Abstract
Objective
To demonstrate a variety of MR imaging findings of orbital inflammatory pseudotumors with extraorbital extension.
Materials and Methods
We retrospectively reviewed the MR features of five patients, who were diagnosed clinically and radiologically as having an orbital inflammatory pseudotumor with extraorbital extension.
Results
The types of orbital pseudotumors were a mass in the orbital apex (n = 3), diffuse form (n = 2), and myositis (n = 1). The extraorbital extension of the orbital pseudotumor passed through the superior orbital fissure in all cases, through the inferior orbital fissure in two cases, and through the optic canal in one case. The orbital lesions extended into the following areas: the cavernous sinus (n = 4), the middle cranial fossa (n = 4), Meckel's cave (n = 2), the petrous apex (n = 2), the clivus (n = 2), the pterygopalatine fossa and infratemporal fossa (n = 2), the foramen rotundum (n = 1), the paranasal sinus (n = 1), and the infraorbital foramen (n = 1). On MR imaging, the lesions appeared as an isosignal intensity with gray matter on the T1-weighted images, as a low signal intensity on the T2-weighted images and showed a marked enhancement on the post-gadolinium-diethylene triamine pentaacetic acid (post-Gd-DTPA) T1-sequences. The symptoms of all of the patients improved when they were given high doses of steroids. Three of the five patients experienced a recurrence.
An idiopathic orbital inflammatory pseudotumor represents a nongranulomatous inflammatory process in the orbit or the eye with no known local or systemic cause. It is diagnosed by exclusion, based on the patient's history, clinical course, the response to steroid therapy, laboratory tests and, in a limited number of cases, a biopsy. The extension of the lesion beyond the orbit or even intracranially is quite rare. Such an extension consists of a nonspecific inflammatory tissue of the orbit that extends through one or more foramina into the adjacent extraorbital or intracranial structures. The extension commonly develops through the superior orbital fissure into the middle cranial fossa and the cavernous sinus (1, 2).
We report on the clinical features and the MR imaging findings of five cases of these unusual orbital inflammatory pseudotumors with extraorbital extension.
This study was conducted as a retrospective review of the clinical and MR features of five patients (four men and one woman), who were diagnosed clinically and radiologically as having an orbital inflammatory pseudotumor with an extraorbital or intracranial extension. Their ages ranged from 32 to 63 years (mean, 50.8 years).
An orbit MRI was performed on all patients using a 0.5T, 1.0T or 1.5T super-conducting system. Spin-echo T1-weighted images (TR/TE, 400-500/13-15 msec) and T2-weighted images (TR/TE, 3500-4000/90-100 msec) in the axial and coronal planes were obtained from all patients. The images were acquired with a section thickness of 3-5 mm, a matrix of 256×256, and a field of view of 20-22 cm. All of the patients underwent T1-weighted axial and coronal imaging after the IV administration of Gd-DTPA. Spin-echo T1-weighted images with fat suppression, prior to and after the administration of Gd-DTPA, were obtained from three patients. Two patients underwent an orbit CT examination. Three patients underwent repeated MRI due to recurrence. A biopsy was performed on two patients, namely a needle biopsy in one case and an open biopsy in the other. In this study, we evaluated the findings of the orbital inflammatory pseudotumors with their extraorbital extensions with regard to the location of the lesion, the MR signal intensity and the CT density of the lesion, as well as the degree of contrast enhancement.
Table 1 summarizes the clinical and neuroimaging characteristics of the five patients. Four of the five patients had a unilateral orbital inflammatory pseudotumor, while the remaining patient had a bilateral lesion. The types of orbital pseudotumors were a mass in the orbital apex (n = 3), a diffuse form (n = 2), and a myositis (n = 1). All of the patients had a variety of symptoms, such as decreased visual acuity (n = 4), diplopia (n = 4), proptosis (n = 3), ocular or facial pain (n = 3), and a headache (n = 1).
All of the patients experienced a chronic onset. An intracranial extension of the orbital pseudotumor through the superior orbital fissure was found in all cases (Fig. 1). The extension was observed through the inferior orbital fissure in two patients (Fig. 2), and through the optic canal in one case. The orbital lesions extended into the cavernous sinuses with a mass lesion being found in four patients, three of whom showed a narrowing and encasement of the cavernous carotid artery (Fig. 3). The extension was also found in the following areas: the middle cranial fossa (n = 4), the pterygopalatine fossa and infratemporal fossa (n = 2), Meckel's cave (n = 2), the petrous apex (n = 2), the clivus (n = 2), the foramen rotundum (n = 1), the paranasal sinus (n = 1), and the infraorbital foramen (n = 1). The lesions appeared as an isosignal intensity with gray matter on the T1-weighted images, a low signal intensity on the T2-weighted images and showed a marked enhancement on the Gd-DTPA T1-weighted images. In all cases, except for one patient with a dominant extension through the inferior orbital fissure, there was a diffuse meningeal enhancement; three of these were also combined with a brain edema. Two patients who underwent CT studies showed an iso-density to the brain parenchyma with strong enhancement.
The pathological findings of the two patients who underwent a biopsy showed chronic inflammatory cells with fibrosis. All of the patients were given high doses of steroids, which resulted in a reduction in the symptoms. Three of the five patients experienced a recurrence.
A pseudotumor of the orbit is a clinical and pathologic condition involving an idiopathic inflammation of the orbital contents that is not related to an infection, neoplasm, or systemic disease (1, 3, 4). The term orbital pseudotumor was originally intended to include all nonneoplastic disorders, but is now limited to those lesions that are idiopathic in nature (1, 2). The incidence of orbital pseudotumors has been reported to be 9% of all orbital mass lesions. They are most often confined to the orbit and frequently involve the lacrimal gland and the muscular cone (5).
The symptoms of idiopathic pseudotumors reflect the degree of the inflammatory response (acute, subacute, or chronic) and the location of the inflammatory tissue. In the chronic sclerosing form that evolves over weeks and months, the signs of fixation of the orbital structures and the mass effect are more prominent. This is associated with slowly progressive visual loss, diplopia and proptosis. A pseudotumor in acute form is more responsive to high doses of systemically administered prednisone than a chronic lesion. The complete resolution of the inflammation may ensue, although a recurrence may occur in the same or other orbit (1, 4).
Pathologically, orbital pseudotumors show a nonspecific infiltration of inflammatory cells composed of lymphocytes, plasma cells, neutrophils, and macrophages. Varying degrees of fibrosis may be observed depending on the chronicity of the disease (2, 3).
The disease can be categorized according to which orbital structure is predominantly involved. Myositis (one or more extraocular muscles), dacryoadenitis (lacrimal gland), periscleritis including Tenon's space, trochleitis, perineuritis (outer dural sheath of the optic nerve and adjacent fat) and the diffuse form can be distinguished according to their location. The inflammatory process within the orbital fat may be localized, and this process can simulate a tumor or may be diffuse within the fatty tissue. The involvement of the lacrimal gland and muscle cone is particularly common (4, 6).
Three major openings are observed in the posterior orbit. The first is the superior orbital fissure that communicates with the middle cranial fossa. The second is the medial to superior orbital fissure which constitutes the optic canal, and which is separated by the optic strut. The third is the inferior orbital fissure which connects the orbit with the infratemporal and pterygopalatine fossae (7).
An idiopathic orbital pseudotumor is commonly restricted to the orbit. However, an extension beyond the orbit can occur in cases of extensive and chronic orbital inflammation (1). The middle cranial fossa and cavernous sinus are the two most common locations into which extensions are observed. A direct intracranial spread can occur through the superior orbital fissure, the inferior orbital fissure or the optic canal. An extension of the lesion into the pterygopalatine and infratemporal fossae probably reflects a chronic inflammatory lesion extending through the inferior orbital fissure (1, 2, 8).
Clifton et al. (8) reported direct evidence of an intracranial extension through the superior orbital fissure, with the following patterns being identified: i) abnormal soft tissue extending through and obliterating the normal fatty plane at the superior orbital fissure into the middle cranial fossa; ii) an expansion of the ipsilateral cavernous sinus; and iii) an abnormal thickening and/or enhancement of the meninges more distantly, in continuity with the orbital lesion. The spread of the lesion into the adjacent paranasal sinuses, although rare, is well documented. Ayala et al. (9) reported that a chronic orbital pseudotumor slowly progressed to the anterior cranial fossa and that the pathway for the extension from the orbit into the anterior cranial fossa could be the anterior ethmoid foramen for the anterior ethmoidal artery. When a pseudotumor invades the cavernous sinus, the process is usually considered to be part of Tolosa-Hunt syndrome (10-12).
An analysis of our five cases showed that the two most common locations of the extension were the middle cranial fossa and the cavernous sinus. An extension through the superior orbital fissure occurred in all cases, through the inferior orbital fissure in two cases and through the optic canal in one case. All cases had a chronic onset with extensive fibrosis, and three patients experienced a recurrence. We thought that these factors would lead to an extraorbital extension of the orbital pseutotumor.
The radiological findings in a pseudotumor are characterized by inflammatory changes in the various intraorbital structures, such as the globe, the lacrimal glands, the extraocular muscles, the orbital fat and the optic nerve. The CT findings do not allow idiopathic orbital inflammation to be unequivocally distinguished from other orbital mass lesions. They usually show an abnormal intraorbital soft tissue mass density, which varies considerably in size, shape, and location. A bony change reflected by a hyperostosis and a remodeling favors the diagnosis of a long-standing benign process, such as a pseudotumor that is sometimes found to extend through the superior orbital fissure and to enlarge and erode the fissure as compared to the normal side. MRI shows a hypointense lesion on the T1- and T2-weighted images (possibly reflecting the fibrotic changes), and shows marked gadolinium enhancement. Fat suppression techniques clearly show an optic nerve sheath lesion and intraorbital inflammation (1, 2, 4, 6, 9).
A prompt response to steroid treatment, in conjunction with the radiological findings, supports the diagnosis of a pseudotumor. However, the diagnosis may be more difficult in the subacute and chronic forms. Sometimes, a chronic idiopathic inflammatory pseudotumor can simulate lymphoma, particularly when there is no history of an acute onset (1, 2). A trial of steroids may cause the mass to shrink and eliminate the need for an orbital biopsy or surgery.
The differential diagnosis is extensive. It consists of infection (bacterial, tuberculosis, fungal, viral), lipogranuloma, fibrous dysplasia, histiocytosis, fibrous histiocytosis, fibromatosis, fibrosarcoma, periosteal fasciitis, nodular fasciitis, amyloidosis, Wegener's granulomatosis, lethal midline granuloma, polyarteritis nodosa, sarcoidosis, and lymphoma (2).
The method of treating an idiopathic orbital inflammation varies. Initial treatment is with high-dose corticosteroids, but this is not always effective. Surgery with a biopsy is indicated when there is no response to the steroid regimen, in order to rule out a neoplasm and to decompress the vital structures. However, this usually does not cure the lesion. Radiotherapy should be used when there is no preponderance of fibrotic tissue, if there is no improvement after the steroid therapy and if the symptoms progress (2, 4).
In conclusion, an intraorbital pseudotumor with extensive and chronic inflammation can extend into the extraorbital location, possibly inducing more serious and widespread clinical symptoms. Although invasive orbital pseudotumors are uncommon, a pseudotumor should be considered in the differential diagnosis of orbital masses that extend beyond the confines of the bony orbit. Prompt recognition of these rare findings of an orbital pseudotumor assists in the choice of appropriate therapy and eliminates the need for unwarranted biopsy or surgery.
Figures and Tables
Fig. 1
Case 1. A 58-year-old man with diplopia and trigeminal neuralgia.
A. An initial MR image with fat suppressed postcontrast coronal T1-weighted images shows increased thickness of the left rectus muscles with dense contrast enhancement, combined with a soft tissue mass in the superomedial aspect of the extra-conal space. A mild infiltration into the left orbital fat is also noted. The symptoms improved after steroid treatment.
B-D. Follow-up MR images obtained after five months.
Postcontrast T1-weighted images with fat suppression show a recurrence. Diffuse infiltrating enhancement in the left orbital fossa and apex is seen along ith an increase in the thickness of the rectus muscles; this extends posteriorly through the superior orbital fissure into the left cavernous sinus and adjacent temporal pachymeninges (arrows).

Fig. 2
Case 2. A 63-year-old man with bilateral proptosis.
A. Orbital CT with bone setting shows a widening of the bilateral pterygopalatine fossae (white arrows) and the infraorbital foramina (small arrows).
B, C. T1-weighted images with fat suppression show diffuse, ill-defined infiltration into the bilateral orbital fossae with involvement of the lacrimal glands and the rectus muscles. The lesions extend into the bilateral pterygopalatine and infratemporal fossae (white arrows), and infraorbital foramina (black arrows).
D. T2-weighted image demonstrates that the lesions show low signal intensity. The orbital lesions extend posteriorly through the inferior orbital fissures (arrows).
E, F. Postcontrast T1-weighted images reveal marked enhancement.

Fig. 3
Case 5. A 46-year-old man with a right proptosis and diplopia.
A, B. Axial T1-weighted image (A) and T2-weighted image (B) reveal a low signal mass in the right orbital apex extending into the cavernous sinus and middle cranial fossa. Marked narrowing and encasement of the cavernous carotid artery is seen.
C. Postcontrast T1-weighted image shows that the lesions are markedly enhanced. Diffuse meningeal thickening with marked enhancement is also noted. Ipsilateral medial and lateral rectus muscles are slightly thickened with some infiltration into the orbital fossa.
D, E. One year later, the follow-up T2-weighted image (D) and postcontrast T1-weighted image (E) show new lesions in the left temporalis muscle (arrows), left orbital fossa and left preorbital space. The lesions show a low signal intensity on the T2-weighted image with strong enhancement.
F. One year later, the follow-up T2-weighted image shows newly developed low signal lesions in the bilateral orbital fossae, orbital apices and the bilateral cavernous sinuses.
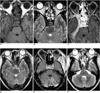
Table 1
The Clinical and Neuroimaging Characteristics of the Six Patients

Note.-VA = visual acuity, OA = orbital apex, SOF = superior orbital fissure, IOF = inferior orbital fissure, OC = optic canal, CS = cavernous sinus, MCF = middle cranial fossa, PPF = pterygopalatine fossa, ITF = infratemporal fossa, PNS = paranasal sinus, PA = petrous apex, MC = Meckel's cave, F = foramen, Y = yes, N = no, ++ = moderate enhancement, +++ = strong enhancement, NA = not available
References
1. Bencherif B, Zouaoui A, Chedid G, Kujas M, Van Effenterre R, Marsault C. Intracranial extension of an idiopathic orbital inflammatory pseudotumor. AJNR Am J Neuroradiol. 1993. 14:181–184.
2. De Jesus O, Inserni JA, Gonzalez A, Colon LE. Idiopathic orbital inflammation with intracranial extension. J Neurosurg. 1996. 85:510–513.
3. Frohman LP, Kupersmith MJ, Lang J, Reede D, Bergeron RT, Aleksic S, et al. Intracranial extension and bone destruction in orbital pseudotumor. Arch Ophthalmol. 1986. 104:380–384.
4. Weber AL, Romo LV, Sabates NR. Pseudotumor of the orbit. Clinical, pathologic, and radiologic evaluation. Radiol Clin North Am. 1999. 37:151–168.
5. Noble SC, Chandler WF, Lloyd RV. Intracranial extension of orbital pseudotumor: a case report. Neurosurgery. 1986. 18:798–801.
6. Kaye AH, Hahn JF, Craciun A, Hanson M, Berlin AJ, Tubbs RR. Intracranial extension of inflammatory pseudotumor of the orbit. J Neurosurg. 1984. 60:625–629.
7. Som PM, Curtin HD. Head and neck imaging. 2003. 4th ed. St Louis: Mosby;329–330.
8. Clifton AG, Borgstein RL, Moseley IF, Kendall BE, Shaw PJ. Intracranial extension of orbital pseudotumor. Clin Radiol. 1992. 45:23–26.
9. Ayala AS, Fernandez Sarabia T, Cabeza Martinez B, Moya MJ, Menendez FL, Garcia PZ. Orbital pseudotumor with intracranial extension. Eur Radiol. 2000. 10:1505.
10. Desai SP, Carter J, Jinkins JR. Contrast-enhanced MR imaging of Tolosa-Hunt syndrome : A case report. AJNR Am J Neuroradiol. 1991. 12:182–183.
11. Goto Y, Hosokawa S, Goto I, Hirakata R, Hasuo K. Abnormality in the cavernous sinus in three patients with Tolosa-Hunt syndrome : MRI and CT findings. J Neurol Neurosurg Psychiatry. 1990. 53:231–234.
12. De Arcaya AA, Cerezal L, Canga A, Polo JM, Berciano J, Pascual J. Neuroimaging diagnosis of Tolosa-Hunt syndrome MRI contribution. Headache. 1999. 39:321–325.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download