Abstract
Pneumocephalus without a facial bone fracture or sinus disease is rare. A possible cause of pneumocephalus is high-pressure air applied into the orbit may cause without any evidence of a facial fracture (12345). The mechanism behind pneumocephalus may be secondary to a blast of air from the orbit to the intracranial space (12) with a degree of pressure (1). We report a case of compressed air injury induced by disseminated pneumocephalus in the absence of a facial bone fracture detected on multidetector computed tomography. After 5 days, a follow-up indicated that the pneumocephalus was almost completely resolved without visual loss.
Pneumocephalus without any evidence of fracture or sinusitis is a rare occurrence. Most cases reporting this condition are associated with orbital emphysema (12345). High pressure air as from a compressed air gun is a major cause of pneumocephalus which is applied intraorbitally (12345). The mechanism of the air flow into the cranial cavity from orbit cavity was suggested to be secondary to a blast of air from the optic canal to the subarachnoid canal (12). In this case report, we present the accidental occurrence of pneumocephalus due to a high pressure air gun into the orbit of the eye.
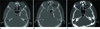
A previously healthy 51-year-old man exposed to a compressed air gun while cleaning an automobile was admitted with left eye swelling, conjunctival hemorrhage, periorbital ecchymosis, and mild visual disturbance. Multidetector computed tomography (MDCT) of the facial bone was performed with a 2.0 mm slice thickness. In addition, axial, sagittal, and coronal reformed images were obtained. On MDCT, no fracture was noted in the face, orbit, sinuses or skull base in any section. Extensive radiolucency consistent with air was detected over the left periorbital area and orbit cavity (Fig. 1A). Air was also seen around the optic canal and along the superior orbital fissure. Pneumocephalus within the subarachnoid spaces such as left suprasellar cistern, interpeduncular cistern, ambient cistern and along the left tentorium cerebellum, was observed (Fig. 1B).
There was no abnormal finding in the sclera, cornea, lens, vitreous and the optic disc of the left eye. An ophthalmological examination revealed that the intraocular pressure was within the normal range in the left eye without discrepancy between the both eyes. Moreover, no evidence of retinal detachment was seen. The patient's eyes were treated with topical antibiotics to prohibit intracranial infection. On a follow-up brain CT five days after, most of the intracerebral air was absorbed, while a small amount of air persisted around the left optic nerve within optic nerve sheath (Fig. 1C). One week later, the patient's visual acuity was recovered.
Pneumocephalus is commonly described in clinical situations when associated with facial trauma. However, pneumocephalus without a facial bone or skull fracture is rare. An example is the application of compressed air applied into the orbit (12345). Most of the compressed air injuries associated with pneumocephalus are accompanied with orbital emphysema (12345). There are several case reports of pneumocephalus due to high-pressure air into the orbit (12345). It is possible for air enter into the intracranial space if the air pressure exceeds 75 lbs·inch-2 (1).
Air entry into the cranial cavity was suggested in several cases (12345). In our case, we assume the compressed air first entered the intraconal space via the dissection of conjunctiva and then passed into the cranial cavity along the optic canal (12). There is a mechanism suggested for air entry into the intracranial space (12). Lubniewski and Feibel (1) presented a case with intracranial, bilateral orbital, and mediastinal air. They presented intracranial air adjacent to the superior orbital fissure and sella on CT (1). They demonstrated that air was injected intracranially but extradurally through the superior orbital fissure (1). The most likely explanation of the pneumocephalus was via dissection beneath the Tenon fascia, around the optic nerve, as suggested by Williams and Frankel (2). In their report, air via the Tenon facsia followed the optic canal into the intracranial subarachnoid space. We also considered that the air entry into the intracranial space without a facial or skull fracture most likely occurs via the Tenon fascia. The MDCT is especially very useful to detect the small amounts of air and enable its localization.
There are various risks of high-pressure injury to the orbit including direct contusion to the orbital contents, traumatic optic atrophy, injection of foreign bodies through the conjunctiva with the risk of infection and inflammation, displacement of the orbital contents with proptosis, transient corneal exposure, and blow-out fracture (67). Injury of the pial and arachnoidal blood supply to the optic nerve may lead to optic atrophy and poor vision (1).
The presence of pneumocephalus is a concern, because it indicates that the protective barriers of the brain have broken down. Prophylactic antibiotic therapy has an important role in preventing intracranial infection through the air entry route. The treatment of the pneumocephalus is mainly a conservative therapy, while the application of systemic and topical prophylactic antibiotics is more a general treatment. Usually, intracranial air is well tolerated but the pneumocephalus without facial or skull fracture has not been evaluated.
To date, there are no reports on the long term follow-up results of compressed induced pneumocephalus. Sequelae of traumatic brain injury include headaches, dizziness, anxiety, apathy, depression, aggression, cognitive impairments, personality changes, mania, psychosis and so on. Though the patient in our case showed no visual disturbance or orbital motor dysfunction for the short-term follow up, the complication of the pneumocephalus may happen. We suggest that long-term imaging follow-up of the patient can be helpful to predict a complication of the pneumocephalus.
In conclusion, high pressure air injury into the eye orbit led to disseminated pneumocephalus without any fracture to the face and skull. In addition, our patient's symptoms were almost completely resolved without visual disturbance or orbital motor dysfunction in short term follow-up. We detected these finding on the MDCT and absorbance of the air was also noted on follow-up study. Owing to the risks of serous sequelae secondary to injury with compressed air such as intracranial infection, prompt appropriate treatment such as prophylactic antibiotic therapy was required. For proper management in the short term, the patient was recovered without definite impairment of the orbit and brain. We suppose that it may help the patient to evaluate the complications of the brain injury as a prognosis in a long-term study.
Figures and Tables
Fig. 1
51-year-old man injured by a compressed air gun into left orbit.
A. Axial MDCT of the facial bone shows extensive emphysema over the left orbit. Air bubbles are detected around the optic nerve intraconal space (arrows). Pneumocephalus is detected in the sella along the optic canal (arrowheads).
B. Disseminated pneumocephalus is noted in sella and along the left tentorium cerebellum, subarachnoid space (arrowheads).
C. Five days after a follow-up MDCT of the brain shows the pneumocephalus and orbital emphysema as being almost completely resolved, with only a small amount of air bubbles remaining around the optic nerve intraconal space (arrow).
Note.-MDCT = multidetector computed tomography
References
1. Lubniewski AJ, Feibel RM. Traumatic air blast injury with intracranial, bilateral orbital, and mediastinal air. Ophthalmic Surg. 1989; 20:677–679.
2. Williams TR, Frankel N. Intracerebral air caused by conjunctival laceration with air hose. Arch Ophthalmol. 1999; 117:1090–1091.
3. Yildiz A, Duce MN, Ozer C, Apaydin FD, Eğilmez H, Kara E. Disseminated pneumocephalus secondary to an unusual facial trauma. Eur J Radiol. 2002; 42:65–68.
4. Kang BS. Disseminated head and neck emphysema with pneumocephalus due to air compressor injury into orbit. Am J Emerg Med. 2007; 25:223–225.
5. Yuksel M, Yuksel KZ, Ozdemir G, Ugur T. Bilateral orbital emphysema and pneumocephalus as a result of accidental compressed air exposure. Emerg Radiol. 2007; 13:195–198.
6. Hitchings R, McGill JI. Compressed air injury of the eye. Br J Ophthalmol. 1970; 54:634–635.
7. Li T, Mafee MF, Edward DP. Bilateral orbital emphysema from compressed air injury. Am J Ophthalmol. 1999; 128:103–104.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download