Abstract
We report here on the case of a 19-year-old woman who presented with progressive weakness of the lower extremities. The radiographs and CT showed vertebra plana of the first thoracic vertebral body. The mass had low signal intensity on the T1-weighted MR image and intermediate signal intensity on the T2-weighted MR image, and this low signal intensity extended to the spinal canal. Histological examination revealed a giant cell tumor (GCT). MR imaging is the imaging modality of choice for helping to distinguish spinal GCT from other spinal tumors by defining the extent and characteristic signal intensity of the tumor.
Vertebra plana is a radiologic diagnosis that indicates complete compression of the vertebral body (1). Although eosinophilic granuloma of the bone is the most frequent benign disease responsible for vertebra plana (2), it can be caused by several pathological conditions. Vertebral plana caused by a giant cell tumor (GCT) has been mentioned in only a few case reports in the English medical literature, and those case reports were without a detailed description (1). To the best of our knowledge, the computed tomography (CT) and magnetic resonance (MR) imaging features of GCT presenting as vertebra plana have seldom been reported in the radiological literature. We report here on the case of a young woman with a GCT involving the thoracic spine and this presented as vertebra plana.
A 19-year-old woman presented with a 10-day history of progressively worsening paraparesis. She also had a 1-month history of upper back pain that had been managed conservatively. The neurologic examination revealed bilateral hand grasp weakness and paraparesis. The results of the laboratory studies were within the normal limits. A swimmers lateral view radiograph of the cervical spine showed collapse of the first thoracic vertebra, and this was consistent with vertebral plana (Fig. 1). Contrast-enhanced CT showed marked collapse of the vertebra, which was surrounded by a well enhanced paravertebral mass that extended to the spinal canal. Round bony erosion due to the soft tissue mass was seen in the anterior aspect of the second thoracic vertebral body (Figs. 2A-C).
The mass showed low signal intensity on the T1-weighted image (Fig. 3A), intermediate signal intensity on the T2-weighted image (Fig. 3B) and strong enhancement on the gadolinium-enhanced T1-weighted image (Fig. 3C), and the mass's signal intensity was similar to that of the spinal cord. The presumptive preoperative diagnosis was eosinophilic granuloma and the alternative diagnosis was Ewing's sarcoma based on the radiological findings of vertebra plana. The patient underwent corpectomy of C7 and T1 and partial corpectomy of T2. A large extraspinal, intraspinal extradural tumor was identified primarily anterior to the spinal cord at C7 and T1. The tumor was removed subtotally and spine arthrodesis was performed. One month later, a second operation was performed for total removal of the residual tumor. There has been no recurrence of neurologic symptoms during 6 months of clinical follow up.
The pathological specimen (Fig. 4) of the tumor revealed proliferation of two cell populations: stromal cells and giant cells. The mononuclear stromal cells were round to oval and they lacked cytologic atypia. The giant cells were large and they contained 50-100 nuclei. Mitotic activity was frequent, while atypical mitotic figures were not found.
GCTs are relatively common, locally aggressive bone tumors, and they account for 4% to 9.5% of all primary osseous neoplasms and 18% to 23% of all benign bone neoplasms (34). The majority of GCTs occur at the ends of long bones such as at the knee joint, and only 7% occur in the spine. GCTs in the spine most commonly involve the sacrum, while the lumbar, thoracic and cervical spine may be affected in order of decreasing frequency (5).
In several large series, involvement of the thoracic spine accounted for only 1% to 2% of GCTs (67). GCTs of the spine develop in skeletally mature patients during the second to fourth decades of life, and they are more frequently seen in females (48). A GCT of the spine can present with pain (often with a radicular distribution), weakness and sensory deficits (910).
Like the GCTs in the appendicular bones, spinal GCTs show no evidence of a mineralized matrix. A GCT in the spine tends to affect the vertebral body rather than the posterior elements of the spine. Radiologically, spinal GCTs usually show as an expansile lesion with osteolysis (9). On CT, a spinal GCT appears as a soft-tissue density mass with well-defined margins that may show a thin rim of sclerosis. It may also have a homogeneous hypervascular appearance with contrast enhancement (6).
This type of tumor usually has low to intermediate signal intensity on T1-weighted MRI. Gadolinium enhancement of the lesion on T1-weighted MRI reflects its vascular supply. Cystic areas, foci of hemorrhage, fluid? fluid levels and a peripheral low-signal-intensity pseudocapsule may also be seen (3). In addition, GCTs may have signal intensity that is lower than or similar to that of the normal spinal cord on T2-weighted MRI in 63% to 96% of the cases (9). This feature may be caused by the relative collagen content of the fibrous components and the hemosiderin within the tumor (69).
Although most GCTs show expansile destruction of the vertebra, as was described in this case, a GCT can be seen as vertebra plana, which is defined by the following radiological criteria: collapse of one vertebral body only, normal adjacent intervertebral disks, the height of the intervertebral space is increased by at least one-third compared to normal and the collapsed vertebra shows increased density (1). Vertebra plana can be seen in various other diseases, including eosinophilic granulomas, myofibromatosis, aneurysmal bone cysts, osteosarcomas, lymphomas and Ewing's sarcomas (12). Vertebra plana could be produced by some disease processes that involve most of a vertebral body, and this is followed by spinal fractures. In our case, the initial working diagnosis was eosinophilic granuloma because it is the most common cause of vertebra plana in young patients. However, the radiologic features in our case, such as the presence of a paravertebral mass and involvement of the spinal canal and the adjacent vertebral bodies, were not typical of an eosinophilic granuloma. An eosinophilic granuloma is usually localized to one vertebra and it is contained by the periosteum, with no expansion to the paravertebral soft tissues (3). A previous report has described the involvement of both the vertebral bodies and posterior osseous elements by eosinophilic granuloma (7).
Ewing's sarcoma can also present as vertebra plana with extension to the posterior elements of the vertebra and it is one of the most common malignant tumors causing vertebra plana, which led us to include it in the differential diagnosis (12).
Owing to the rarity of a GCT presenting as vertebra plana, it was not considered in the differential diagnosis. Yet in retrospect, the MRI findings suggested the characteristic findings of a GCT tumor of the spine, including the presence of intermediate signal intensity on the T2-weighted image that was similar to that of the spinal cord. Given that this characteristic MRI feature was combined with imaging findings showing the involvement of two adjacent vertebrae and a posterior element, the diagnosis of spinal GCT should have been favored over eosinophilic granuloma and Ewing's sarcoma.
Surgery is the treatment of choice for giant cell tumor of the spine because it should be completely removed; the recurrence rate is slightly increased in cases with extension of giant cell tumor into the spinal canal and paraspinous space (3).
In conclusion, although rare, a GCT should be considered in the differential diagnosis of vertebra plana, and especially when observing tumor involvement of the adjacent vertebra or paravertebral tumor expansion, as well as when the tumor's signal intensity is similar to that of the spinal cord on the T2-weighted image.
Figures and Tables
Fig. 1
A 19-year-old woman with spinal GCT. The swimmers lateral view radiograph of the cervical spine, which was acquired with the patient with one arm up and one arm down, shows apparent collapse of the T1 vertebral body.

Fig. 2
A 19-year-old woman with a spinal GCT. The precontrast (A) and postcontrast axial CT (B) shows a soft tissue mass (arrowheads) that has destroyed the first thoracic vertebral body with extension to the spinal canal (arrow), and this mass shows homogeneous enhancement (arrowheads) on the contrast-enhanced axial CT (B). The sagittal CT reconstruction (C) shows the paper-thin vertebral body (arrowheads), with preservation of the intervertebral disc space. Round bony erosion is seen in the anterior aspect of the T2 vertebral body (arrow).

Fig. 3
A 19-year-old woman with a spinal GCT. The collapsed first thoracic vertebral body is surrounded by a paravertebral mass with low signal intensity (arrowheads) and the spinal cord is compressed on the T1-weighted image (A), and the mass shows intermediate signal intensity on the T2-weighted image (B) and homogenous enhancement on the contrast-enhanced T1-weighted image (C). MRI shows that the mass involves the anterior aspect of the second thoracic vertebral body (arrows), and this corresponds to the erosive lesion seen on CT (Fig. 2C).
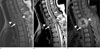
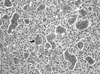
Fig. 4
The histological specimen shows that the tumor consists of mononuclear stromal cells evenly mixed with numerous osteoclast-like giant cells (arrow) (hematoxylin and eosin stain; original magnification, × 200). The mononuclear cells are round to oval or elongated and they lack cytologic atypia. The giant cells are large and they have over 20-30 nuclei.
References
1. Baghaie M, Gillet P, Dondelinger RF, Flandroy P. Vertebra plana: Benign or malignant lesion? Pediatr Radiol. 1996; 26:431–433.
2. Papagelopoulos PJ, Currier BL, Galanis E, Grubb MJ, Pritchard DJ, Ebersold MJ. Vertebra plana caused by primary ewing sarcoma: case report and review of the literature. J Spinal Disord Tech. 2002; 15:252–257.
3. Rodallec MH, Feydy A, Larousserie F, Anract P, Campagna R, Babinet A, et al. Diagnostic imaging of solitary tumors of the spine: What to do and say. Radiographics. 2008; 28:1019–1041.
4. Murphey MD, Nomikos GC, Flemming DJ, Gannon FH, Temple HT, Kransdorf MJ. From the archives of AFIP. Imaging of giant cell tumor and giant cell reparative granuloma of bone: radiologicpathologic correlation. Radiographics. 2001; 21:1283–1309.
5. Hart RA, Boriani S, Biagini R, Currier B, Weinstein JN. A system for surgical staging and management of spine tumors. A clinical outcome study of giant cell tumors of the spine. Spine. 1997; 22:1773–1782.
6. Sakurai H, Mitsuhashi N, Hayakawa K, Niibe H. Giant cell tumor of the thoracic spine simulating mediastinal neoplasm. AJNR Am J Neuroradiol. 1999; 20:1723–1726.
7. Johnson S, Klostermeier T, Weinstein A. Case report 768. Eosinophilic granuloma of the cervical spine. Skeletal Radiol. 1993; 22:63–65.
8. Sanjay BK, Sim FH, Unni KK, McLeod RA, Klassen RA. Giant-cell tumours of the spine. J Bone Joint Surg Br. 1993; 75:148–154.
9. Kwon JW, Chung HW, Cho EY, Hong SH, Choi SH, Yoon YC, et al. MRI findings of giant cell tumors of the spine. AJR Am J Roentgenol. 2007; 189:246–250.
10. Bidwell JK, Young JW, Khalluff E. Giant cell tumor of the spine: computed tomography appearance and review of the literature. J Comput Tomogr. 1987; 11:307–311.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download