity of the SSC tendon, examining normal/articular-surface partial-thickness tear (PTTa)/full-thickness tear (FTT). Diagnostic performance of T1 SPIR and T2 TSE was calculated with arthroscopic results as the reference standard, and sensitivity, specificity, and accuracy were compared using the McNemar test. Interobserver agreement was measured with kappa (κ) statistics.
Results
There were 74 SSC tendon tears (36 PTTa and 38 FTT) confirmed by arthroscopy. Significant differences were found in the sensitivity and accuracy between T1 SPIR and T2 TSE using the McNemar test, with respective rates of 95.9–94.6% vs. 71.6–75.7% and 90.8–91.7% vs. 79.2–83.3% for detecting tear; 55.3% vs. 31.6–34.2% and 85.8% vs. 78.3–79.2%, respectively, for FTT; and 91.7–97.2% vs. 58.3–61.1% and 89% vs. 78–79.3%, respectively, for PTTa. Interobserver agreement for T1 SPIR was almost perfect for T1 SPIR (κ = 0.839) and substantial for T2 TSE (κ = 0.769).
The subscapularis (SSC) is the largest of the rotator cuff muscles. It is important in passive and active stabilization of the glenohumeral joint (123). Isolated SSC tendon tears are very rare and most occur in the setting of chronic supraspinatus tendon tears (4567). Early studies of rotator cuff tendon tears focused on the supraspinatus tendon. However, SCC tendon tears have garnered increasing attention over the last decade or so.
The transverse force couple formed by the SSC muscle and the posteriorly located infraspinatus/teres minor muscles is important in maintaining the normal function of the shoulder (8). An underdiagnosed SSC tendon tear results in an unbalanced transverse force couple, which may lead to persistent pain and weakness, and a suboptimal surgical outcome after the repair of coexisting supraspinatus or infraspinatus tears (9101112). However, SSC tendon tears can be difficult to diagnose solely on physical examination, and lesions may be overlooked on arthroscopy as the humeral head can hinder the visualization of SSC tendon footprint (1314). Therefore, imaging studies, in particular magnetic resonance imaging (MRI), may play an important role in the accurate preoperative assessment of the SSC tendon.
The use of magnetic resonance arthrography (MRA) in evaluating rotator cuff tears is controversial, since it is invasive and carries the potential of complications. However, studies have suggested an improved diagnostic accuracy with MRA compared with MRI in assessing rotator cuff tendon tears (15). Moreover, a recent meta-analysis comparing the diagnostic value of 3-tesla (3T) MRI and 3T MRA in diagnosing rotator cuff tendons reported a trend toward improved diagnostic accuracy with MRA compared to MRI in the diagnosis of SSC tendon tears (16). The data support the use of MRA in the evaluation of SSC tendon tears.
The accuracy of preoperative MRA in detecting SSC tendon tears has been investigated (1017). MRA has been reported to have an overall accuracy of 84–88% in diagnosing SSC tendon tears (17) but only a 36% preoperative sensitivity in detecting arthroscopically proven SSC tears (10). These controversial results may have resulted from many factors, including the size and location of the tear being evaluated, different imaging protocols, and level of experience of the radiologists evaluating the magnetic resonance (MR) images.
Based on our clinical experience, we hypothesized that, among many factors, the imaging sequences used in MRA may have an important influence on the diagnosis of SSC tendon tears. Therefore, the purpose of our study was to compare the diagnostic performance of T1-weighted spectral presaturation with inversion-recovery sequences (T1 SPIR) and T2-weighted turbo spin-echo sequences (T2 TSE) on 3T direct MRA in the preoperative evaluation of SSC tendon tears with arthroscopic findings as the reference standard.
This retrospective study was approved by our Institutional Review Board. Informed consent was waived.
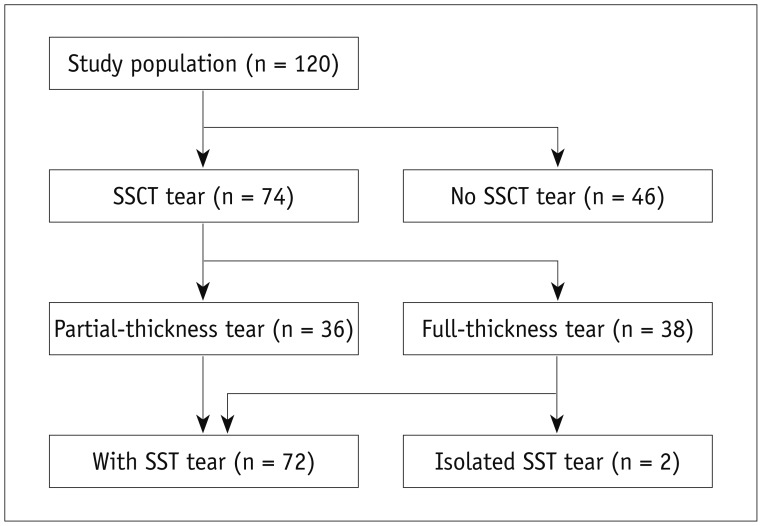
Among 223 consecutive 3T MRA examinations of the shoulder performed at our institution between April and December 2015, patients with a subsequent arthroscopic surgery performed at our institution within 3 months of the MRA and a clear record of the arthroscopic findings regarding the presence and degree of the SSC tendon tear were enrolled retrospectively. There were 94 patients who had not performed subsequent arthroscopy within 3 months and 7 patients without detailed arthroscopic results of SSC tendon. Two other patients were excluded because they had previously undergone shoulder surgery (n = 1) and was younger than 16 years of age (n = 1). A total of 120 patients were included in the study (mean age, 62.7 years; age range, 36–81 years; 50 men and 70 women). The mean interval between MRI and arthroscopic surgery was 31 days (range, 1–84 days).
All MRA examinations were performed with an Achieva or Ingenia 3-T MRI scanner (Philips Healthcare, Best, the Netherlands) using a dedicated shoulder coil. Prior to MR acquisition, intra-articular contrast administration was performed under fluoroscopic guidance. A 22-gauge spinal needle was placed into the glenohumeral joint with an anterior approach and 1–2 mL of iodinated contrast medium was injected to confirm the intra-articular location of the needle. Approximately 10–12 mL of a dilute solution of gadolinium-based contrast agent (Gadovist; Bayer Schering Pharma, Berlin, Germany) with a concentration of 2.5 mmol/L was injected. MR imaging of the shoulder was initiated within 30 minutes post-injection. T1 SPIR images were obtained in the axial, oblique coronal (perpendicular to the glenoid or parallel to the long axis of the supraspinatus tendon), and oblique sagittal (parallel to the glenoid or perpendicular to the long axis of the supraspinatus tendon) planes. T2 TSE images were also acquired in axial, oblique coronal, and oblique sagittal planes. The detailed parameters of all sequences are summarized in Table 1.
Magnetic resonance arthrography images were analyzed retrospectively and independently by two observers (with 25 and 5 years of experience in musculoskeletal radiology, respectively) who were blinded to the radiologic reports and arthroscopic results. Both readers evaluated the T1 SPIR and T2 TSE in two separate sessions, which were longer than 3 weeks apart to minimize recall bias. The MR images were anonymized and viewed in random order in each session on an Infinitt Picture Archiving and Communication System Workstation (Infinitt Healthcare, Seoul, Korea).
The MRA images were evaluated for the integrity of the SSC tendon on axial and oblique sagittal planes, and were classified as normal tendon, articular-surface partial-thickness tear (PTTa), or full-thickness tear (FTT). Normal tendon was defined as an intact tendon without leakage of contrast medium onto the lesser tuberosity of the humerus or within the tendon. PTTa was defined as a partial detachment from the lesser tuberosity or defect of the articular-surface of the tendon showing contrast leakage onto the lesser tuberosity with or without intratendinous extension on one or more images with a preserved continuity of the remaining bursal-surface of the tendon (Fig. 1). FTT was defined as a disruption of continuity of the tendon replaced by contrast filling from the bursal to the articular surfaces on one or more images (Fig. 2). Concealed interstitial tears and bursal-surface tears were not analyzed in this study due to the inaccessibility of these types of lesions during arthroscopy, which is gold standard for diagnosing rotator cuff tears.
All arthroscopic examinations were performed within 3 months after the MRA by a single orthopedic surgeon with 16 years of experience in shoulder surgery. During arthroscopy, all included patients underwent repair of the torn supraspinatus and/or SSC tendons. The presence and grade of the SSC tendon tear (PTTa or FTT) were recorded based on the arthroscopic findings, and served as the reference standard. The diagnosis of PTTa tear was made when the tendon was partially detached from the lesser tuberosity or torn horizontally with or without split on the intra-articular view through posterior portal. The bursal-surface partial-thickness tear were not recorded on the arthroscopic report because the bursal-surface of the tendon were not routinely evaluated during arthroscopy. FTT was diagnosed when the tendon tear extended completely across the intra-articular visible tendon or detached completely from the lesser tuberosity.
The sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and accuracy of T1 SPIR and T2 TSE were calculated for the presence of SSC tendon tear regardless of tear grade, FTT, and PTTa by both readers. In the analysis for the PTTa, diagnostic performance was calculated relative to the diagnosis of no tear with exclusion of patients with FTT confirmed arthroscopically (1819). The sensitivity, specificity, and accuracy of T1 SPIR and T2 TSE were compared using the McNemar's test. A p value < 0.05 was considered statistically significant.
Interobserver agreement between two readers for the grading of SSC tears was measured with the kappa (κ) statistics. The strength of agreement were interpreted according to the classification proposed by Landis and Koch (2021): poor (κ = 0), slight (κ = 0.0–0.2), fair (κ = 0.21–0.40), moderate (κ = 0.41–0.60), substantial (κ = 0.61–0.80), and almost perfect (κ = 0.81–1.00). All statistical analyses were performed using software (SPSS Statistics, version 18.0; SPSS Inc., Chicago, IL, USA).
Among the 120 patients, arthroscopy revealed a tear in the SSC tendon in 74 patients (61.7%). The 74 SSC tendon tears comprised 38 FTT and 36 PTTa. Among the 74 patients, only two had an isolated SSC lesion, whereas 72 (97.3%) had an accompanying supraspinatus tendon tear. Of these 72 tears, 65 were FTT (Fig. 3).
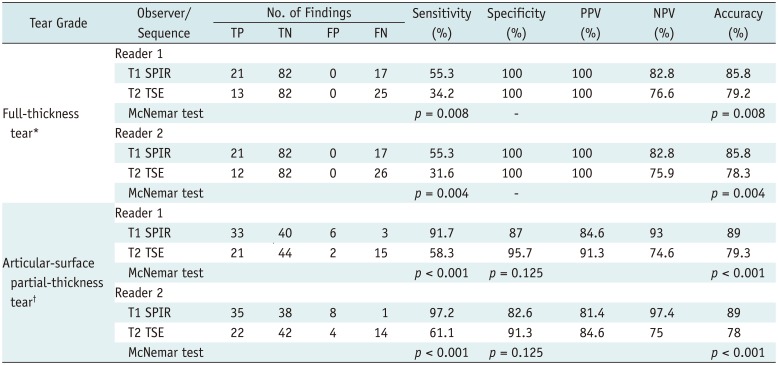
The sensitivity, specificity, PPV, NPV, and accuracy of T1 SPIR and T2 TSE for diagnosing the presence of SSC tendon tear regardless of tear grade are summarized in Table 2. T1 SPIR was more sensitive in detecting SSC tendon tears compared to T2 TSE. There were statistically significant differences in the sensitivity and accuracy between T1 SPIR and T2 TSE (p < 0.001 for both reader 1 and reader 2). The diagnostic performances of T1 SPIR and T2 TSE for diagnosing FTT and PTTa are presented in Table 3. T1 SPIR also showed superior diagnostic sensitivity and accuracy with statistical significance for both FTT and PTTa. Among the 36 PTTa, more than 30% were missed on T2 TSE by readers (33% for reader 1, 36.1% for reader 2). These missed tears were correctly diagnosed on T1 SPIR (Fig. 4).
On T1 SPIR, FTT of the SSC tendon was underdiagnosed as PTTa in 15 patients (88.2%) among the false-negative cases for reader 1 (n = 17), and in 16 (94.1%) patients for reader 2 (n = 17) (Fig. 5). On T2 TSE, FTT of the SSC tendon was underdiagnosed as PTTa in 22 patients (88%) among the false-negative cases for reader 1 (n = 25), and in 19 (73.1%) patients for reader 2 (n = 26). Interobserver agreement for T1 SPIR was almost perfect for T1 SPIR (κ = 0.839) and substantial for T2 TSE (κ = 0.769).
The results show that T1 SPIR is better than T2 TSE in the detection of the SSC tendon tears as well as in the grading tears.
Subscapularis tendon tears were found in 61.7% (74/120) of the patients undergoing arthroscopy for rotator cuff repair. This is a slightly higher prevalence compared to those reported in previous published literature (10–58.8%) (111722232425262728). The prevalence of SSC tendon tears has been reported in a variety of ranges depending on the included patients of the studies. Barth et al. (23) reported a SSC tear prevalence of 29.4% (20/68) among the all prospectively included patients scheduled for an arthroscopic procedure during a 3-month period. In this series, it was increased by 58.8% (20/34) when limited to patients with rotator cuff tendon repair, which was similar to our result. The chronicity and severity of supraspinatus tendon tear affects the incidence of SSC tendon abnormality (528). In the recent study by Yoo et al. (28), 50.5% (415/821) of the patients undergoing shoulder arthroscopy were diagnosed as SSC tendon tear, and the percentage of medium or large size FTT of tendons other than SSC was higher in the SSC tendon tear group compared to SSC tendon intact group. This may account for the results of our study, as the patients were those undergoing arthroscopy for rotator cuff tendon repair with a large percentage of full-thickness supraspinatus tendon tear.
The overall diagnostic performance of T1 SPIR for detecting SSC tendon abnormalities in our study was similar or more superior to that of the MRA-based study of Pfirrmann et al. (17), which demonstrated a sensitivity of 91%, specificity ranging between 79% and 86%, and accuracy ranging between 84% and 88% with combination of parasagittal T1-weighted turbo spin-echo sequence and transverse three-dimensional gradient-echo fast imaging sequence with steady-state precession. The higher strength of magnetic field of MR scanners might explain the slightly higher sensitivity in our study. In the study of Choo et al. (21), the sensitivity and specificity of the SSC tendon tear, regardless of grades of the tear, were 90–95% and 57–71%, respectively, with two-dimensional (2D) FSE sequences, which is also similar to our results.
T1-weighted spectral presaturation with inversion-recovery sequences showed superior diagnostic sensitivity and accuracy for detecting SSC tendon tears, regardless of the grade of tear, compared to T2 TSE with statistical significance on 3T MRA. This difference was more pronounced for PTTa (91.7–97.2% vs. 58.3–61.1%), compared to that for FTT (55.3% vs. 31.6–34.2%). We speculate that T2 TSE without fat-suppression used in our study has a minimal arthrographic effect, and the diagnostic performance may be similar to conventional MRI. In addition, the lower sensitivity on T2 TSE appears to be related to lower contrast resolution of T2 pulse sequence. Magee (29) suggested that 3T MRA is statistically more sensitive than conventional 3T MRI in detecting partial-thickness articular-surface supraspinatus tears (97% vs. 68%). As most partial thickness SSC tendon tears are found at the articular-surface (6), T1 SPIR of MRA may further improve the diagnosis of SSC tendon tears compared to conventional MRI.
The majority of the false-negative cases for diagnosing FTT of SSC tendon on T1 SPIR that contributed to low sensitivity were underdiagnosed as PTTa. This results disagree with Choo et al. (21), who reported more superior sensitivity for FTT (100%) compared to that for partial-thickness tears (82–88%) using 2D sequences of 3T MRA. However, the total sample size and number of full-thickness SSC tendon tears (n = 4) were relatively small in the prior study. The anatomical characteristics of the SSC tendon footprint may also account for the low sensitivity. Most of the tendinous portion of SSC attaches on the lesser tuberosity, but most superior and superficial fibers are continuous with fibers overlying the bicipital groove. These fibers contribute to the rotator interval capsule and biceps pulley, and interdigitate with anterior most fibers of the supraspinatus tendon (42230). Even when the tendinous fibers of SSC completely detach from the lesser tuberosity, the superficial “bridging fibers” may remain intact, preventing the torn SSC tendon from being retracted (Fig. 5). In this case, the SSC tendon lesion may be interpreted as a PTTa by radiologists due to the intact bridging fibers. However, the horizontally complete detachment from the lesser tuberosity is considered a FTT on arthroscopy. We thought this discrepant interpretation may be the possible cause of the low sensitivity for diagnosing FTT of SSC tendon in our study. Furthermore, the presence of these intact bridging fibers prevented contrast extension to the subcoracoid bursal plane, leading to an underdiagnosis of FTT to PTTa. It is important to note that an underdiagnosis of FTT of SSC tendon may occur in these circumstances, to avoid erroneous interpretation of MRA. Furthermore, a potential cause for false-negative MR findings could be lack of familiarity with detailed anatomy at the SSC tendon attachments. In addition to the aforementioned technical and anatomical factors, the lower specificity for the detection of the SSC tear may be related to scar tissue formation.
Our study has several potential limitations. First, the study was performed in the patients who had undergone arthroscopic rotator cuff repair, a population expected to have a relatively higher prevalence of high grade rotator cuff tear. However, the initial purpose of the study was focused to the preoperative evaluation of the SSC tendon tear. Second, concealed interstitial tears and bursal-surface tears were not included in this study, as the reference method of arthroscopy could not provide the information regarding these types of SSC tendon tears. However, the relative prevalence of the concealed interstitial tears as well as the bursal surface tears of the SSC tendon was relatively lower than that of the tear types included in this study. Third, we were not able to evaluate the separate diagnostic performance of MRA in each anatomical footprint (e.g., leading edge, upper tendon, middle tendon, muscular portion, and musculotendinous junction), as the performance evaluation of MRA was entirely based on the arthroscopic results. It may have influenced our observation. Fourth, because we did not use T2 TSE with fat-suppression, our results of the T2 TSE do not represent the true diagnostic accuracy of 3T MRI. Furthermore, T2-shortening effect of gadolinium-based contrast agent can lower the T2 signal intensity of the injected contrast agent, which may have contributed to lower diagnostic accuracy of T2 TSE (3132). Finally, the routine use of MRA for rotator cuff lesions has been considered controversial, because of its invasiveness, radiation hazard, and side effects of contrast media (33).
In conclusion, T1 SPIR is a more sensitive and accurate imaging sequence compared to T2 TSE in detecting SSC tendon tear on 3T MRA.
References
1. Blasier RB, Soslowsky LJ, Malicky DM, Palmer ML. Posterior glenohumeral subluxation: active and passive stabilization in a biomechanical model. J Bone Joint Surg Am. 1997; 79:433–440. PMID: 9070535.
2. Halder A, Zobitz ME, Schultz E, An KN. Structural properties of the subscapularis tendon. J Orthop Res. 2000; 18:829–834. PMID: 11117307.

3. Abboud JA, Soslowsky LJ. Interplay of the static and dynamic restraints in glenohumeral instability. Clin Orthop Relat Res. 2002; 48–57. PMID: 12072745.

4. Morag Y, Jamadar DA, Miller B, Dong Q, Jacobson JA. The subscapularis: anatomy, injury, and imaging. Skeletal Radiol. 2011; 40:255–269. PMID: 20033149.

5. Bergin D, Parker L, Zoga A, Morrison W. Abnormalities on MRI of the subscapularis tendon in the presence of a full-thickness supraspinatus tendon tear. AJR Am J Roentgenol. 2006; 186:454–459. PMID: 16423952.

6. Sakurai G, Ozaki J, Tomita Y, Kondo T, Tamai S. Incomplete tears of the subscapularis tendon associated with tears of the supraspinatus tendon: cadaveric and clinical studies. J Shoulder Elbow Surg. 1998; 7:510–515. PMID: 9814932.

7. MacMahon PJ, Taylor DH, Duke D, Brennan DD, O'Brien J, Eustace SJ. Contribution of full-thickness supraspinatus tendon tears to acquired subcoracoid impingement. Clin Radiol. 2007; 62:556–563. PMID: 17467393.

8. Burkhart SS. Arthroscopic treatment of massive rotator cuff tears. Clinical results and biomechanical rationale. Clin Orthop Relat Res. 1991; 45–56.
9. Aluisio FV, Osbahr DC, Speer KP. Analysis of rotator cuff muscles in adult human cadaveric specimens. Am J Orthop (Belle Mead NJ). 2003; 32:124–129. PMID: 12647876.
10. Foad A, Wijdicks CA. The accuracy of magnetic resonance imaging and magnetic resonance arthrogram versus arthroscopy in the diagnosis of subscapularis tendon injury. Arthroscopy. 2012; 28:636–641. PMID: 22281195.

11. Adams CR, Schoolfield JD, Burkhart SS. Accuracy of preoperative magnetic resonance imaging in predicting a subscapularis tendon tear based on arthroscopy. Arthroscopy. 2010; 26:1427–1433. PMID: 20875724.

12. Kang Y, Lee GY, Lee JW, Lee E, Kim B, Kim SJ, et al. Texture analysis of torn rotator cuff on preoperative magnetic resonance arthrography as a predictor of postoperative tendon status. Korean J Radiol. 2017; 18:691–698. PMID: 28670164.

13. Gerber C, Krushell RJ. Isolated rupture of the tendon of the subscapularis muscle. Clinical features in 16 cases. J Bone Joint Surg Br. 1991; 73:389–394. PMID: 1670434.

14. Warner JJ, Allen AA, Gerber C. Diagnosis and management of subscapularis tendon tears. Tech Orthop. 1994; 9:116–125.

15. de Jesus JO, Parker L, Frangos AJ, Nazarian LN. Accuracy of MRI, MR arthrography, and ultrasound in the diagnosis of rotator cuff tears: a meta-analysis. AJR Am J Roentgenol. 2009; 192:1701–1707. PMID: 19457838.

16. McGarvey C, Harb Z, Smith C, Houghton R, Corbett S, Ajuied A. Diagnosis of rotator cuff tears using 3-Tesla MRI versus 3-Tesla MRA: a systematic review and meta-analysis. Skeletal Radiol. 2016; 45:251–261. PMID: 26634253.

17. Pfirrmann CW, Zanetti M, Weishaupt D, Gerber C, Hodler J. Subscapularis tendon tears: detection and grading at MR arthrography. Radiology. 1999; 213:709–714. PMID: 10580943.

18. Herold T, Bachthaler M, Hamer OW, Hente R, Feuerbach S, Fellner C, et al. Indirect MR arthrography of the shoulder: use of abduction and external rotation to detect full- and partial-thickness tears of the supraspinatus tendon. Radiology. 2006; 240:152–160. PMID: 16709790.

19. Jung JY, Jee WH, Park MY, Lee SY, Kim YS. Supraspinatus tendon tears at 3.0 T shoulder MR arthrography: diagnosis with 3D isotropic turbo spin-echo SPACE sequence versus 2D conventional sequences. Skeletal Radiol. 2012; 41:1401–1410. PMID: 22322904.
20. Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977; 33:159–174. PMID: 843571.

21. Choo HJ, Lee SJ, Kim OH, Seo SS, Kim JH. Comparison of three-dimensional isotropic T1-weighted fast spin-echo MR arthrography with two-dimensional MR arthrography of the shoulder. Radiology. 2012; 262:921–931. PMID: 22267587.

22. Arai R, Sugaya H, Mochizuki T, Nimura A, Moriishi J, Akita K. Subscapularis tendon tear: an anatomic and clinical investigation. Arthroscopy. 2008; 24:997–1004. PMID: 18760206.

23. Barth JR, Burkhart SS, De Beer JF. The bear-hug test: a new and sensitive test for diagnosing a subscapularis tear. Arthroscopy. 2006; 22:1076–1084. PMID: 17027405.

24. Lafosse L, Jost B, Reiland Y, Audebert S, Toussaint B, Gobezie R. Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg Am. 2007; 89:1184–1193. PMID: 17545420.

25. Adams CR, Brady PC, Koo SS, Narbona P, Arrigoni P, Karnes GJ, et al. A systematic approach for diagnosing subscapularis tendon tears with preoperative magnetic resonance imaging scans. Arthroscopy. 2012; 28:1592–1600. PMID: 22922004.

26. Gyftopoulos S, O'Donnell J, Shah NP, Goss J, Babb J, Recht MP. Correlation of MRI with arthroscopy for the evaluation of the subscapularis tendon: a musculoskeletal division's experience. Skeletal Radiol. 2013; 42:1269–1275. PMID: 23797370.

27. Lin L, Yan H, Xiao J, He Z, Luo H, Cheng X, et al. The diagnostic value of magnetic resonance imaging for different types of subscapularis lesions. Knee Surg Sports Traumatol Arthrosc. 2016; 24:2252–2258. PMID: 25253237.

28. Yoo JC, Rhee YG, Shin SJ, Park YB, McGarry MH, Jun BJ, et al. Subscapularis tendon tear classification based on 3-dimensional anatomic footprint: a cadaveric and prospective clinical observational study. Arthroscopy. 2015; 31:19–28. PMID: 25442662.

29. Magee T. 3-T MRI of the shoulder: is MR arthrography necessary? AJR Am J Roentgenol. 2009; 192:86–92. PMID: 19098184.

30. Cash CJ, MacDonald KJ, Dixon AK, Bearcroft PW, Constant CR. Variations in the MRI appearance of the insertion of the tendon of subscapularis. Clin Anat. 2009; 22:489–494. PMID: 19306321.

31. Elster AD, Sobol WT, Hinson WH. Pseudolayering of Gd-DTPA in the urinary bladder. Radiology. 1990; 174:379–381. PMID: 2296649.

32. Lee MJ, Kim MJ, Yoon CS, Song SY, Park K, Kim WS. The T2-shortening effect of gadolinium and the optimal conditions for maximizing the CNR for evaluating the biliary system: a phantom study. Korean J Radiol. 2011; 12:358–364. PMID: 21603295.

33. Gusmer PB, Potter HG, Schatz JA, Wickiewicz TL, Altchek DW, O'Brien SJ, et al. Labral injuries: accuracy of detection with unenhanced MR imaging of the shoulder. Radiology. 1996; 200:519–524. PMID: 8685350.

Fig. 1
67-year-old woman with arthroscopically confirmed articular-sided partial-thickness SSC tendon tear.
T1-weighted spectral presaturation with inversion-recovery axial (A) and oblique sagittal (B) images and T2-weighted turbo spin-echo axial (C) and oblique sagittal (D) images demonstrate localized contrast leakage onto uppermost facet of lesser tuberosity (arrows). Large contrast-filled defect caused by complete tear of supraspinatus and infraspinatus tendons (arrowheads) is also noted. SSC = subscapularis
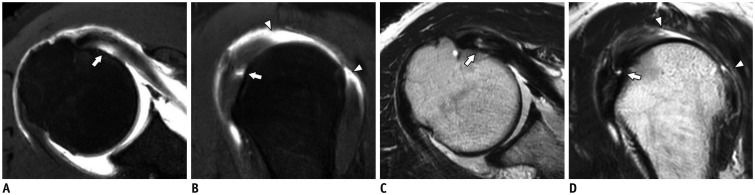
Fig. 2
64-year-old man with full-thickness SSC tendon tear diagnosed by arthroscopy.
T1-weighted spectral presaturation with inversion-recovery axial (A) and oblique sagittal (B) images and T2-weighted turbo spin-echo axial (C) and oblique sagittal (D) images reveal discontinuity of the tendon (arrows) with medial retraction.
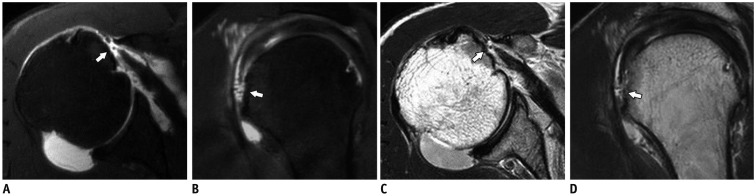
Fig. 4
68-year-old man with articular-sided partial-thickness SSC tendon tear confirmed by arthroscopy.
A, B. T1-weighted spectral presaturation with inversion-recovery axial (A) and oblique sagittal (B) images show focal contrast-filled defect in undersurface of uppermost footprint of SSC tendon (arrows), which was diagnosed as partial-thickness tear by both readers. C, D. T2-weighted turbo spin-echo axial (C) and oblique sagittal (D) images show slightly increased signal intensity of SSC tendon without fluid-equivalant signal defect (arrows), which was underdiagnosed as normal by both readers.
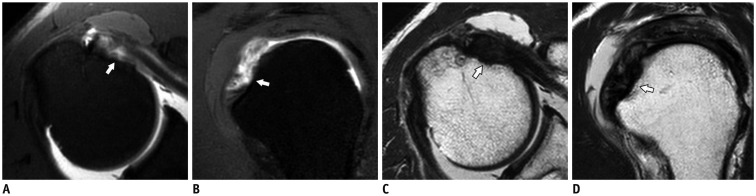
Fig. 5
68-year-old man with arthroscopically diagnosed full-thickness SSC tendon tear.
A, B. T1-weighted spectral presaturation with inversion-recovery axial (A) and oblique sagittal (B) images show detachment of SSC tendon from lesser tuberosity with contrast filling (arrows). Superficial “bridging fiber” remains without retraction, which have continuity with fibers overlying bicipital groove and anterior-most fibers of supraspinatus tendon (arrowheads). Both readers underdiagnosed as partial-thickness SSC tear. Accompanied full-thickness supraspinatus tendon tear (asterisk) with contrast leakage into subacromial-subdeltoid bursal space is also shown.
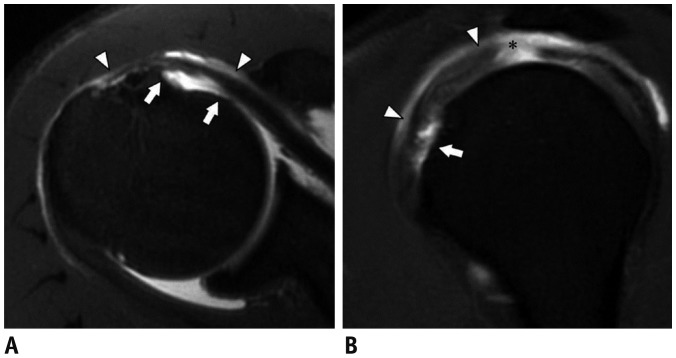
Table 1
Sequence Parameters for MRA
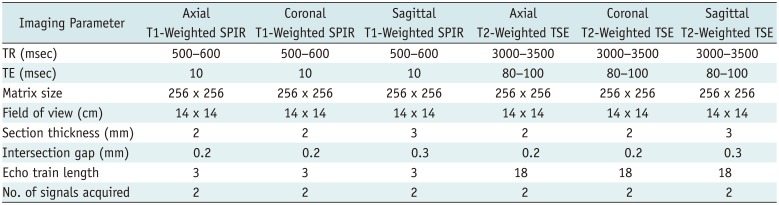
Table 2
Diagnostic Performance of T1 SPIR and T2 TSE for Detection of SSC Tendon Tear
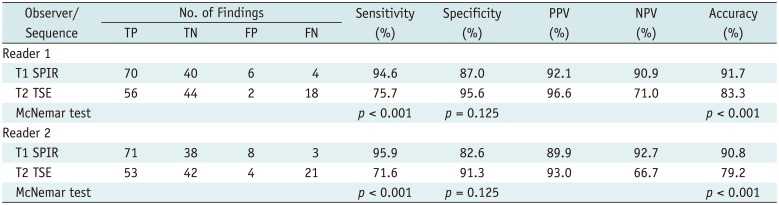
Table 3
Diagnostic Performance of T1 SPIR and T2 TSE for Diagnosis of Full-Thickness and Articular-Surface Partial-Thickness SSC Tendon Tear




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download