1. Deleanu B, Prejbeanu R, Vermesan D, Haragus H, Icma I, Predescu V. Acute abdominal complications following hip surgery. Chirurgia (Bucur). 2014; 109(2):218–222.

3. Abrahamson J, Eldar S. Acute cholecystitis after orthopaedic operations. Int Orthop. 1988; 12(1):93–95.


4. Lee SH, Chun CS. Post-traumatic and post-operative cholecystitis in Korea. Ann Surg Treat Res. 1986; 30(2):149–156.
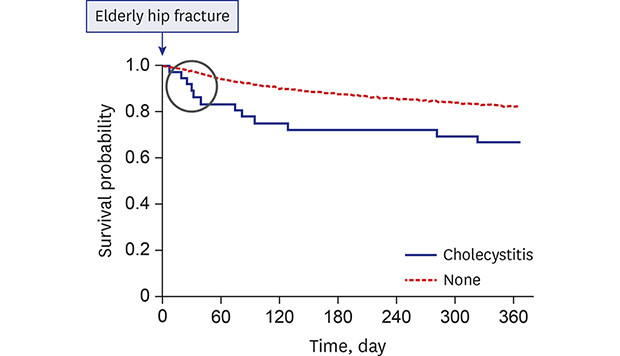
6. Choo SK, Park HJ, Oh HK, Kang YK, Kim Y. Acute cholecystitis in elderly patients after hip fracture: incidence and epidemiology. Geriatr Gerontol Int. 2016; 16(3):380–383.


7. Peer A, Hendel D, Halperin N. Acute cholecystitis and cholestasis as a complication in hip surgery. Injury. 1982; 14(2):159–161.

8. Lee J, Lee JS, Park SH, Shin SA, Kim K. Cohort profile: the national health insurance service–national sample cohort (NHIS-NSC), South Korea. Int J Epidemiol. 2017; 46(2):e15.

9. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7(9):e016640.

10. Park C, Jang S, Jang S, Ha YC, Lee YK, Yoon HK, et al. Identification and validation of osteoporotic hip fracture using the National Health Insurance database. J Korean Hip Soc. 2010; 22(4):305–311.

11. Lee YK, Ha YC, Choi HJ, Jang S, Park C, Lim YT, et al. Bisphosphonate use and subsequent hip fracture in South Korea. Osteoporos Int. 2013; 24(11):2887–2892.


14. Welch JP, Malt RA. Outcome of cholecystostomy. Surg Gynecol Obstet. 1972; 135(5):717–720.

15. Glenn F. Acute acalculous cholecystitis. Ann Surg. 1979; 189(4):458–465.


16. Tsang ST, Aitken SA, Golay SK, Silverwood RK, Biant LC. When does hip fracture surgery fail? Injury. 2014; 45(7):1059–1065.


17. Smith T, Pelpola K, Ball M, Ong A, Myint PK. Pre-operative indicators for mortality following hip fracture surgery: a systematic review and meta-analysis. Age Ageing. 2014; 43(4):464–471.


18. Cha YH, Ha YC, Yoo JI, Min YS, Lee YK, Koo KH. Effect of causes of surgical delay on early and late mortality in patients with proximal hip fracture. Arch Orthop Trauma Surg. 2017; 137(5):625–630.


20. von Friesendorff M, McGuigan FE, Wizert A, Rogmark C, Holmberg AH, Woolf AD, et al. Hip fracture, mortality risk, and cause of death over two decades. Osteoporos Int. 2016; 27(10):2945–2953.


21. Hafif A, Gutman M, Kaplan O, Winkler E, Rozin RR, Skornick Y. The management of acute cholecystitis in elderly patients. Am Surg. 1991; 57(10):648–652.

22. Glenn F, Wantz GE. Acute cholecystitis following the surgical treatment of unrelated disease. Surg Gynecol Obstet. 1956; 102(2):145–153.

23. Goisser S, Schrader E, Singler K, Bertsch T, Gefeller O, Biber R, et al. Malnutrition according to mini nutritional assessment is associated with severe functional impairment in geriatric patients before and up to 6 months after hip fracture. J Am Med Dir Assoc. 2015; 16(8):661–667.

24. Karres J, Kieviet N, Eerenberg JP, Vrouenraets BC. Predicting early mortality after hip fracture surgery: the hip fracture estimator of mortality Amsterdam. J Orthop Trauma. 2018; 32(1):27–33.


25. Yi NJ, Han HS, Kim YW, Min SK, Choi YM. The safety of a laparoscopic cholecystectomy in acute cholecystitis in high risk patients older than sixty. J Korean Surg Soc. 2003; 64(5):396–401.
26. Suissa S. Immortal time bias in pharmaco-epidemiology. Am J Epidemiol. 2008; 167(4):492–499.








 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download