1. Menkes JH, Alter M, Steigleder GK, Weakley DR, Sung JH. A sex-linked recessive disorder with retardation of growth, peculiar hair, and focal cerebral and cerebellar degeneration. Pediatrics. 1962; 29(5):764–779.

2. Danks DM, Campbell PE, Walker-Smith J, Stevens BJ, Gillespie JM, Blomfield J, et al. Menkes' kinky-hair syndrome. Lancet. 1972; 1(7760):1100–1102.


3. Tümer Z, Møller LB. Menkes disease. Eur J Hum Genet. 2010; 18(5):511–518.


4. Vulpe C, Levinson B, Whitney S, Packman S, Gitschier J. Isolation of a candidate gene for Menkes disease and evidence that it encodes a copper-transporting ATPase. Nat Genet. 1993; 3(1):7–13.


5. Chelly J, Tümer Z, Tønnesen T, Petterson A, Ishikawa-Brush Y, Tommerup N, et al. Isolation of a candidate gene for Menkes disease that encodes a potential heavy metal binding protein. Nat Genet. 1993; 3(1):14–19.


6. Mercer JF, Livingston J, Hall B, Paynter JA, Begy C, Chandrasekharappa S, et al. Isolation of a partial candidate gene for Menkes disease by positional cloning. Nat Genet. 1993; 3(1):20–25.

7. El Meskini R, Culotta VC, Mains RE, Eipper BA. Supplying copper to the cuproenzyme peptidylglycine alpha-amidating monooxygenase. J Biol Chem. 2003; 278(14):12278–12284.

8. Kodama H, Okabe I, Yanagisawa M, Kodama Y. Copper deficiency in the mitochondria of cultured skin fibroblasts from patients with Menkes syndrome. J Inherit Metab Dis. 1989; 12(4):386–389.

9. Petris MJ, Strausak D, Mercer JF. The Menkes copper transporter is required for the activation of tyrosinase. Hum Mol Genet. 2000; 9(19):2845–2851.

10. Qin Z, Itoh S, Jeney V, Ushio-Fukai M, Fukai T. Essential role for the Menkes ATPase in activation of extracellular superoxide dismutase: implication for vascular oxidative stress. FASEB J. 2006; 20(2):334–336.


12. Horn N, Tümer Z. Menkes disease and the occipital horn syndrome. In : Royce PM, Steinmann B, editors. Connective Tissue and Its Heritable Disorders: Molecular, Genetic, and Medical Aspects. 2nd ed. New York, NY: John Wiley and Sons Inc.;2002. p. 651–685.
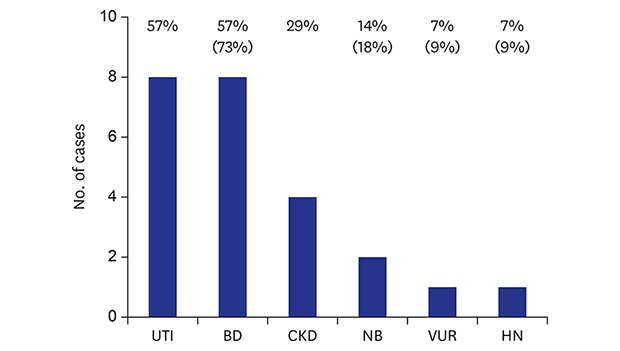
13. Zaffanello M, Maffeis C, Fanos V, Franchini M, Zamboni G. Urological complications and copper replacement therapy in childhood Menkes syndrome. Acta Paediatr. 2006; 95(7):785–790.


14. Lee JS, Lim BC, Kim KJ, Hwang YS, Cheon JE, Kim IO, et al. Menkes disease in Korea:
ATP7A mutation and epilepsy phenotype. Brain Dev. 2015; 37(2):223–229.

15. Smpokou P, Samanta M, Berry GT, Hecht L, Engle EC, Lichter-Konecki U. Menkes disease in affected females: the clinical disease spectrum. Am J Med Genet A. 2015; 167A(2):417–420.


17. Das S, Levinson B, Whitney S, Vulpe C, Packman S, Gitschier J. Diverse mutations in patients with Menkes disease often lead to exon skipping. Am J Hum Genet. 1994; 55(5):883–889.


18. Tümer Z, Møller LB, Horn N. Mutation spectrum of
ATP7A, the gene defective in Menkes disease. Adv Exp Med Biol. 1999; 448:83–95.

19. Gu YH, Kodama H, Murata Y, Mochizuki D, Yanagawa Y, Ushijima H, et al.
ATP7A gene mutations in 16 patients with Menkes disease and a patient with occipital horn syndrome. Am J Med Genet. 2001; 99(3):217–222.

20. Tümer Z, Birk Møller L, Horn N. Screening of 383 unrelated patients affected with Menkes disease and finding of 57 gross deletions in ATP7A. Hum Mutat. 2003; 22(6):457–464.

21. Møller LB, Bukrinsky JT, Mølgaard A, Paulsen M, Lund C, Tümer Z, et al. Identification and analysis of 21 novel disease-causing amino acid substitutions in the conserved part of
ATP7A
. Hum Mutat. 2005; 26(2):84–93.

22. Rucker RB, Kosonen T, Clegg MS, Mitchell AE, Rucker BR, Uriu-Hare JY, et al. Copper, lysyl oxidase, and extracellular matrix protein cross-linking. Am J Clin Nutr. 1998; 67(5):Suppl. 996S–1002S.

24. Harcke HT Jr, Capitanio MA, Grover WD, Valdes-Dapena M. Bladder diverticula and Menkes' syndrome. Radiology. 1977; 124(2):459–461.


25. Kodama H, Murata Y, Kobayashi M. Clinical manifestations and treatment of Menkes disease and its variants. Pediatr Int. 1999; 41(4):423–429.


26. Oshio T, Hino M, Kirino A, Matsumura C, Fukuda K. Urologic abnormalities in Menkes' kinky hair disease: report of three cases. J Pediatr Surg. 1997; 32(5):782–784.


27. Eradi B, Rajimwale A. Excision of massive bladder diverticula in Menkes disease. J Pediatr Urol. 2010; 6(3):312–314.


28. Kageyama S, Okada Y, Konishi T, Koizumi S, Tomoyoshi T. Menkes' kinky hair disease associated with a large bladder diverticulum: a case report. Int J Urol. 1997; 4(3):318–320.


29. Hebert KL, Martin AD. Management of bladder diverticula in Menkes syndrome: a case report and review of the literature. Urology. 2015; 86(1):162–164.

30. Tobias JD. Anaesthetic considerations in the child with Menkes' syndrome. Can J Anaesth. 1992; 39(7):712–715.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download