Abstract
Objective
Described herein is a microcatheter looping technique to facilitate aneurysm selection in paraclinoid aneurysms, which remains to be technically challenging due to the inherent complexity of regional anatomy.
Materials and Methods
This retrospective study was approved by our Institutional Review Board, and informed consent was waived. Microcatheter looping method was employed in 59 patients with paraclinoid aneurysms between January 2012 and December 2013. In the described technique, construction of a microcatheter loop, which is steam-shaped or pre-shaped, based on the direction of aneurysms, is mandatory. The looped tip of microcatheter was advanced into distal internal carotid artery and positioned atop the target aneurysm. By steering the loop (via inner microguidewire) into the dome of aneurysm and easing tension on the microcatheter, the aneurysm was selected. Clinical and morphologic outcomes were assessed with emphasis on technical aspects of the treatment.
Results
Through this looping technique, a total of 59 paraclinoid aneurysms were successfully treated. After aneurysm selection as described, single microcatheter technique (n = 25) was most commonly used to facilitate coiling, followed by balloon protection (n = 21), stent protection (n = 7), multiple microcatheters (n = 3), and stent/balloon combination (n = 3). Satisfactory aneurysmal occlusion was achieved through coil embolization in 44 lesions (74.6%). During follow-up of 53 patients (mean interval, 10.9 ± 5.9 months), only one instance (1.9%) of major recanalization was observed. There were no complications related to microcatheter looping.
Paraclinoid (or paraophthalmic) aneurysms generally are lesions arising from a segment of internal carotid artery (ICA), between roof of cavernous sinus and origin of posterior communicating artery (123). Endovascular coil embolization has been widely employed for the treatment of intracranial aneurysms since the International Subarachnoid Aneurysm Trial and the International Study of Unruptured Intracranial Aneurysms (3456). Recently, improved protection devices and advanced coiling techniques, such as balloon remodeling and stenting, have enabled coil embolization of aneurysms with complex configurations (7891011). However, the distinctive angio-anatomic configurations of paraclinoid aneurysms continue to challenge coil embolization (12). Because such lesions uniformly are juxtadistal to a sharply curved carotid siphon, microcatheter aneurysm selection is technically demanding. A microcatheter looping method that facilitates selection of paraclinoid aneurysms is presented herein, along with angiographic and clinical outcomes supporting use of this technique.
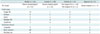
Between January 2012 and December 2013, 908 intracranial aneurysms in 768 patients were subjected to endovascular treatment, including 215 paraclinoid aneurysms. Patients with ICA-ophthalmic artery aneurysms qualified for study, but cavernous ICA aneurysms proximal to carotid siphon were excluded, as those were dissecting, fusiform, false, or blood-blister-like aneurysms. Our microcatheter looping method for aneurysm selection was applied in 59 patients (female, 50; male, 9; mean age, 53.5 ± 9.3 years). All lesions were unruptured aneurysms (one recanalized), classifiable as either superior, inferior medial, or lateral type, based on direction of aneurysmal dome relative to carotid siphon. All lesions had diameters smaller than 10 mm (mean, 4.6 ± 1.2; range, 2.6-9.1 mm). Therapeutic decisions were rendered through multidisciplinary deliberation by both neurosurgeons and nonsurgical neurointerventionists, and informed consent was obtained from all patients, once need for treatment and related risks were adequately explained. This study was approved by the Institutional Review Board of our hospital. Clinical and radiographic features of the cohort are shown in Table 1.
Technical steps in the microcatheter looping technique (for aneurysm selection) are as follows: 1) identifying proper microcatheter shape; 2) forming the looped microcatheter tip; 3) positioning the looped microcatheter in distal ICA, atop aneurysm; 4) steering microcatheter tip (via inner microguidewire) into dome of aneurysm; and 5) releasing of tension on microcatheter, thus facilitating insertion into aneurysm sac. Corresponding schematics are shown in Figure 1.
The first step of this technique is identifying proper microcatheter shape, according to type of aneurysm and direction of dome (Table 2). The process of making a loop of a microcatheter tip, as next step, is reported elsewhere (713). The looping generally is achieved without great difficulty under the following conditions: 1) the microcatheter passes through carotid siphon; 2) microcatheter advances under the guidance of looped microguidewire between cervical ICA and cavernous ICA; and 3) guiding catheter moves from distal common carotid artery to proximal ICA (with microcatheter placed in proximal external carotid artery). Once formed, the microcatheter loop is advanced to distal ICA and positioned atop the aneurysm. If microcatheter tip and dome of aneurysm are directed differently, the tip may be steered into the dome, via an inner microguidewire. Subsequently, tension on the microcatheter is slowly eased, allowing the tip to insert into dome and the loop to untie. For this purpose, a short, tight angle of microguidewire tip is preferable to a long, loose angle. Microguidewire steering is unnecessary for a microcatheter tip directed similarly to dome of aneurysm (Fig. 2). In some instances, aneurysm selection was achieved simply by advancing the looped microcatheter (Supplementary Video 1 in the online-only Data Supplement).
Most of the procedures were performed under general anesthesia. Aneurysmal configuration and arterial architecture were evaluated using the Integris V (Philips Medical Systems, Best, the Netherlands) and Innova IGS 630 (GE Healthcare, Milwaukee, WI, USA) biplane system, including three-dimensional rotational angiography. All patients were managed with antiplatelet agent before coiling in a relatively consistent scheme at our institution (14). After femoral sheath placement, systemic heparinization was started with a loading dose of 3000 IU and was maintained with a dose of 1000 IU on an hourly basis. After the procedure, antiplatelet medications were not routinely prescribed for maintenance except in case of stent protection, coil protrusion, and procedural thromboembolism.
Immediate angiographic results after coil embolization were classified according to a 3-point Raymond scale: complete obliteration (no residual filling of contrast medium in the aneurysms), residual neck (the persistence of any portion of the original defect of the arterial wall), and residual aneurysm (any opacification of the sac) (15).
Clinical outcomes were assessed with the Glasgow outcome scale (GOS), which was applied throughout the hospitalization period and at the last available clinical follow-up. Two experienced neurointerventionists who were blinded to the immediate post-embolization angiogram independently reviewed anatomical follow-up results and categorized as follows: stable occlusion (no interval change since the procedure or progressive thrombosis within the aneurysm); minor recanalization (progressive filling limited at the neck of the aneurysm); and major recanalization (the aneurysmal sac filling) (16). Conventional angiography and repetitive embolization was recommended for patients, who presented with major recanalization.
Our looping technique was largely applied to medially directed paraclinoid aneurysms (n = 31, steamed pigtail-shaped tip), followed by those directed inferiorly (n = 11, chiefly pre-shaped 90° microcatheter), laterally (n = 10, steamed pigtail-shaped tip), and superiorly (n = 7, steamed S-shaped tip) (Table 2). Technical success was achieved in all cases. In the majority of cases (n = 45, 76.3%), the technique was applied following the failure of the standard methods, except for 14 cases in which the microcatheter loop was spontaneously formed in the process of advancement of microcatheter in the carotid siphon. Following this approach, a single microcatheter (n = 25), without protection device, was most often used to facilitate coiling, followed by balloon remodeling (n = 21), stent protection (n = 7), multiple microcatheters (n = 4), and stent/balloon combination (n = 3). The coiling techniques that were applied varied, depending on direction of aneurysm. Aneurysms directed inferiorly usually entailed use of a single microcatheter, without protection device, whereas most aneurysms directed superiorly or laterally required balloons or stents (Table 2). Immediate post-procedural angiographic assessment revealed complete occlusion in nine aneurysms (15.3%), residual neck in 35 (59.3%), and residual aneurysm in 15 (25.4%) cases. Although a post-procedural symptomatic thrombus did develop in one patient, who underwent stent insertion and responded poorly to clopidogrel, there were no adverse events related to this microcatheter looping technique. All patients were neurologically intact (GOS 5) at the time of discharge, with one exceptional demonstrating symptomatic thrombus (GOS 4).
Follow-up radiologic imaging was performed at least 6 months after coil embolization in 53 aneurysms (mean interval, 10.9 ± 5.9 months), except in five recently treated aneurysms (< 6 months), for a follow-up rate of 98.1% (53/54). Stable occlusion was observed in 48 aneurysms (90.6%), minor recanalization in four (7.5%), and major recanalization in one (1.9%). The patient with major recanalization underwent repeat endovascular coiling. Follow-up angiography 6 months after re-embolization showed stable occlusion. During the follow-up period, none of the patients suffered delayed cerebral infarction.
A 32-year-old woman was admitted for endovascular treatment of an unruptured paraclinoid aneurysm (maximum diameter, 3.3 mm; dome-to-neck ratio, 1.1) with small bleb. She was seeking treatment because of her young age and a family history of subarachnoid hemorrhage. A 6-Fr guiding catheter was advanced into cervical ICA. Because the aneurysm was superiorly directed (relative to carotid siphon), an S-shaped microcatheter (Excelsior SL-10, Stryker, Fremont, CA, USA) was configured by steaming. Traditional maneuvers, including forward or backward movement and inner microguidewire steering, failed to select the aneurysm. After looping of the microcatheter (via microguidewire loop) in cavernous ICA, it was advanced to distal ICA, overlying the aneurysm. The inferiorly directed microcatheter was steered superiorly to align with the dome of aneurysm. Slow release of tension on the microcatheter subsequently allowed its tip to enter aneurysmal sac. Thereafter, coil insertion was performed under the balloon protection. Post-embolization angiography showed successful occlusion of the aneurysm sac, and the patient was discharged the following day, free of complications. At a 6-month follow-up visit, magnetic resonance angiography confirmed stable occlusion of aneurysm (Fig. 3).
Despite improvements in protection devices and coiling techniques (i.e., balloon remodeling and stenting) applicable to more complex scenarios, coil embolization of paraclinoid aneurysms is still a challenge, due to the inherently difficult angio-anatomy (17). Such aneurysms commonly are situated juxtadistal to a sharply angled carotid siphon. The two major technical issues encountered in managing these lesions include problematic microcatheter aneurysm selection and kick-back during coil insertion due to lack of microcatheter support. Consequently, embolization may fail or fall short, conferring unsatisfactory post-procedural occlusion.
One of the most important factors in microcatheter selection of intracranial aneurysms (including paraclinoid aneurysms) is a properly configured distal tip, either pre-shaped or steam-shaped (121819). As shown in Table 2, consistencies in microcatheter shape are evident, depending on how a dome of aneurysm is directed (relative to carotid siphon). Methods for the shaping of microcatheter tips in this context are reported elsewhere, but once an appropriate shape is found or generated, the traditional means of selecting aneurysms by microcatheter include antegrade or retrograde microcatheter shift, inner microguidewire steering, or microguidewire guidance (12). Sometimes these options fail, and microguidewire-guided aneurysm selection does carry a risk of aneurysmal perforation, if navigation in tortuous arteries is poorly controlled. In such disadvantaged situations, the looping method described here may be useful, although it is not presently advocated as a first-line maneuver. The efficacy and safety of this approach must first be established in a larger study population.
Once aneurysm selection is achieved, kick-back may be problematic during coiling due to lack of microcatheter support. In this regard, steamed S- and pigtail-shaped microcatheters tend to offer less resistance (17). Kick-back is also related to arterial tortuosity and direction of aneurysm near/with respect to carotid siphon. Thus, devices that enhance microcatheter support and provide neck protection against coil protrusion are often required to complete coiling. In our series, 52.5% of treated aneurysms required balloon remodeling or stent protection. There may be a concern that making a loop or advancement of the looped microcatheter might cause internal injury of the parent artery (and possibly dissection), although there was no such case in our series. Such an event could possibly be circumvented by the use of microcatheters with acute-angled tips, including pigtail or J.
Above-mentioned angio-anatomic and technical difficulties made successful occlusion (complete occlusion or neck remnant) of paraclinoid aneurysms, which are comparatively hard to achieve in the immediate aftermath of coil embolization. However, therapeutic success rates in follow-up imaging of these lesions fared better than the ones determined in the immediate aftermath. This phenomenon may be attributable to progressive thrombosis, impacted by aneurysmal configuration (small size and nature of side-wall) and hemodynamic buffering by carotid siphon.
In conclusion, a novel microcatheter looping technique employed to treat successfully 59 paraclinoid aneurysms appeared to be safe and is proposed as a viable alternative to traditional maneuvers.
Figures and Tables
Fig. 1
Schematic illustration (I) of microcatheter looping for aneurysm selection.
A. Microcatheter loop shaped in cavernous internal carotid artery (ICA), after appropriate selection/configuring of microcatheter tip angle. B. Looped microcatheter tip advanced to distal ICA, atop aneurysm. C. Torque of inner microguidewire directs microcatheter tip to aneurysmal sac. D. Release of tension on microcatheter eases tip into sac of aneurysm.

Fig. 2
Schematic illustration (II) of microcatheter looping for aneurysm selection.
A. Paraclinoid aneurysm with dome superiorly directed; steam configured S-shaped microcatheter looped in cavernous internal carotid artery (ICA). B. Microcatheter tip directed to dome of aneurysm as looped microcatheter advanced to distal ICA. C. Release of microcatheter tension enables insertion into sac of aneurysm.

Fig. 3
Illustrative case.
A. Paraclinoid aneurysm with superior direction on left internal carotid artery (ICA) angiography. B. After microcatheter was shaped to "S" using steam, looping of microcatheter tip was achieved using microguidewire loop. Looped microcatheter was advanced into distal ICA over aneurysm. C. Microcatheter tip was directed differently from aneurysm direction. D. Inferiorly directed microcatheter was steered superiorly to align with dome of aneurysm. E. Tension of microcatheter was released to select aneurysm, and then microcatheter tip was inserted into aneurysm sac, untying loop. F. Coil embolization was performed using balloon protection. G. Aneurysm was completely occluded. H. Six-month follow-up MR angiography showed that aneurysm was stably occluded.

Table 1
Characteristics of Patients with Paraclinoid Aneurysm Treated by Looping Method

Table 2
Characteristics of Paraclinoid Aneurysms, Grouped by Directions of Aneurysms
References
1. Wang Y, Li Y, Jiang C, Jiang F, Meng H, Siddiqui AH, et al. Endovascular treatment of paraclinoid aneurysms: 142 aneurysms in one centre. J Neurointerv Surg. 2013; 5:552–556.
2. Hoh BL, Carter BS, Budzik RF, Putman CM, Ogilvy CS. Results after surgical and endovascular treatment of paraclinoid aneurysms by a combined neurovascular team. Neurosurgery. 2001; 48:78–89. discussion 89-90
3. Kwon WH, Jeong HW, Kim ST, Seo JH. Angiographic and clinical result of endovascular treatment in paraclinoid aneurysms. Neurointervention. 2014; 9:83–88.
4. Molyneux A, Kerr R, Stratton I, Sandercock P, Clarke M, Shrimpton J, et al. International Subarachnoid Aneurysm Trial (ISAT) of neurosurgical clipping versus endovascular coiling in 2143 patients with ruptured intracranial aneurysms: a randomised trial. Lancet. 2002; 360:1267–1274.
5. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 362:103–110.
6. Cho YD, Sohn CH, Kang HS, Kim JE, Cho WS, Hwang G, et al. Coil embolization of intracranial saccular aneurysms using the Low-profile Visualized Intraluminal Support (LVIS™) device. Neuroradiology. 2014; 56:543–551.
7. Cho YD, Kang HS, Kim JE, Son YJ, Lee JY, Lee SJ, et al. Microcatheter looping technique for coil embolization of complex configuration middle cerebral artery aneurysms. Neurosurgery. 2012; 71:1185–1191. discussion 1191
8. Pierot L, Cognard C, Spelle L, Moret J. Safety and efficacy of balloon remodeling technique during endovascular treatment of intracranial aneurysms: critical review of the literature. AJNR Am J Neuroradiol. 2012; 33:12–15.
9. Lee JY, Seo JH, Cho YD, Kang HS, Han MH. Endovascular treatment of wide-neck intracranial aneurysms using a microcatheter protective technique: results and outcomes in 75 aneurysms. AJNR Am J Neuroradiol. 2011; 32:917–922.
10. Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery. 2007; 61:460–468. discussion 468-469
11. Lee SJ, Cho YD, Kang HS, Kim JE, Han MH. Coil embolization using the self-expandable closed-cell stent for intracranial saccular aneurysm: a single-center experience of 289 consecutive aneurysms. Clin Radiol. 2013; 68:256–263.
12. Kwon BJ, Im SH, Park JC, Cho YD, Kang HS, Kim JE, et al. Shaping and navigating methods of microcatheters for endovascular treatment of paraclinoid aneurysms. Neurosurgery. 2010; 67:34–40. discussion 40
13. Kwon BJ, Seo DH, Ha YS, Lee KC. Endovascular Treatment of Wide-necked Cerebral Aneurysms with an Acute Angle Branch Incorporated into the Sac: Novel methods of Branch Access in 8 Aneurysms. Neurointervention. 2012; 7:93–101.
14. Kang HS, Kwon BJ, Kim JE, Han MH. Preinterventional clopidogrel response variability for coil embolization of intracranial aneurysms: clinical implications. AJNR Am J Neuroradiol. 2010; 31:1206–1210.
15. Roy D, Milot G, Raymond J. Endovascular treatment of unruptured aneurysms. Stroke. 2001; 32:1998–2004.
16. Kang HS, Han MH, Kwon BJ, Kwon OK, Kim SH, Choi SH, et al. Short-term outcome of intracranial aneurysms treated with polyglycolic acid/lactide copolymer-coated coils compared to historical controls treated with bare platinum coils: a single-center experience. AJNR Am J Neuroradiol. 2005; 26:1921–1928.
17. Ahn JH, Cho YD, Kang HS, Kim JE, Cho WS, Jung SC, et al. Endovascular treatment of ophthalmic artery aneurysms: assessing balloon test occlusion and preservation of vision in coil embolization. AJNR Am J Neuroradiol. 2014; 35:2146–2152.
18. Lee WJ, Cho YD, Kang HS, Kim JE, Cho WS, Kim KM, et al. Endovascular coil embolization in internal carotid artery bifurcation aneurysms. Clin Radiol. 2014; 69:e273–e279.
19. Cho YD, Lee WJ, Kim KM, Kang HS, Kim JE, Han MH. Endovascular coil embolization of middle cerebral artery aneurysms of the proximal (M1) segment. Neuroradiology. 2013; 55:1097–1102.
Supplementary Materials
The online-only Data Supplement is available with this article at http://dx.doi.org/10.3348/kjr.2015.16.4.899.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download