Abstract
Renal hemangioma is an uncommon benign tumor which usually causes painless or painful gross hematuria. Its preoperative diagnosis is extremely difficult or even impossible.
We experienced three cases of renal hemangioma, located mainly at the pelvocalyceal junction or in the inner medulla. US demonstrated variable echogenecity, and CT revealed a lack of significant enhancement. Where there is gross hematuria in a young adult, especially when the renal mass located in the pelvocalyceal junction or inner medulla shows little enhancement on CT, renal hemangioma should form part of the differential diagnosis.
Hemangioma is a rare tumor found in the urinary tract. Though it may occur in any part of the tract, the kidney is most frequently affected, followed by the urinary bladder, ureters, and urethra (1-4). It is one of the benign causes of hematuria in young adults. Diagnosis is often difficult and preoperative diagnosis is rare (5-7). An understanding of the radiological findings of this rare entity may, however, facilitate its preoperative diagnosis, which may require limited renal resection (8, 9). We report the radiologic findings of three cases of renal hemangioma, including those of US and CT scans.
A 31-year-old man presented with colicky abdominal pain and gross hematuria. He complained of frequency, dysuria, and a residual urine sensation after voiding. Excretory urography (IVU) showed smooth extrinsic indentation in the lower pole calyx. Ultrasonography revealed a well-defined echogenic mass containing multiple anechoic areas in the inferior pole of the right kidney (Fig. 1). Selective renal angiography showed avascularity of the mass and displacement of the interlobar and segmental arteries. Radical nephrectomy was performed. The mass was spongy-like and consisted of multiple blood-filled spaces; microscopic examination showed it was located in the inner medulla. The pathologic findings were consistent with cavernous hemangioma (Table 1).
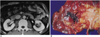
A 43-year-old man presented with gross hematuria and pain in the left flank. US demonstrated a 1.5-cm-sized mass in the pelvis of the left kidney, which was isoechoic to renal cortex (Fig. 2A). There was also an echogenic blood clot in the urinary bladder. Enhanced CT scan showed a lobulated, low attenuated mass adjacent to the renal pelvis (Fig. 2B). The renal mass, the density of which was 35.2 and 44.4 Hounsfield units on unenhaned- and enhanced CT scans, respectively, did not show significant enhancement. Because of the possibility of malignancy, a left nephrectomy was performed. On patholgic examination revealed multiple vascular channels of variable size beneath the pelvic mucosa. The pathologic diagnosis was cavernous hemangioma.
A 43-year-old man presented with left lower abdominal pain which had lasted for one month. He had a history of renal tuberculosis and a left ureteral stone. Physical examination was unremarkable. US showed a mass, about 2 cm in size and slightly hyperechoic to renal cortex, in the lower pole of the left kidney. It had poor margin. Unehanced CT scan showed a lobulated mass with higher attenuation than the renal parenchyma; after the intravenous administration of contrast material, the mass did not show significant enhancement (Fig. 3A). Renal cell carcinoma was diagnosed, and the patient was referred for left nephrectomy. Pathologic analysis of the specimen showed a hemorrhagic lesion in the corticome-dullary junction of the lower pole (Fig. 3B). Microscopical-ly, the hemorrhagic area was seen to composed of capillary-sized vessels, and there was no evidence of malignancy.
Although renal hemangioma can be found in any part of the kidney, the most frequent location is the tip of the papilla. The submucosal region, the papilla, and the medulla account for 90% of anatomic locations, and the renal parenchyma and capsule the rest (2, 5-7).
Renal hemangiomas are usually solitary and unilateral, without significant side or sex predilection, but in 12% of the cases are multiple. Hemangiomas of the urinary tract are generally considered to be an isolated disease, but may be associated with tuberous sclerosis, Sturge-Weber syndrome, and Klippel-Trenaunay-Weber syndrome. The size of a renal hemangioma ranges from 1-2 cm in diameter to as large as the kidney itself (1-5, 7, 9).
Clinical symptoms including colicky painful or painless intermittent hematuria frequently appear in the third or fourth decade (1-5). In our cases, painful hematuria was encountered in two patients and flank and abdominal pain in all three.
Because there are no specific clinical or radiological findings for the tumors, renal hemangiomas are often missed. It is impossible to detect them on IVU unless they are large enough to produce calyceal deformity or a filling defect. Their angiographic appearance varies and may be as hypervascular, hypovascular, or normal.
The US findings of renal hemangiomas are similar to those of liver hemangiomas, which on ultrasound is often echogenic (2). A hypoechoic rim, intratumoral cysts, and the absence of acoustic shadowing are important findings that may help distingish renal cell carcinoma from angiomyolipoma (10, 11). In our cases, the mass was hyperechoic in two patients, and isoechoic to renal parenchyma in the other. In one of two patients with hyperechoic hemangioma, the mass contained anechoic areas in the center, corresponding to blood-filled spaces (Fig. 1). There was no visible hypoechoic rim or posterior shadowing. In contrast to angiomyolipoma, the echogenecity of which is in most cases equal to that of renal sinus (11), the echogenecity of hyperechoic hemangiomas was less than that of renal sinus. As most renal hemangiomas are located in the renal pelvis or at the medullary junction, the possibility of a renal pelvic tumor such as transitional cell carcinoma should be considered (12). The US findings are nonspeficic, and may mimick more common tumors of the kidney, including renal cell carcinoma and transitional cell carcinoma.
There are few descriptions of the CT findings of renal hemangioma. The tumor may enhance on injection of intravenous contrast material, but are not usually encapsulated (2). In two of our cases, however, the lesion was not significantly enhanced. The reason for this is not clear, but it might be due to intratumoral hemorrhaging of the mass.
Therapeutic measures for renal cavernous hemangioma range from no therapy to total nephrectomy (2, 5, 8). Management includes observation, nephrectomy, heminephrectomy, papillectomy and embolization. In a healthy patient with mild to moderate hematuria who is clinically and radiographically well, observation is not contraindicated. Renal hemangioma is seldom diagnosed preoperatively, and it is therefore impossible to recommend specific treatment (4). Generally, surgery is considered when the tumor causes symptoms such as life-threatening hemorrhage, or when it is difficult to distinguish the lesion from a disease such as carcinoma which requires nephrectomy. Hemi- or total nephrectomy is the procedure of choice (1, 4, 7), and radiation therapy and transarterial embolization are sometimes employed (1, 4, 6, 11).
In conclusion, the definitive preoperative diagnosis of renal hemangiomas is very difficult, and in order to establish this, operative proof is required. Renal hemangioma should, however, be included in the differential diagnosis, especially when CT scanning reveals little enhancement of a the renal mass located at the pelvocalyceal junction or in the inner medulla.
Figures and Tables
Fig. 1
Renal hemangioma in a 31-years-old man.
Longitudinal US shows a well-defined round echogenic mass lesion (arrows) containing multiple anechoic areas in the lower pole of the right kidney.

Fig. 2
Renal hemangima in a 31-years-old man.
A. US shows a 1.5 cm-sized mass (arrow) in the pelvis of the left kidney, which is isoechoic to renal parenchyma.
B. Enhanced CT scan shows a non-enhancing, low attenuated mass with lobulated margin (arrows) adjacent to the pelvis.

Fig. 3
Renal hemangioma in a 31-years-old man.
A. Enhanced CT scan shows a non-enhancing mass with lobulated margin in the lower pole of the left kidney. Unenhanced CT scan shows a high-attenuated mass suggesting hemorrhage (not shown).
B. Gross pathologic specimen shows a hemorrhagic lesion (arrows) at the corticomedullary junction of the lower pole.
References
1. Motley RC, Patterson DE, Weiland LH. Ureteroscopic visualization of a cavernous hemangioma of the renal pelvis. J Urol. 1990; 143:788–790.
2. Numan F, Berkmen T, Korman U, et al. Cavernous hemangioma of the kidney: case report. Clin Imaging. 1993; 17:106–108.
3. Yazaki T, Takahashi S, Ogawa Y, et al. Large renal hemangioma necessitating nephrectomy. Urology. 1985; 25:302–304.
4. Jahn H, Nissen HM. Haemangioma of the urinary tract: review of the literature. Br J Urol. 1991; 68:113–117.
5. Wang T, Palazzo JP, Mitchell D, et al. Renal capsular hemangioma. J Urol. 1993; 149:1122–1123.
6. Gordon R, Rosenmann E, Barzilay B, et al. Correlation of selective angiography and pathology in cavernous hemangioma of the kidney. J Urol. 1976; 115:608–609.
7. Petrson NE, Thompson HT. Renal hemangioma. J Urol. 1971; 105:27–31.
8. Stanley RJ, Cubillo E, Mancillajimensez R, et al. Cavernous hemangioma of the kidneys. AJR. 1975; 125:682–687.
9. Ekelund L, Gothlin J. Renal hemangiomas. An analysis of 13 cases diagnosed by angiography. AJR. 1975; 125:788–794.
10. Yamashita Y, Ueno S, Makita O, et al. Hyperechoic renal tumors: anechoic rim and intratumoral cysts in US differentiation of renal cell carcinoma from angiomyolipoma. Radiology. 1993; 188:179–182.
11. Siegel CL, Middleton AD, Teefey SA, et al. Angiomyolipoma and renal cell carcinoma: US differentiation. Radiology. 1996; 198:789–793.
12. Mittelstaedt CA. Mittelstaedt CA, editor. Kidney. General Ultrasound. 1992. New York: Churchill Livingstone;p. 947–951.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download