INTRODUCTION
Acute pyelonephritis (APN) is one of the most common community-based bacterial infections. The annual incidence rate of APN is 15–17 cases per 10,000 persons in the U.S., and 80% of the cases occur in women.
1 It is estimated that half of all women have at least one episode of urinary tract infection (UTI) including APN during their adult life.
2
Although APN responds well to antimicrobial agents, increasing antimicrobial-resistant uropathogens make its treatment difficult.
3 Extended-spectrum beta-lactamase (ESBL)-producing or fluoroquinolone-resistant Enterobacteriaceae have emerged as significant pathogens in hospital-acquired infections as well as in community-acquired infections, which results in reduced clinical efficacy in APN treatment.
345 Recently, the U.K. experienced a gradual increase of
Escherichia coli bacteremia over 14 years from 2000, and the major source of infection was UTI.
6 This increase in
E. coli bacteremia may be in part explained by the aging population, increased international travel, and consumption of antibiotics. According to a prospective observational study in Korea, antimicrobial resistance rates among
E. coli are as high as those in the U.K.; 21.3% for fluoroquinolone, and 9.3% for 3rd generation cephalosporins among
E. coli from community-acquired APN during 2010–2012.
7 These resistance rates are likely to have changed the other epidemiologic characteristics of APN in Korea.
The purpose of this study was to describe the current epidemiologic characteristics such as incidence, mortality, recurrence, medical cost, and admission/visit days due to APN in Korea.
METHODS
Data source
The National Health Insurance System of Korea covers almost the entire population, including low-income families with medical aid: 98% of the entire population were covered in 2014.
8 We obtained insurance claim data of the National Health Insurance Corporation which provides online health insurance data service through Health Insurance Review and Assessment Service. Our data over January 2010 to June 2015 include patient information about age, gender, insurer type, clinic or hospital code, area of the clinic or hospital, care type (inpatient/outpatient), treatment start date, treatment days, admission/visit days, primary discharge diagnosis code, sub-discharge diagnosis code, relevant department, medical cost, and prescription pharmaceuticals. The discharge diagnosis codes follow the International Classification of Diseases, 10th Revision (ICD-10). Usually, there is a 1 to 2-month lag for billing in national health insurance claim.
Definitions
We included the patients whose primary discharge diagnosis was APN from 2010 to 2014: ICD-10 codes N10 (acute tubulo-interstitial nephritis) and N12 (tubulo-interstitial nephritis, not specified as acute or chronic) were selected because these codes are used as diagnostic codes of APN in Korea. Two or more claims during a 14-day period were considered as a single episode.
9 If claims of both inpatient and outpatient existed in a single episode, we classified it as an inpatient episode. As for exclusion criteria, firstly, we excluded the patients < 15 years of age because the target population in this study was adults. Secondly, the episodes with zero admission/visit day, zero medical cost or no antibiotic prescription were excluded. Finally, claims of Veteran Health Insurance were excluded, because beneficiaries of Veteran Health Insurance could claim double with a single event (
Fig. 1).
Fig. 1
Flow diagram showing the process of selecting episodes with APN based on health insurance claim data.
APN = acute pyelonephritis.

When an episode's treatment result was recorded as ‘death,’ the case is classified as an in-hospital mortality case.
Episodes without an APN episode during the previous 12 months are considered “sporadic.” In contrast, episodes with a sporadic or recurrent APN episode during the previous 12 months are considered “recurrent.” If the time interval between two consecutive episodes is longer than 12 months, then the second episode is regarded as sporadic. The other episodes are “undefined”; all episodes in 2010 are classified as “undefined” because analysis of APN episodes during the previous 12 months is impossible with our data. Furthermore, an episode within 12 months after an undefined episode is also classified as “undefined” to be excluded from recurrence analysis.
9
The medical cost in our study includes all expenses paid by patient and health insurance: clinic charge per physician visit, cost per prescription, hospitalization charge, procedure or operation charge, laboratory test charge, radiologic examination charge, etc. Non-reimbursed medical costs are not included. All costs are in USD (1 USD ≒ 1,150 KRW).
As for payer type, the patients in our study are coved either by the national health insurance or medical aid; the medical aid is a national health-care program for low-income families. If multiple payer types, hospital types or departments were involved in the same episode, we use only the type or department for hospitalization prior to outpatient visit, or if no hospitalization, then the first recorded type or department for the episode.
Data analysis and statistics
Incidence rates were calculated using the population size data from the Statistic Korea as the denominator, because the National Health Insurance System of Korea covers almost the entire population. The estimated annual population size with age ≥ 15 in Korea was: 42,495,697 in 2010; 42,923,904 in 2011; 43,434,585 in 2012; 43,708,344 in 2013; and 44,073,517 in 2014.
10
To find the yearly trend of age, mortality rate, average medical cost, and average admission/visit days, linear regression analysis for five yearly time-series observations was applied to each variable with time as the single explanatory variable, and the P value of the slope estimate of time is used as the P value for the trend. As for the seasonality of APN incidence, linear regression analysis for 60 monthly time-series observations was done with the monthly dummy variables as the regressors, and the P value was obtained from the test for zero slopes of the monthly dummy variables. We adopt P value < 0.05 as statistical significance. All analyses were done with SAS enterprise guide version 6.1 (SAS Institute Inc., Cary, NC, USA).
Ethics statement
The study protocol was approved by the Institutional Review Boards (IRB) of Hanyang University Hospital (IRB number: 2016-01-032), and the requirement for written informed consent from patients was waived.
RESULTS
Incidence
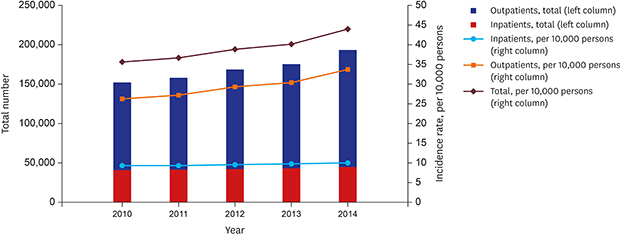
A total of 845,656 APN episodes were identified during 2010–2015 in Korea (151,380 in 2010; 157,353 in 2011; 168,470 in 2012; 175,208 in 2013; and 193,245 in 2014). Most cases (93.1%) met N10 code (acute tubulo-interstitial nephritis). The overall annual incidence rate (per 10,000 persons) of APN was 39.1 and were on the increase year to year (35.6 in 2010; 36.7 in 2011; 38.9 in 2012; 40.1 in 2013; and 43.8 in 2014;
P = 0.004). The increasing trend was observed in both inpatients (9.4 in 2010; 9.4 in 2011; 9.6 in 2012; 9.7 in 2013; and 10.1 in 2014;
P = 0.014) and outpatients (26.2 in 2010; 27.2 in 2011; 29.3 in 2012; 30.4 in 2013; and 33.8 in 2014;
P = 0.004) (
Fig. 2). This trend was present in both men (5.8 in 2010; 5.8 in 2011; 6.3 in 2012; 6.5 in 2013; and 8.0 in 2014;
P = 0.042) and women (65.1 in 2010; 67.2 in 2011; 71.1 in 2013; 73.3 in 2013; and 79.3 in 2014;
P = 0.003); for those aged under 55 years (30.6 in 2010; 31.5 in 2011; 32.7 in 2012; 33.2 in 2013; and 36.4 in 2014;
P = 0.014) and 55 years and over (50.4 in 2010; 51.3 in 2011; 55.5 in 2012; 57.4 in 2013; and 61.7 in 2014;
P = 0.003).
Fig. 2
Annual incidence of APN episodes in Korea, 2010–2014.
APN = acute pyelonephritis.
For inpatients, the increasing trend in annual incidence rate was significant in secondary hospitals (4.96 in 2010; 4.95 in 2011; 5.11 in 2012; 5.28 in 2013; and 5.64 in 2014; P = 0.020), but it was not significant in tertiary hospitals (1.46 in 2010; 1.39 in 2011; 1.36 in 2012; 1.39 in 2013; and 1.43 in 2014; P = 0.686), hospitals (2.44 in 2010; 2.53 in 2011; 2.59 in 2012; 2.51 in 2013; and 2.55 in 2014; P = 0.332), and local clinics (0.49 in 2010; 0.52 in 2011; 0.49 in 2012; 0.50 in 2013; and 0.44 in 2014; P = 0.234). As for outpatients, the increasing trend was significant in secondary hospitals (4.23 in 2010; 4.28 in 2011; 4.91 in 2012; 5.04 in 2013; and 5.31 in 2014; P = 0.008), hospitals (2.10 in 2010; 2.35 in 2011; 2.76 in 2012; 2.80 in 2013; and 3.23 in 2014; P = 0.003), and local clinics (18.50 in 2010; 19.15 in 2011; 20.03 in 2012; 21.04 in 2013; and 23.61 in 2014; P = 0.001), while it remained relatively stable in tertiary hospitals (1.33 in 2010; 1.37 in 2011; 1.47 in 2012; 1.40 in 2013; and 1.49 in 2014; P = 0.086).
Eleven times more women were diagnosed and treated with APN than men (men vs. women, 6.5 vs. 71.3). One of every 4.1 patients was hospitalized (inpatients vs. outpatients, 9.6 vs. 29.4). The incidence rate of inpatients was 18.9 for women and 1.5 for men; for outpatients, 54.4 for women and 5.0 for men. The incidence rate increased with age among both inpatients (
P < 0.001) and outpatients (
P < 0.001). The incidence rate for inpatients increased with age faster than that for outpatients (
Fig. 3).
Fig. 3
Incidence rate (per 10,000 persons) of APN episodes in Korea by age group, 2010–2014.
APN = acute pyelonephritis.

As for payer type, the majority of patients were coved by health insurance; the ratio of health insurance to the medical aid was approximately 15:1. The ratio was higher in outpatients than inpatients (18:1 vs. 10:1) and in women than men (16:1 vs. 11:1). For hospital type, secondary hospitals (total 53.8%; men 56.1%; women 53.6%) and local clinics (total 69.6%; men 69.4%; women 69.7%) are the major type for inpatient and outpatient episodes, respectively.
The incidence rate was higher in both inpatients and outpatients during summer (June to August), compared with the other seasons in all study years (
P < 0.001;
Fig. 4).
Fig. 4
Monthly incidence rate (per 10,000 persons) of APN episodes in Korea, 2010–2014.
APN = acute pyelonephritis.

In-hospital mortality
A total of 500 episodes' outcome was recorded as death from 2010 to 2014 (89 in 2010; 75 in 2011; 116 in 2012; 106 in 2013; and 114 in 2014). The overall in-hospital mortality rate per 1,000 APN episodes during our study period was 0.6; the in-hospital mortality of man patients was higher than woman patients (men vs. women, 1.5 vs. 0.5). The annual in-hospital mortality rate remained stable throughout the study years (P = 0.718).
Recurrence
Table 1 shows the recurrence rates of APN within 12 months following a sporadic or recurrent episode. Overall, 15.8% experienced recurrence within 12 months, and women experienced recurrence more than men (men vs. women, 13.1% vs. 16.1%). The median duration until the first recurrence was 44 days; it was shorter in men than in women (men vs. women, 29 vs. 46 days). From the second recurrence and thereafter, the duration until the next recurrence gradually shortened as the number of recurrences increased. The recurrence rate increased with the number of previous recurrences for both genders; among patients with 1, 2, 3, and 4 previous recurrences, 29.9%, 43.2%, 52.6%, and 59.6% experienced a subsequent recurrence, respectively. The recurrence rate varied depending on the duration for the previous recurrence. For example, if the duration between the first and second recurrence was < 61 days, the risk of a third recurrence was 54.8%.
Table 1
Recurrence rate of APN within 12 months following a sporadic or recurrent episode

|
Episode |
Frequency |
Median duration between 2 consecutive episodes, day |
Recurrence rate given the preceding recurrence, % |
Recurrence rate by the duration since the previous recurrence, %a
|
|
< 61 day |
61–120 day |
≥ 121 day |
|
Total |
|
|
|
|
|
|
|
Sporadic |
532,834 |
|
|
|
|
|
|
1st recurrence |
84,213 |
44 |
15.8 |
|
|
|
|
2nd recurrence |
25,195 |
56 |
29.9 |
42.4 |
49.6 |
41.0 |
|
3rd recurrence |
10,880 |
53 |
43.2 |
54.8 |
54.5 |
46.8 |
|
4th recurrence |
5,728 |
50 |
52.6 |
60.3 |
60.0 |
57.8 |
|
5th recurrence |
3,416 |
47 |
59.6 |
66.9 |
62.1 |
53.1 |
|
≥ 6th recurrence |
7,901 |
|
|
|
|
|
|
Undefined |
174,961 |
|
|
|
|
|
|
Men |
|
|
|
|
|
|
|
Sporadic |
45,593 |
|
|
|
|
|
|
1st recurrence |
5,971 |
29 |
13.1 |
|
|
|
|
2nd recurrence |
1,836 |
35 |
30.7 |
46.7 |
40.9 |
41.7 |
|
3rd recurrence |
826 |
33 |
45.0 |
56.9 |
68.0 |
47.9 |
|
4th recurrence |
469 |
32 |
56.8 |
62.7 |
58.6 |
47.8 |
|
5th recurrence |
281 |
31 |
59.9 |
67.8 |
58.5 |
62.5 |
|
≥ 6th recurrence |
929 |
|
|
|
|
|
|
Undefined |
13,946 |
|
|
|
|
|
|
Women |
|
|
|
|
|
|
|
Sporadic |
487,241 |
|
|
|
|
|
|
1st recurrence |
78,242 |
46 |
16.1 |
|
|
|
|
2nd recurrence |
23,359 |
59 |
29.9 |
42.0 |
50.2 |
41.0 |
|
3rd recurrence |
10,054 |
55 |
43.0 |
54.5 |
53.8 |
46.7 |
|
4th recurrence |
5,259 |
52 |
52.3 |
60.0 |
60.1 |
58.4 |
|
5th recurrence |
3,135 |
49 |
59.6 |
66.8 |
62.3 |
52.7 |
|
≥ 6th recurrence |
6,972 |
|
|
|
|
|
|
Undefined |
161,015 |
|
|
|
|
|
Medical cost
The overall annual gross cost was USD 52.3 million in 2010, USD 56.0 million in 2011, USD 58.0 million in 2012, USD 61.3 million in 2013, and USD 68.1 million in 2014. The average medical cost per episode was 12.9 times higher in inpatients compared with outpatients (inpatients USD 1,144 vs. outpatients USD 89), and 1.2 times higher in men than women (men USD 420 vs. women USD 343). The average medical cost was on the increase year to year throughout the study period in inpatients (
P = 0.009) while there was no significant change in outpatients (
P = 0.342;
Fig. 5). If medical cost includes only clinic charge per physician visit, cost per prescription and hospitalization charge, then the average cost of APN would be USD 693 (men USD 874 and women USD 676) for inpatients and USD 49 (men USD 38 and women USD 50) for outpatients. The medical cost trend remained stable throughout the study period (inpatients
P = 0.866 and outpatients
P = 0.164). The average medical cost increased with age among inpatients (
P < 0.001), but it had no significant change across different age groups of outpatients (
P = 0.439).
Fig. 5
Annual medical cost of APN episodes in Korea, 2010–2014.
APN = acute pyelonephritis.

Admission or visit days
The average hospitalization duration per episode was 9.0 days; the average number of visits per episode was 2.2. No significantly increasing or decreasing annual trend was seen in both inpatients and outpatients (inpatients P = 0.466 and outpatients P = 0.080). Men stayed longer per inpatient episode (men vs. women, 10.5 vs. 8.9 days). In contrast, women visited more often per outpatient episode (men vs. women, 1.9 vs. 2.3). The average hospitalization duration increased with age (P < 0.001), but it had no significant change across different age groups of outpatients (P = 0.653).
DISCUSSION
In this paper, we showed that the annual incidence rate of APN has been increasing in Korea. But there are a couple of factors that make this finding somewhat tentative. Firstly, the data came from the claims database of the Health Insurance Review and Assessment Service, and the quality of the data is not exactly the best possible. For instance, there are many patients with the ICD-10 codes N10 or N12 who did not receive any antibiotics, which is hard to believe. Also, for patients treated in local clinics, the diagnosis of APN might be false because most patients with systemic symptoms and signs tend to be admitted to hospital in Korea, which means that patients treated for APN in local clinics might have been patients of cystitis or asymptomatic carriers. Secondly, in 2011, the Korean government defined cystitis as an elementary infection with common cold to be treated in local clinics or small hospitals, and made it more expensive for cystitis to be treated in tertiary hospitals. Hence, doctors in secondary or tertiary hospitals might have put down APN as the code of systemic diseases for patients with cystitis in order to reduce their medical expense. Despite this, however, when we analyzed inpatients admitted to hospitals to avoid errors in outpatient data, an increasing trend of APN was still seen. Other than these factors, availability of medical service such as entry barriers to medical service and expansion of private medical insurance might have affected the incidence of APN.
Considering factors causing the increasing incidence rate of APN, evolution in
E. coli strains might have an important contributing factor. ST131 clone of
E. coli, which is notorious for antimicrobial resistance and extensive virulence profile, has increased in both community and hospital UTIs worldwide.
111213 For instance, in the U.K., the proportion of ST131 clone substantially increased among
E. coli isolates from bacteremia during 2001–2010, and
E. coli sepsis increased further by 16% during 2010–2014.
1114 In Korea, the proportion of ST131 strain isolated from community-acquired
E. coli bacteremia, which was 19.7% (15/76) during 2006–2011, jumped to 26.9% (32/119) in 2016.
1516 Also, the virulence of
E. coli might have changed.
We found 500 deaths caused by APN during 2010–2014 and our estimated in-hospital mortality rate per 1,000 APN episodes was 0.6. In comparison, all death certificates in Korea from the Statistics Korea indicate 1,122 deaths caused by APN (men 207; women 915) during the same period.
17 The possible reasons for the discrepancy are; 1) the death certificates from the Statistics Korea included deaths outside of hospital, and 2) some severe or fatal cases such as those whose primary diagnosis code was sepsis might have been left out in our study. Considering the death certificate analysis and this paper's findings, the mortality rate per 1,000 APN episodes in Korea is likely to range from 0.6 to 1.3.
Recurrence is a common problem among APN patients. Approximately 15.8% of APN patients experienced recurrence within 12 months in our study. This recurrence rate is much higher than 9.2% and 5.7% for women and men, respectively, in a preceding study for Korea.
9 A number of factors seem to predispose APN patients to recurrence. For instance, host genetic factors increasing the susceptibility of vaginal colonization with uropathogens and behavior factors (such as sexual intercourse, diaphragm-spermicide use, and bladder emptying) play a role in recurrence of UTI.
18 Virulence of uropathogens and patients' underlying conditions such as diabetes may also predispose patients to APN recurrence.
1920 Interestingly, we found that as the number of the previous recurrences increased, the interval between episodes became shorter, and the probability of further recurrences became higher.
The average medical cost increased among inpatients (from USD 1,076 to USD 1,230), but remained stable among outpatients (at about USD 85 to USD 90). The average hospital days or outpatient visit numbers were also stable throughout the study period. These seem to be due to changes in the cost of diagnosis or treatment. As for treatment, the average antibiotic cost did not change much throughout the study years (the data not shown). Instead, the diagnostic cost of APN might have changed substantially as follows.
Abdominal computed tomography (CT) and ultrasonography (US) are taken for most hospitalized APN patients in Korea since late 2000s. In a previous prospective study from 2010 to 2011, 78.3% of APN patients admitted to hospitals in Korea underwent abdominal CT (57.7%), abdominal US (17.7%), or both (2.8%) within 7 days of admission.
21 As for radiologic imaging studies for community-acquired APN, the American College of Radiology recommended a 72 hours waiting period before carrying out any imaging,
2223 and proposed CT as the imaging method of choice for diagnosing patients with atypical pyelonephritis,
22 which suggests that unnecessary radiologic imaging might have been done for the diagnosis of typical uncomplicated APN in Korea. In most developed countries including Korea, use of CT and magnetic resonance imaging (MRI) has much increased in the last two decades.
24 In the U.S., CT imaging doubled, and MRI imaging tripled during 1997–2006, despite that the disease burden itself remained more or less the same.
25
The main strength of the present study is the data source: National Health Insurance data, which is the most representative health data in Korea. Even though the reliability of diagnosis is somewhat questionable as in other studies using administrative data, still there is no denying that these data are an important tool in analyzing medical practices in Korea. APN has homogeneous pathology and simple diagnostic criteria, which simplifies analysis using large data based on the entire population.
26 We also note that approximately 80% of the patients whose discharge diagnosis was APN met the admission criteria in Canada.
20 Despite the above strength, there are some limitations in our data as well. Firstly, as in other studies using administrative data, diagnosis is fully dependent on physicians, across whom diagnostic criteria may vary. Secondly, only the main discharge diagnosis of APN was included; some cases might have been coded as a sub-discharge diagnosis under other ICD-codes such as gram-negative sepsis and adult respiratory distress syndrome. Thirdly, our data source does not contain non-reimbursed medical cost, possibly resulting in an under-estimation of medical cost.
In summary, the incidence of APN increased in Korea during 2010–2014. Approximately 11 times more women were diagnosed and treated with APN than men, and one of every four patients was hospitalized. The overall recurrence rate was 15.8%, and the median duration from a sporadic episode to the first recurrence was 44 days. The probability of recurrence increased with the number of previous recurrences. The overall average medical cost among inpatients was USD 1,144, which was 13 times higher than that among outpatients. Collectively, these findings demonstrate that the epidemiology of APN has been changing in Korea.







 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download