Abstract
A 59-year-old man with a known central hepatocellular carcinoma (HCC) underwent a trans-arterial-chemo-embolization (TACE) and a post-TACE percutaneous radiofrequency ablation (PRFA). Two months after the PRFA, the patient presented jaundice and an abdominal computed tomography was obtained. An arterial enhancing mass adjacent to the ablated necrotic lesion with a continuously coexisting mass inside the right hepatic duct, suggestive of a HCC recurrence with a direct extension to the biliary tract was found. Finally a biliary tumor obstruction has been developed and a percutaneous transhepatic biliary drainage was performed. This case of biliary obstruction caused by directly invaded recurred HCC after PRFA will be reported because of its rare occurence.
The percutaneous radiofrequency ablation (PRFA) is the primary treatment for hepatocellular carcinoma (HCC) recently. Although PRFA is a relatively safe procedure, a biliary obstruction can be caused as rare complication. More than extreme rare is the biliary obstruction caused by a biliary HCC or tumor cast after a PRFA. A known HCC patient presented with a liver parenchymal and intra-biliary mass following the radiofrequency ablation of the necrotic lesion. We assume that the extended biliary tumor from the recurred HCC may be the result of a minimal bile duct injury after the thermal ablation.
A 59-year-old man with a known HCC, centrally located between S4 and S8 caused by liver cirrhosis with chronic hepatitis B visited our hospital via the emergency room and was admitted on 26. November 2012 because of progressive jaundice and abdominal pain. In spite of several times of trans-arterial-chemo-embolization (TACE), the HCC recurred three times and was treated with TACE and a consecutive thermal PRFA 2 months prior to the actual episode. In the laboratory analysis a serum level of total bilirubin was shown with 5.57 mg/L with a normal range 0.2-1.2 mg/dL and the direct bilirubin serum level was 4.6 mg/dL with a normal range of 0-0.5 mg/dL. Other abnormal laboratory data included: alkaline phosphatase, 709 IU/L (57-230); ç-glutamyl transferase, 1392 IU/L (8-70); glutamic oxaloacetic transaminase, 259 IU/L (5-35); glutamic pyruvic transaminase, 374 IU/L (5-35). Protein induced by vitamin K absence (PIVKA) and alpha-fetoprotein level were within normal ranges.
In the emergently obtained contrast enhanced abdominal CT was noted an early enhancing mass adjacent to the previously ablated necrotic lesion (Fig. 1A, B) with a continuous extension into the right hepatic duct and the common hepatic duct (CHD) (Fig. 1C). Dilatation of biliary duct was not prominent but a portal vein thrombosis was developed (Fig. 1C). Although the portal and as well the delayed phase of the CT revealed no definite washout of the contrast enhancement from the mass, an invasion of the recurrent HCC into the biliary tree was assumed. An abdominal laboratory serum analysis was performed 1 month later and the serum levels of total and direct bilirubin were marked as elevated (26.84 mg/dL and 23.27 mg/dL). The serum PIVKA level was 108 mAU/mL with a normal range between 0-40 mAU/mL. Two weeks later, the serum levels of total and direct bilirubin level were elevated up to 32.53 mg/dL and 26.14 mg/dL respectively and a follow-up abdominal CT was performed. The abdominal CT demonstrated the previously enhancing mass increased in size (Fig. 2A) and it was also noted an extent of intra-biliary growth, an increased size of portal vein thrombosis and a diffuse dilatation of the intra-hepatic and extra-hepatic bile ducts (Fig. 2B).
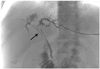
A left sided percutaneous trans-biliary drainage (PTBD) was performed immediately because the jaundice was considered as induced by the biliary tumor obstruction. This procedure resulted in a markedly dilatation improvement of the hepatic ducts as well as in decreased serum levels of bilirubin. Twenty days after PTBD, the percutaneous transhepatic cholangiography showed an intra-biliary mass with a markedly extension to CBD without duct dilatation (Fig. 3). Because of the better patients' condition, a radiation therapy was possible. The follow-up abdominal CT after the radiation therapy showed a complete disappearance of central and intra-biliary mass and a reduced size of portal vein thrombosis.
Jaundice presents in 19% to 40% of patients with HCC at the time of diagnosis and occurs in later stages usually (1). However, HCC causes obstructive jaundice by intra-ductal invasion of bile duct or extrinsic compression of hepatic hilum in rare cases. This type of HCC is also known as "icteric type HCC (IHCC)" and is often accompanied by biliary colic (2). Causes of obstructive jaundice in this type of HCC include an intra-luminal growth of tumor leading to an obstruction of intra or extra-hepatic ducts, tumor tissue fragments and/or hemorrhages or blood clots due to necrosis, bleeding and detachment of intra-ductal tumors, giving rise to the obstruction. This causes are similar to the reported findings in IHCC (3). Several studies have reported about an intraductal HCC without an obvious intrahepatic tumor (4, 5). HCC invades the biliary systems through one of the following three mechanisms: 1) the tumor may grow continuously in a distal fashion, filling the entire extrahepatic biliary system with a solid cast of tumor; 2) a fragment of necrotic tumor may separate from the proximal intraductal growth, migrating to the distal common bile duct and causing obstruction; or 3) a hemorrhage from the tumor may partially or completely fill the biliary tree with blood clots (6).
PRFA has been accepted as a safe technique for the HCC treatment. But the heat from the radio-frequency energy may produce a nonspecific thermal injury to the tumor tissue as well as to the adjacent normal structures including the bile duct (7). The patient in the presented report got a progressive jaundice with prior trans-arterial embolization and PRFA for centrally located HCC. An early enhancing mass was placed adjacent the thermal necrotic lesion with a continuous extension through the right hepatic duct and CHD was shown in the abdominal CT. Although no pathologic confirmation was done, a recurred HCC was presumed because of the enhancement of the arterial phase in the dynamic CT and a significant elevation of the tumor marker serum level. Findings of the following CT were a more increased size of the central mass with a progression of intra-biliary tumor growth. This findings supported our assumption it may be possible that the recurred HCC directly extend into the hepatic biliary duct through a bile injury which was caused by PRFA.
To the best of our knowledge, a biliary obstruction caused by intra-biliary tumor growth after PRFA is extremely rare. It has been assumed that the microscopic injury caused by thermal ablation supported the easy invasion of the recurred HCC into the biliary tract. Sasahira et al. (8) reported that extra-biliary obstructions after percutaneous ablation were rare and major causes of extra-hepatic biliary obstruction after percutaneous thermal ablation such as biliary casts, haemobilia and common bile duct stones.
In the most literatures it was reported the PTBD offers a significant palliation for patients with benign or malignant biliary obstruction with a low morbidity and mortality. But Kubota et al. (9) postulated an ineffectiveness of PTBD in HCC because of the underlying hepatic dysfunction due to liver cirrhosis and diffuse tumor infiltration. However, other reports argued a effectiveness of PTBD in 59.1% of IHCC, regardless of the Child classification of patients (2). In our case, the serum level of bilirubin was decreased after the PTBD performance and the condition of the patient was improved. He got a radiation therapy finally.
In conclusion, we experienced a biliary obstruction caused by a direct intra-biliary growth from recurred HCC after PRFA. A physician performing PRFA of HCC should consider the biliary complication of an ablation, especially if a mass abuts a major bile duct or is centrally located.
Figures and Tables
Fig. 1
Transverse CT scans in 60-year-old man with prior trans-arterial embolization and radiofrequency ablation due to central located hepatocellular carcinoma.
A. Arterial phase scan shows lipiodol uptake lesions is located in the ablation necrosis which is central portion of the liver.
B. The same CT scan in hepatic hilum level demonstrates early enhancing mass (black arrow) at the hepatic hilum is abutting upon the right hepatic duct (white arrow). The mass is located just below the necrotic thermal lesion.
C. On portal phase scan, the mass is extending into the common hepatic duct (black arrow) and portal vein thrombus (gray arrow) is also noted.

Fig. 2
Two months after follow-up transverse scans follow of the same patient.
A. Arterial phase scan reveals early enhancing mass (black arrow) at hepatic hilum was increased in size with dilated adjacent right hepatic duct (white arrow).
B. On the same CT scan, the intra-biliary growing of the mass (black arrow) and portal vein thrombosis (gray arrow) are more prominent with biliary dilatation.

References
1. Qin LX, Tang ZY. Hepatocellular carcinoma with obstructive jaundice: diagnosis, treatment and prognosis. World J Gastroenterol. 2003; 9:385–391.
2. Lee JW, Han JK, Kim TK, Choi BI, Park SH, Ko YH, et al. Obstructive jaundice in hepatocellular carcinoma: response after percutaneous transhepatic biliary drainage and prognostic factors. Cardiovasc Intervent Radiol. 2002; 25:176–179.
3. Long XY, Li YX, Wu W, Li L, Cao J. Diagnosis of bile duct hepatocellular carcinoma thrombus without obvious intrahepatic mass. World J Gastroenterol. 2010; 16:4998–5004.
4. Abe T, Kajiyama K, Harimoto N, Gion T, Shirabe K, Nagaie T. Intrahepatic bile duct recurrence of hepatocellular carcinoma without a detectable liver tumor. Int J Surg Case Rep. 2012; 3:275–278.
5. Qin LX, Ma ZC, Wu ZQ, Fan J, Zhou XD, Sun HC, et al. Diagnosis and surgical treatments of hepatocellular carcinoma with tumor thrombosis in bile duct: experience of 34 patients. World J Gastroenterol. 2004; 10:1397–1401.
6. Chen MF, Jan YY, Jeng LB, Hwang TL, Wang CS, Chen SC. Obstructive jaundice secondary to ruptured hepatocellular carcinoma into the common bile duct. Surgical experiences of 20 cases. Cancer. 1994; 73:1335–1134.
7. Rhim H, Yoon KH, Lee JM, Cho Y, Cho JS, Kim SH, et al. Major complications after radio-frequency thermal ablation of hepatic tumors: spectrum of imaging findings. Radiographics. 2003; 23:123–134.
8. Sasahira N, Tada M, Yoshida H, Tateishi R, Shiina S, Hirano K, et al. Extrahepatic biliary obstruction after percutaneous tumour ablation for hepatocellular carcinoma: aetiology and successful treatment with endoscopic papillary balloon dilatation. Gut. 2005; 54:698–702.
9. Kubota Y, Seki T, Kunieda K, Nakahashi Y, Tani K, Nakatani S, et al. Biliary endoprosthesis in bile duct obstruction secondary to hepatocellular carcinoma. Abdom Imaging. 1993; 18:70–75.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download