Abstract
Extramedullary plasmacytoma originating from the bronchus is a very rare condition, and the radiological diagnostic criteria for this disease are not well established due to its rarity. It often appears as a tumor with smooth margins and very rarely invades the surrounding structures. A computed tomography scan and a positron emission tomography/computed tomography scan were performed on a 71-year-old male patient who was admitted for hemoptysis. A solid mass with irregular margins infiltrating the surrounding vasculature and mediastinum was observed, and a presumptive diagnosis of lung cancer was made. However, bronchoscopy with transbronchial biopsy and immunohistochemical staining confirmed the diagnosis of extramedullary plasmacytoma. We herein present a rare case of extramedullary plasmacytoma which mimiked lung cancer.
Extramedullary plasmacytoma is a rare form of plasma cell dyscrasia that arises outside the bone marrow and usually affects the mucus membrane of the upper respiratory tract (1, 2). Extramedullary plasmacytoma originating from the lower bronchus is a very rare condition, and its diagnosis and treatment methods are not well established. Previously published cases of primary pulmonary plasmacytoma usually presented them as a well-defined mass with smooth margins (1, 3, 4). We report a unique case, found in a symptomatic older male patient, with extramedullary plasmacytoma of the lower bronchus, mimicking the lung cancer.
Extramedullary plasmacytoma is a rare form of plasma cell dyscrasia that arises outside the bone marrow and usually affects the mucus membrane of the upper respiratory tract (1, 2). Extramedullary plasmacytoma originating from the lower bronchus is a very rare condition, and its diagnosis and treatment methods are not well established. Previously published cases of primary pulmonary plasmacytoma usually presented them as a well-defined mass with smooth margins (1, 3, 4). We report a unique case, found in a symptomatic older male patient, with extramedullary plasmacytoma of the lower bronchus, mimicking the lung cancer.
A 71-year-old male visited the hospital because of hemoptysis that began 3 days ago. Three days before coming to the hospital, he had coughed up a cup of dark red blood. Subjective symptomatic complaints by the patient upon arrival to the hospital included dyspnea, cough, and sputum. He had lost 5 kilograms in the past one month and complained of continued generalized weakness. He also had diabetes and a 45 pack-year history of smoking, which he quitted five years ago. Initial laboratory values revealed a hemoglobin level of 11.5 g/dL and C-reactive protein of 3.06 mg/dL. Blood urea nitrogen, creatinine, calcium, inorganic phosphate, aspartate aminotransferase, alanine aminotransferase, and serum electrolyte levels were all within the normal range. Plasma protein was 6.2 g/dL and albumin was 3.0 g/dL.
A chest X-ray showed atelectasis of right middle and lower lobes (Fig. 1). There were no signs of the right side fluid shifting on the right decubitus view. Chest computed tomography scan revealed a mass narrowing lumen of the right main bronchus and obstructing the bronchus intermedius, which caused atelectasis of the right middle lobe and the right lower lobe. This mass, measuring 5.8 × 4.8 × 3.8 cm in dimensions, showed a heterogenous enhancement and an invasion of the posterior segment of the right upper lobe. It further invaded the right main pulmonary artery, left atrium, and the right superior and inferior pulmonary veins. An enlarged metastatic lymph nodes were observed in the right lower paratracheal area and the prevascular space of the mediastinum (Fig. 2). Positron emission tomography/computed tomography (PET/CT) scan revealed an increased fluorodeoxyglucose (FDG) uptake in the mass involving the right upper lobe, which obstructed the right main bronchus and the bronchus intermedius with the maximum standardized uptake value of 6.9. Increased FDG uptakes were also detected in the mediastinal lymph node in torso maximum intensity projection image (Fig. 3).
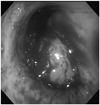
Sputum culture did not reveal any malignant cells, but bronchoscopy showed a mass in the right main bronchus, which obstructed the bronchus intermedius. The mass was round in shape and was oozing (Fig. 4). A bronchoscopic biopsy revealed that the mass was mostly constituted of abnormal mature plasma cells. Immunohistochemistry yielded positive results for lambda light chain but negative results for CD3, CD5, CD10, CD20, and kappa light chain (Fig. 5). Multiple myeloma was ruled out after bone marrow biopsy revealed normocellularity, and no monoclonal gammopathy was observed on the immunoelectrohporesis of plasma and urine. Involvement of the skeletal system was not noticed on a PET/CT scan and bone scan.
Surgical resection of the tumor was not recommended based on the image findings, because of its infiltration into the surrounding structures. After the patient received radiation therapy (total of 5040 cGy), the tumor showed a significant reduction in size on the follow-up imaging study (Fig. 6).
Extramedullary plasmacytoma is a rare tumor which makes up approximately 5% of all patients with plasmacytomas, and are mostly present in the head, the neck, or the upper respiratory tract mucosa (3, 4, 5). It occasionally appears in the gastrointestinal track, thyroid, skin, testis, and lungs (4, 5, 6). Published cases of solitary pulmonary plasmacytoma report the male/female ratio of 1.4:1 to 5:1, but there is no predilection for sex and a median age is over 50 years (1, 4). Although most patients are asymptomatic, some patients complain of dyspnea, fever, cough, sputum, and hemoptysis (2).
Primary pulmonary plasmacytomas often present relatively as homogeneous masses. Their frequent radiologic findings are solitary masses or nodules, and they frequently occur in the perihilar area (1, 2). Infrequently, the lobar consolidation and bilateral reticulonodular opacity (7), diffuse alveolar consolidation (5), or mulitple nodules (2) have also been described (2, 5, 7). Masses are round to ovoid in shape or have well-defined and smooth margins. The size is highly variable, ranging from 1.5 cm to 6 cm in diameter (1).
For treatment, surgical resection has shown a good prognosis and complete resection is even considered curative (1). Surgery without adjuvant systemic therapy was performed in 91% of reported cases (4), but some patients receive radiation therapy after the surgery (1). When resection is not possible due to diffuse lung involvement, chemotherapy becomes the treatment of choice (2, 4, 5). Concurrent chemotherapy and radiation therapy have shown effective, while a stand-alone chemotherapy or radiation therapy has shown significantly worse prognosis on a long-term (4). However, the patient in this report has received only the radiation therapy and has achieved a significant reduction in the tumor size. This case is the first case in Korean radiologic literature about the pulmonary plasmacytoma mimicking malignant lung cancer. This case characterized a lung cancer in morphology by involving lung parenchyma, bronchus, mediastinum, and lymph node. There are previously reported cases where plasmacytoma mimic the lung cancer, but those cases do not involve the lymph node (8). Therefore, this is the differentiated point of our case, and what makes this case more meaningful is how a positive outcome was achieved through the radiation therapy alone.
Figures and Tables
Fig. 2
Chest CT scan.
A. Axial image shows 5.8 × 4.8 cm heterogenous enhancing mass obstructing right bronchus intermedius and invading mediastinum.
B. Coronal image shows narrowing of right main bronchus by this mass and atelectasis of right middle and lower lobes.

Fig. 3
Positron emission tomography CT scan.
A. Axial fusion image shows increased fluorodeoxyglucose (FDG) uptakes (maximal standardized uptake value 6.9) in this mass.
B. Torso maximum intensity projection image shows increased FDG uptakes in this mass and mediastinal lymph nodes.

Fig. 5
Microscopic images of tumor tissue sampled by bronchoscopy.
A. The tumor composed of sheets of closely packed plasma cells which are characterized by an eccentric nucleus and basophilic cytoplasm. The plasma cells destroy the lung parenchyma and scattered fibrous bands course through the neoplasm (H&E, × 400).
B. Immunohistochemically, the tumor cells show diffuse reactivity with monoclonal λ-light chain of the cytoplasm (IHC × 400).
C. Immunohistochemically, the tumor cells show negative reaction with κ-light chain (IHC × 400).
Note.-IHC = immunohistochemistry

References
1. Montero C, Souto A, Vidal I, Fernández Mdel M, Blanco M, Verea H. [Three cases of primary pulmonary plasmacytoma]. Arch Bronconeumol. 2009; 45:564–566.
2. Kim SH, Kim TH, Sohn JW, Yoon HJ, Shin DH, Kim IS, et al. Primary pulmonary plasmacytoma presenting as multiple lung nodules. Korean J Intern Med. 2012; 27:111–113.
3. Koss MN, Hochholzer L, Moran CA, Frizzera G. Pulmonary plasmacytomas: a clinicopathologic and immunohisto-chemical study of five cases. Ann Diagn Pathol. 1998; 2:1–11.
4. Ujiie H, Okada D, Nakajima Y, Yoshino N, Akiyama H. A case of primary solitary pulmonary plasmacytoma. Ann Thorac Cardiovasc Surg. 2012; 18:239–242.
5. Mohammad Taheri Z, Mohammadi F, Karbasi M, Seyfollahi L, Kahkoei S, Ghadiany M, et al. Primary pulmonary plasmacytoma with diffuse alveolar consolidation: a case report. Patholog Res Int. 2010; 2010:463465.
6. Lim YH, Park SK, Oh HS, Choi JH, Ahn MJ, Lee YY, et al. A case of primary plasmacytoma of lymph nodes. Korean J Intern Med. 2005; 20:183–186.
7. Horiuchi T, Hirokawa M, Oyama Y, Kitabayashi A, Satoh K, Shindoh T, et al. Diffuse pulmonary infiltrates as a roentgenographic manifestation of primary pulmonary plasmacytoma. Am J Med. 1998; 105:72–74.
8. Goździuk K, Kedra M, Rybojad P, Sagan D. A rare case of solitary plasmacytoma mimicking a primary lung tumor. Ann Thorac Surg. 2009; 87:e25–e26.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download