Abstract
Objective
To evaluate the retrieval rate and accuracy of ultrasound (US)-guided 14-G semi-automated core needle biopsy (CNB) for microcalcifications in the breast.
Materials and Methods
US-guided 14-G semi-automated CNB procedures and specimen radiography were performed for 33 cases of suspicious microcalcifications apparent on sonography. The accuracy of 14-G semi-automated CNB and radiology-pathology concordance were analyzed and the microcalcification characteristics between groups with successful and failed retrieval were compared.
Results
Thirty lesions were successfully retrieved and the microcalcification retrieval rate was 90.9% (30/33). Thirty lesions were successfully retrieved. Twenty five were finally diagnosed as malignant (10 invasive ductal carcinoma, 15 ductal carcinoma in situ [DCIS]) and five as benign. After surgery and mammographic follow-up, the 25 malignant lesions comprised 12 invasive ductal carcinoma and 13 DCIS. Three lesions in the failed retrieval group (one DCIS and two benign) were finally diagnosed as two DCIS and one benign after surgery. The accuracy of 14-G semi-automated CNB was 90.9% (30/33) because of two DCIS underestimates and one false-negative diagnosis. The discordance rate was significantly higher in the failed retrieval group than in the successful retrieval group (66.7% vs. 6.7%; p < 0.05). Punctate calcifications were significantly more common in the failed retrieval group than in the successful retrieval group (66.7% vs. 3.7%; p < 0.05).
Standard of care for suspicious microcalcifications in the breast is stereotactic-guided percutaneous biopsy or mammography (MG)-guided wire localization and surgical excision (1). Stereotactic biopsy, however, requires a sufficient breast volume to guarantee a safe procedure limiting its universal application.
Ultrasound (US)-guided biopsy has many advantages over the MG-guided procedure including no ionizing radiation, greater patient comfort, no need for breast compression, real-time confirmation of needle location, lower cost, and universally available sonography equipment (1-4). Improvements in the resolution of sonographic equipment have led to the use of US-guided biopsy for histologic assessment of suspicious microcalcifications in the breast those are apparent on sonography (1, 5-12). Due to its higher sensitivity and lower rate of common sampling errors, US-guided vacuum-assisted biopsy (VAB) has been preferred to 14-gauge (G) automated core needle biopsy (CNB) (5, 6, 10-12).
14-G semi-automated CNB is a coaxial system similar to VAB in terms of the single skin puncture and repeated needle passes. Using an introducer, radiologists can precisely obtain contiguous tissue specimens and reduce the procedure time. Additionally, 14-G semi-automated CNB device is less costly than the VAB device.
The purpose of the present study was to evaluate the rate of successful retrieval of microcalcifications and diagnostic accuracy of US-guided 14-G semi-automated CNB for suspicious microcalcifications in the breast those were apparent on sonography.
Between January 2008 and September 2011, 138 lesions containing isolated suspicious microcalcifications without an associated mass or asymmetry were detected on contact MG. Based on findings from magnified images, each lesion was categorized as suspicious (category 4) or highly suggestive of malignancy (category 5) according to the American College of Radiology Breast Imaging-Reporting and Data System (BI-RADS) (13). Category 4 lesions were subcategorized as low (A), intermediate (B), or moderate (C) suspicious lesions.
To select between US-guided 14-G semi-automated CNB and MG-guided wire localization and surgical excision, targeted US was performed for all suspicious calcifications. We prospectively determined the biopsy method and excluded lesions that were not apparent on US. In addition, lesions located in the posterior portion of the mammary zone of very thin patients who had obliterated retromammary fat layer were excluded to avoid complications such as pneumothorax. Finally, 33 consecutive lesions were selected for US-guided 14-G semi-automated CNB and were enrolled into the study. Written informed consent for US-guided 14-G semi-automated CNB was obtained from all patients and institutional review board approval was obtained from our institute.
Targeted US (iU22®; Philips, Bothell, WA, USA) examination was performed using a linear array transducer (L12-5) to identify a correlating lesion containing microcalcifications. Unilateral orthogonal mammographic views were obtained with a skin marker only when there was uncertainty about the mammography-sonography correlation. The biopsy was performed using a STERICUT® 14-G semi-automated CNB set (TSK Laboratory, Tochigi, Japan). One breast radiologist with 10 years of experience performed both breast US and US-guided 14-G semi-automated CNB in all cases.
For biopsy, the skin was punctured using an introducer with a stylet and advanced forward near the margin of the lesion. The stylet was removed and a biopsy gun was inserted through the introducer. The biopsy needle was pushed manually into the lesion. The location of the needle within the lesion was confirmed on transverse and longitudinal scans. The biopsy gun was fired, causing it to follow the biopsy needle and remove tissue from the lesion. The biopsy gun was then withdrawn through the introducer and the needle was pushed manually. The specimen could then be observed in the notch. Insertion of the biopsy gun through the introducer was repeated after changing the angle of insertion. Several cores of more than 1 cm length were obtained for each lesion. A 1- or 2-cm cutting edge excursion could be used; we usually selected a 2-cm excursion.
After the biopsy, the retrieved cores were placed on wet paper or a plastic weigh boat and specimen radiography (Senograph DS®; GE, Buc, France) was performed to identify the presence of microcalcifications. The parameters of exposure for specimen radiography were 22 kVp, 8 mAs, and 1.8 × magnification. A core containing any calcification on specimen radiography was defined as a successfully retrieved core. The total number of retrieved cores, the number of successfully retrieved cores containing any calcification, and the total number of calcifications on specimen radiography were enumerated.
Concordance between the MG findings of microcalcifications and the results of US-guided 14-G semi-automated CNB was reviewed. Radiology-pathology concordance was considered when a BI-RADS category 4 or higher lesion showed a malignant result on 14-G semiautomated CNB. There were two exceptions for category 4A lesions. In low suspicious lesions, 14-G semi-automated CNB results showing a specific benign diagnosis, such as fibroadenoma or fat necrosis, were considered to be concordant. Also, nonspecific benign results, such as fibrocystic changes (FCC), were considered to be concordant in low suspicious lesions. In contrast, for category 4B or higher lesions, nonspecific benign results were considered to be discordant because of the possible sampling error.
Additionally, we reviewed the accuracy of US-guided 14-G semi-automated CNB of microcalcifications by comparing the results with surgical pathology. When both results were the same, the 14-G semi-automated CNB was considered accurate. If the 14-G semi-automated CNB result of ductal carcinoma in situ (DCIS) yielded a diagnosis of invasive ductal carcinoma (IDC) in a subsequent surgery, it was deemed a DCIS underestimate. If the 14-G semi-automated CNB result of atypical ductal hyperplasia (ADH) or ductal intraepithelial neoplasia (DIN) 1B yielded a diagnosis of DCIS in a subsequent surgical excision, it was deemed an ADH underestimate.
Mean lesion size, morphology, and distribution of microcalcifications on magnified images, and associated features of calcifications, such as mass or non-mass lesions on US, were analyzed. These factors were compared between the successful and failed retrieval groups. Biopsy-related complications including infection, hemorrhage, and pneumothorax were checked by radiology reports and chart review.
The chi-square test and Fisher's exact test were performed for nonparametric variables and Student's t test was performed for parametric interference. Statistical analyses were performed using SPSS 17.0 software (SPSS Inc., Chicago, IL, USA). p values < 0.05 were considered to indicate statistical significance.
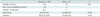
Thirty-three (23.9%, 33/138) lesions in 32 patients were subjected to US-guided 14-G semi-automated CNB. One patient had suspicious microcalcifications in both breasts. Other suspicious microcalcifications underwent MG-guided wire localization excision (76.1%, 105/138). Mean patient age was 49 years (range, 24-67 years). Thirty patients were asymptomatic and were detected on screening MG. One patient had bloody nipple discharge and the other had palpable cancer in the upper inner quadrant and incidental suspicious microcalcifications in the lower inner quadrant of the same breast. Magnified images identified four low suspicious lesions (4A; 15.2%), five intermediate suspicious lesions (4B; 12.1%), eight moderate suspicious lesions (4C; 24.2%), and 16 highly suggestive of malignancy lesions (5; 48.5%) (Table 1).
Calcifications were successfully retrieved in 30/33 lesions (90.9%) and confirmed on specimen radiography. No complications related to 14-G semi-automated CNB were observed. Thirty cases of successfully retrieved microcalcifications were assigned to the successful retrieval group and the remaining three lesions were assigned to the failed retrieval group. Results of US-guided 14-G semi-automated CNB identified 26 (78.8%) malignant and seven (21.2%) benign lesions (Fig. 1). The successful retrieval group comprised 25 malignant (15 DCIS and 10 IDC) and five benign lesions. The five benign lesions were one ADH (or DIN 1B), one columnar cell hyperplasia (CCH), one FCC, one fibroadenoma, and one fat necrosis. In the failed retrieval group, one DCIS and two FCC were identified.
After 14-G semi-automated CNB, 30 lesions underwent cancer surgery (n = 26) or repeated biopsy after MG-guided wire localization (n = 4), and final pathology results were provided (Fig. 1). Of the 16 DCIS on 14-G semi-automated CNB, 14 were confirmed to be DCIS on final pathology (Fig. 2). The remaining two DCIS, which belonged to the successful retrieval group, were upgraded to IDC. The rate of DCIS underestimates was 12.5% (2/16) and their BIRADS assessments were category 4C and 5, respectively. All 10 IDC on 14-G semi-automated CNB were confirmed to be IDC on final pathology. Of the seven benign lesions, four underwent MG-guided wire localization and excision, and were finally diagnosed as three FCC and one DCIS. The latter was the only false-negative case of 14-G semi-automated CNB and belonged to the failed retrieval group. The other three benign lesions underwent mammographic follow-up for 2 years and no missed cancers were found. There was no ADH underestimate.
According to the BI-RADS categories, three of four category 4A calcifications were successfully retrieved on US-guided 14-G semi-automated CNB. The results were all benign (one fibroadenoma, one fat necrosis, and one FCC) and concordant (Table 1). None of the successfully retrieved benign lesions showed a missed cancer after 2 years of mammographic follow-up. One low suspicious lesion diagnosed as DCIS on biopsy, despite failed retrieval of microcalcifications, was finally confirmed to be DCIS after surgery, confirming the 14-G semi-automated CNB results to be accurate.
Four of five category 4B calcifications were successfully retrieved and 14-G semi-automated CNB results were all malignant (one DCIS and three IDC) and concordant (Table 1). All lesions were finally diagnosed as one DCIS and three IDC after breast cancer surgery, confirming the 14-G semi-automated CNB results to be accurate. Microcalcification retrieval failed in one intermediate suspicion lesion. Although the 14-G semi-automated CNB result was FCC and considered to be discordant, the lesion was finally diagnosed as FCC after MG-guided wire localization excision, confirming the 14-G semi-automated CNB result to be accurate. All of the category 4C lesions were successfully retrieved and the 14-G semi-automated CNB results were one ADH (or DIN 1B), four DCIS, and three IDC. The ADH case was considered discordant, but was finally confirmed to be FCC after MG-guided wire localization excision, confirming the 14-G semi-automated CNB result to be accurate. All of the moderate suspicious lesions except one were finally confirmed to be malignant after breast cancer surgery. In one case among them, however, the final pathology result was upgraded to IDC, confirming the 14-G semi-automated CNB result to be a DCIS underestimate.
Of the 16 category 5 calcifications, 15 were successfully retrieved (Table 1). The 14-G semi-automated CNB results in the successful retrieval group were 10 DCIS, four IDC, and one CCH. Of the category 5 lesions, 14 were finally diagnosed as malignancy after surgery. In one case, however, the final pathology result was upgraded to IDC, confirming the 14-G semi-automated CNB result to be a DCIS underestimate. The CCH case was considered to be discordant, but was finally confirmed to be FCC after MG-guided wire localization excision, confirming the 14-G semi-automated CNB result to be accurate (Fig. 3). Retrieval of calcification failed in one highly suspicious lesion and its 14-G semi-automated CNB result was FCC, which was considered to be discordant. The case was finally diagnosed as DCIS after MG-guided wire localization and surgical excision, confirming the 14-G semi-automated CNB result to be a false-negative.
Of the 30 lesions in the successful retrieval group, two (6.7%) showed a radiology-pathology discordance, whereas two of the three (66.7%) lesions in the failed retrieval group showed discordance. The discordance rate was higher in the failed retrieval group (p = 0.035). Of the 30 lesions in the successful retrieval group, 28 (93.3%) lesions were accurately diagnosed, and two of the three (66.7%) lesions in the failed retrieval group were accurately diagnosed. The accuracy of 14-G semi-automated CNB was not significantly different (p = 0.256). The overall accuracy of US-guided 14-G semi-automated CNB was 90.9% (30/33) because of two DCIS underestimates and one false-negative case.
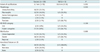
We compared the characteristics of specimen radiography according to the retrieval of calcifications (Table 2). The total number of retrieved cores did not differ between groups: 6.5 (range, 4-9) in the successful retrieval group and 7.3 (range, 6-10) in the failed retrieval group (p = 0.61). In the successful retrieval group, the mean number of cores containing calcification was 4.8 (range, 1-8) and the mean total number of calcifications in the retrieved cores was 24 (range, 2-101).
We reviewed imaging findings of microcalcifications, including the extent of the calcification, morphology, and distribution on MG, and associated features on US (Table 3). Based on the MG findings, the extent of calcification did not differ between two groups (16.7 mm [range, 3-70 mm] in the successful retrieval group and 18.0 mm [range, 9-30 mm] in the failed retrieval group, p = 0.093). Punctate (66.7%, 2/3) calcifications were more common in the failed retrieval group than in the successful retrieval group (p = 0.033). Linear/branching (33.3%, 10/30) and coarse heterogeneous (16.7%, 5/30) calcifications were more common in the successful retrieval group. The proportions of linear/segmental and clustered distributions were similar in both groups (36.7% vs. 33.3%; 60.0% vs. 66.7%; p = 0.095). On US, microcalcifications were associated with mass (63.3%; 19/30) or non-mass (30.0%; 9/30) lesions in the successful retrieval group, whereas they were associated with mass (100%, 3/3) in the failed retrieval group.
For suspicious microcalcifications in the breast those are either not palpable or not associated with a mass on MG, standard of care is stereotactic-guided VAB or MG-guided wire localization and surgical excision (1, 2, 9, 14). Stereotactic equipment, however, is not universally applicable. Further, an adequate breast thickness is essential for safe procedures (15). As high-resolution sonography equipment is universally available, US-guided VAB can be an effective alternative to stereotactic-guided VAB for suspicious calcifications in the breast (10-12). VAB is superior to automated CNB for the retrieval of microcalcifications because the former provides larger tissue specimens and contiguous sampling (1-3, 5, 6, 9-12, 14).
On the other hand, using a 14-G semi-automated CNB device, radiologists can precisely obtain multiple cores of calcifications because the introducer reduces reverberation artifacts and the possibility of missing the target (16). The cost of 14-G semi-automated CNB is lower than that of VAB. Using an introducer in the semi-automated gun does not significantly add to the cost. Thus, US-guided 14-G semi-automated CNB may be an acceptable and cost-effective procedure for suspicious microcalcifications compared with US-guided VAB.
In the present study, the retrieval rate of microcalcifications using the semi-automated gun was 91%. The retrieval rates of microcalcifications in VAB are reported to be 91-100% under stereotactic guidance (1, 2) and 71-97% under US guidance (10-12). Thus, in the retrieval of microcalcifications, US-guided 14-G semi-automated CNB is comparable to VAB, particularly considering the smaller tissue specimens and lower cost. The retrieval rate of microcalcifications using an automated gun is 86-94% (1, 2) and the results of the present study are comparable to US-guided automated CNB. Interestingly, the retrieval rate in the present study was superior to that in a report of US-guided VAB (91% vs. 71%) (11). This difference may be related to the exclusion criteria used in the present study. We excluded calcifications that were located in the posterior portion of the mammary zone in very thin patients who had obliterated retromammary fat layer to avoid pneumothorax. Cho et al. (11) reported that microcalcifications located in the anterior or middle part of the breast were retrieved more frequently than those in the posterior part of the breast. The lower retrieval of the latter likely reflected the difficulty in inserting a biopsy needle to a sufficiently deep position because of fear of an iatrogenic pneumothorax. So, the retrieval rate of posteriorly located calcifications was lower than that of other calcifications.
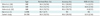
The accuracy of 14-G semi-automated CNB was 91%, due to the two DCIS underestimates and one false-negative diagnosis. The accuracies of US-guided VAB were 94-96% (Table 4) (10-12). These excellent results, however, came from a mean of 10-17 VAB cores, which represent larger tissue specimens compared with stereotactic-guided VAB (mean, 11-13 cores) (1, 2) and a mean of seven cores in the present study.
Histologic underestimation by 14-G semi-automated CNB is mostly an issue in calcified lesions rather than in mass lesions, and DCIS underestimates are more common in 14-G semi-automated CNB than that of VAB due to sampling error (2). In stereotactic-guided biopsy of microcalcifications, the rate of DCIS underestimates is reported to be 16-37% with 14-G semi-automated CNB and 0-23% with VAB (2, 9, 14). In US-guided biopsy of microcalcifications, the rate of DCIS underestimates ranges from 7-19% with VAB (Table 4) (10-12). Hahn et al. (12) reported a rate of DCIS underestimates of 0%, but an ADH (or DIN 1B) underestimation of 33% (1/3). In the present study, the rate of DCIS underestimates of 14-G semi-automated CNB was 13% (2/16), which is comparable to that of US-guided VAB and there was no ADH underestimate.
One false-negative diagnosis was identified. The MG finding in that case was segmental fine pleomorphic calcifications and was assessed as a BI-RADS category 5. On sonography, a few calcifications with subtle non-mass lesions were identified. US-guided VAB or MG-guided wire localization excision would be a more desirable procedure for the particular case. Fortunately, the discordant 14-G semi-automated CNB result led the patient to act quickly on the diagnosis of breast cancer. The false-negative rate of the present study was 3.7% (1/27), which is comparable to those of US-guided automated CNB (mean, 2.8%; range, 0.3-8.2%) and MG-guided wire localization excision (mean, 2%; range, 0-8%) (1).
Breast microcalcifications are observed on sonography as distinct echogenic dots without posterior acoustic shadowing and are more readily identified when associated with a hypoechoic mass or duct-like structures than when no associated sonographic abnormality is present (1, 7). In the present study, 31 of 33 microcalcifications visible on sonography were associated with a mass or nonmass lesions on sonography. The remaining two lesions of isolated calcifications on sonography were retrieved successfully and accurately diagnosed. Although the number of cases was too small to deduce a conclusive inference, it could be suggested that isolated calcifications without associated lesions could be successfully retrieved using 14-G semi-automated CNB in the era of high-resolution sonography.
This study has some limitations. First, the number of enrolled cases in this study was small, which may have limited a conclusive inference. Second, all procedures were performed by one experienced breast radiologist who had used 14-G semi-automated CNB for many years. The proficiency of 14-G semi-automated CNB can affect the retrieval rate of microcalcifications. Third, US-guided 14-G semi-automated CNB was not applicable to all suspicious microcalcifications; only 24% of microcalcifications were considered amenable in the current study, similar to the findings of other studies (1, 5, 9). Nevertheless, in selected cases, US-guided semi-automated 14-G CNB can provide a reliable and cost-effective diagnosis of suspicious microcalcifications. Last, we did not deploy marker clips after US-guided biopsy because they are not generally used in Korea.
In conclusion, US-guided 14-G semi-automated CNB provided a retrieval rate and diagnostic accuracy of 90.9% with a DCIS underestimate rate of 13%. Thus, this could be useful procedure for suspicious isolated microcalcifications apparent on sonography.
Figures and Tables
Fig. 1
US-guided 14-G semi-automated core needle biopsy results and pathologic diagnosis of microcalcifications.
*Magnification mammography, †Microcalcifications. DCIS = ductal carcinoma in situ, IDC = invasive ductal carcinoma, US = ultrasound, ADH = atypical ductal hyperplasia, DIN = ductal intraepithelial neoplasia, CCH = columnar cell hyperplasia, FCC = fibrocystic changes
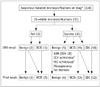
Fig. 2
Details from case of 54-year-old asymptomatic woman.
A. Mammography shows clustered fine pleomorphic calcifications (arrows). BI-RADS assessment is category 5. B. Targeted US shows multiple echogenic dots (arrows) within irregular indistinct isoechoic mass. C. Specimen radiography after US-guided 14-G semi-automated CNB shows multiple microcalcifications (arrows) in five of six cores retrieved. Pathology results of both CNB and final surgery were DCIS. BI-RADS = Breast Imaging-Reporting and Data System, US = ultrasound, CNB = core needle biopsy, DCIS = ductal carcinoma in situ

Fig. 3
Details from case of 42-year-old asymptomatic woman.
A. Magnification mammography shows compactly clustered fine linear and fine pleomorphic calcifications (arrows). BI-RADS assessment is category 5. B. Targeted US shows multiple microcalcifications (arrows) within oval partially indistinct hypoechoic mass. C. Specimen radiography shows 69 microcalcifications in five (arrows) of six cores retrieved. Pathology result of CNB was columnar cell hyperplasia with microcalcifications and that of mammography-guided localization and surgical excision was fibrocystic change with microcalcifications. BI-RADS = Breast Imaging-Reporting and Data System, US = ultrasound, CNB = core needle biopsy

References
1. Soo MS, Baker JA, Rosen EL. Sonographic detection and sonographically guided biopsy of breast microcalcifications. AJR Am J Roentgenol. 2003; 180:941–948.
2. Liberman L. Percutaneous imaging-guided core breast biopsy: state of the art at the millennium. AJR Am J Roentgenol. 2000; 174:1191–1199.
3. Philpotts LE, Hooley RJ, Lee CH. Comparison of automated versus vacuum-assisted biopsy methods for sonographically guided core biopsy of the breast. AJR Am J Roentgenol. 2003; 180:347–351.
4. Youk JH, Kim EK, Kim MJ, Lee JY, Oh KK. Missed breast cancers at US-guided core needle biopsy: how to reduce them. Radiographics. 2007; 27:79–94.
5. Kim YM, Park HB, Ryu JW. Usefulness of ultrasound-guided mammotome biopsy for microcalcification. J Korean Radiol Soc. 2005; 53:129–135.
6. Cho N, Moon WK. Digital mammography-guided skin marking for sonographically guided biopsy of suspicious microcalcifications. AJR Am J Roentgenol. 2009; 192:W132–W136.
7. Moon WK, Im JG, Koh YH, Noh DY, Park IA. US of mammographically detected clustered microcalcifications. Radiology. 2000; 217:849–854.
8. Teh WL, Wilson AR, Evans AJ, Burrell H, Pinder SE, Ellis IO. Ultrasound guided core biopsy of suspicious mammographic calcifications using high frequency and power Doppler ultrasound. Clin Radiol. 2000; 55:390–394.
9. Ciatto S, Houssami N, Ambrogetti D, Bianchi S, Bonardi R, Brancato B, et al. Accuracy and underestimation of malignancy of breast core needle biopsy: the Florence experience of over 4000 consecutive biopsies. Breast Cancer Res Treat. 2007; 101:291–297.
10. Kim HS, Kim MJ, Kim EK, Kwak JY, Son EJ, Oh KK. US-guided vacuum-assisted biopsy of microcalcifications in breast lesions and long-term follow-up results. Korean J Radiol. 2008; 9:503–509.
11. Cho N, Moon WK, Cha JH, Kim SM, Jang M, Chang JM, et al. Ultrasound-guided vacuum-assisted biopsy of microcalcifications detected at screening mammography. Acta Radiol. 2009; 50:602–609.
12. Hahn SY, Shin JH, Han BK, Ko EY. Sonographically-guided vacuum-assisted biopsy with digital mammography-guided skin marking of suspicious breast microcalcifications: comparison of outcomes with stereotactic biopsy in Asian women. Acta Radiol. 2011; 52:29–34.
13. American College of Radiology BI-RADS Committee. ACR BIRADS breast imaging and reporting data system: breast imaging atlas. 4th ed. Reston: American College of Radiology;2003.
14. Jackman RJ, Burbank F, Parker SH, Evans WP 3rd, Lechner MC, Richardson TR, et al. Stereotactic breast biopsy of nonpalpable lesions: determinants of ductal carcinoma in situ underestimation rates. Radiology. 2001; 218:497–502.
15. Hendrick RE, Parker SH. Principle of stereotactic mammography and quality control. In : Parker SH, Jobe WE, editors. Percutaneous Breast Biopsy. New York: Raven;1993. p. 56–58.
16. Abdsaleh S, Azavedo E, Lindgren PG. Semiautomatic core biopsy. A modified biopsy technique in breast diseases. Acta Radiol. 2003; 44:47–51.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download