INTRODUCTION
Cervical cancer is rare in the pediatric population. In cases of cervical cancer, adenocarcinoma is predominantly reported. Clear cell adenocarcinoma (CCAC) of the uterine cervix is very rare tumor, and accounts for only 4% of all adenocarcinomas of the uterine cervix. Furthermore, its radiological features have not been well described (1).
In this case report, we describe the imaging finding of CCAC of the uterine cervix in a 15-year-old girl with no history of intrauterine diethylstilbestrol (DES) exposure.
CASE REPORT
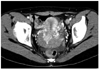
A 15-year-old adolescent girl complained of continuous vaginal bleeding over a duration of ten months. Her menarche occurred at 11 years of age. Although the presenting physician prescribed estrogen, it was ineffective in controlling the bleeding. A vaginal examination revealed an irregular mass arising from the vagina. Transrectal pelvic ultrasonography indicated a well-defined homogeneous hyperechoic mass in the upper vagina and cervix, measuring 7 cm (Fig. 1). Post-contrast computed tomography indicated a homogeneous well-defined enhancing mass occupying the uterine cervix and upper vagina, measuring 7 cm in maximum diameter. The mass abutted the bladder anteriorly and the rectum posteriorly (Fig. 2). Multiple enlarged lymph nodes were noted in the paraaortic as well as in both the common and external iliac areas. Further, the largest node measuring 3 cm was seen in the left external iliac chain.
Magnetic resonance imaging (MRI) was performed to evaluate the anatomic location of the main mass more accurately as well as the relationship between the mass, cervix, bladder and rectum. Axial and sagittal T2-weighted images presented a 7 × 4 × 7 cm lobulated mass, hyperintense versus myometrium, occupying the uterine cervix and upper vagina (Fig. 3A, B). Axial T1-weighted images showed an isointense mass, versus myometrium, occupying the uterine cervix and upper vagina (Fig. 3C). Gadolinium-enhanced, axial and sagittal T1-weighted images revealed a well-enhanced, homogeneous mass (Fig. 3D). No parametrial extension was evident and the interfaces between the mass, bladder and rectum were sharply delineated without tumor invasion. Multiple enlarged lymph nodes are also detected in both paraaortic areas as well as in both common and external iliac areas. F-18 fluorodeoxyglucose (FDG) positron emission tomography/CT (PET/CT) was also performed, revealing the presence of an area of an increased uptake in the uterine cervix and vagina, which corresponded to the lesion seen on CT and MRI (Fig. 4A). Multiple minimal hypermetabolic lesions were also visualized in the pelvic cavity and retroperitoneum (Fig. 4B). Cancer antigen 125 was elevated to 90 U/mL. After examination under anesthesia and biopsy, a diagnosis of International Federation of Gynecology and Obstetrics (FIGO) stage IIA carcinoma was made. Photomicrographs showed infiltrating tumor cells with a tubular-cystic growth pattern in the cervical stroma. Furthermore, tumor cells with clear cytoplasm often projected into the lumen of cysts and tubules with a 'hobnail appearance' (Fig. 5). The tumor was histologically confirmed as CCAC. Under a diagnosis of stage IIA CCAC, radical hysterectomy, bilateral ovary fixation and pelvic and paraaortic lymphadenectomy were performed. The tumor was originated from the cervix. Pathological examination revealed an invasion of the upper vagina and multiple pelvic and retroperitoneal lymph node metastases. Subsequently, six cycles of chemotherapy were administered every 3 weeks as follows; paclitaxel [135-175 mg/m2 (total dose 190 mg) was administered intravenously in normal saline 500 mL over 3 hours] and carboplatin (intravenously over 1 hour at a dose based on glomerular filtration rate to target an area under the concentration curve of 5 mg/min). The patient remained disease free at the time of writing (6 months after diagnosis).
DISCUSSION
CCAC is a rare tumor of the cervix, and its etiology and pathogenesis are unclear. However, many reports have associated this cancer subtype with prior intrauterine exposure to DES, a synthetic nonsteroidal estrogen hormone and teratogen with the ability to cross the placenta (2). During the 1970s and 1980s, the incidence of CCAC markedly increased, as DES was used therapeutically in early pregnancy in the belief that it would decrease complications, such as toxemia of pregnancy and bleeding, and help to reduce premature births and neonatal deaths. DES was widely used from 1946 to 1960 and its use continued until 1971, when the link between DES exposure and vaginal and cervical adenocarcinoma was first reported (2). The risk of CCAC development is 1 in 1000 for DES-exposed women up to the age of 34. However, in 25% of CCAC cases, no history of maternal hormone exposure was found (1, 3). Several factors, such as non-steroidal estrogen exposure during pregnancy, a maternal history of spontaneous abortion and premature birth are believed to contribute to CCAC, which has two peaks in its age/incidence distribution. Women in the younger group are aged 17 to 37 years (mean age, 26 years) and those in the older group are aged 44 to 88 years (mean age, 71 years). The younger group is largely composed of women exposed to DES, whereas the majority in the older group has no history of DES exposure (3).
The most common symptom in pediatric patients at presentation is vaginal bleeding (1). CCAC is often misdiagnosed as precocious puberty or anovulatory bleeding in a child or young women with prolonged vaginal bleeding. Routine vaginal cytology is often negative and the tumor is not palpated during rectal examination. Because young patients have a slightly higher incidence of advanced-stage disease, early diagnosis of the cervical mass is important in pediatric patients (4). Accordingly, abnormal vaginal bleeding in girls should be promptly investigated through a pelvic examination and appropriate imaging.
CCAC of uterine cervix and vagina in adolescent patients are reported in about thirty cases in the previous literatures; however, only three cases demonstrated the imaging findings of tumors. Donnelly et al. (5) described the CT and MRI finding of CCAC of the vagina in a 5-year-old girl. The mass was 5 × 3 cm in size, well-defined and hyperintense on T2-weighted images and isointense versus the vaginal wall on T1-weighted images; it did not invade the adjacent tissues. Gadolinium-enhanced MR images were not obtained. Herbst (6) reported a case of CCAC in an 8.6-year-old girl with a 4 × 5 cm well-defined, heterogeneous enhancing, soft tissue mass in the vagina, which was hyperintense on T2-weighted images and hypointense on T1-weighted images. Singh et al. (7) described the MRI finding of CCAC of cervix in a 13-year-old girl. On the T2-weighted image, the tumor showed a well-defined homogeneous hyperintensity, measuring 4 × 3 cm in size. The imaging findings reported in the cases of CCAC were similar to those observed in our case.
We also performed preoperative F-18 FDG PET/CT, which demonstrated the presence of a highly metabolic lesion in the uterine cervix and vagina and the presence of multiple distinct foci of FDG uptake in the pelvic cavity and retroperitoneum due to metastatic lymphadenopathies. To our knowledge, there was no study which described the PET/CT finding in the case of the CCAC patient. Our experiences suggest that F-18 FDG PET/CT can be valuable for evaluating CCAC of the uterine cervix with metastatic lymphadenopathy in the pelvic cavity and retroperitoneum.
Diagnostic imaging of adenocarcinoma of vagina and cervix contributes to therapeutic management, surgical planning and the prediction of prognosis. The prognosis of CCAC is closely related to primary tumor volume, extent, growth pattern, stage, nuclear atypia and mitotic activity (3). Although the ultrasound and CT identified the primary tumor in our patient, the MRI depicted a definite, delicate delineation of the tumor margin, tumor extent, growth pattern and involvements of the adjacent structure. Furthermore, the MRI provides a better depiction of genitourinary malformations, because CCAC has been associated with various complicated genitourinary malformations, such as artretic hemicervix, ipsilateral renal agenesis, bicornuate uterus and double uteri and vagina with unilateral renal agenesis.
The treatment of CCAC is similar to that of cervical cancer. Because most patients are young, surgery has been the mainstay of treatment. Radical hysterectomy and pelvic lymphadenectomy are the standard surgical treatments for patients with FIGO stage IB or IIA. A recent study revealed oncologic outcomes of fertility-sparing radical trachelectomy versus radical hysterectomy for stage IB1 cervical carcinoma in young adult women and found no statistically significant survival differences, indicating that for early stage cancer, fertility-sparing surgery is a safe option (8). Surgical resection is important for survival. Although radiotherapy is commonly used instead of surgery to treat adults with cervical cancer, surgery should be considered the treatment of choice for children or young adolescents due to the risk of radiation fibrosis of the bladder and bowel loop (1). Carboplatin and paclitaxel regimens have comparable response rates for the treatment of advanced adenocarcinoma of the cervix without toxicity (7).
CCAC in young children should be differentiated from embryonal rhabdomyosarcoma and endodermal sinus tumor. Embryonal rhabdomyosarcoma is one of the most common malignant vaginal tumors in young children and mostly occurs in children younger than 2 years old. MRI findings tend to be hypointensity on T1-weighted images, hyperintensity on T2-weighted images and heterogeneous enhancement in the contrast-enhanced phase (9). Vaginal endodermal sinus tumors are a rare entity and usually occur in children younger than 3 years old. The tumor showed uniform isointensity on T1-weighted images, heterogeneous hyperintensity on T2-weighted images and heterogeneous enhancement on contrast-enhanced images (10).
In this article, we described the ultrasonography, CT, MRI and F-18 FDG PET/CT findings of CCAC of the uterine cervix in an adolescent. Due to the aggressive nature of the tumor and limitations of vaginal examination in children, diagnostic imaging modalities should be considered promptly for any child complaining of vaginal bleeding in order to avoid delayed diagnosis.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download