1. Chung KB, Lee EY, Im JP, Han SK, Yim JJ. Clinical characteristics and treatment responses of patients who developed tuberculosis following use of a tumor necrosis factor-α inhibitor. Korean J Intern Med. 2013; 28(2):174–179.

2. Shim TS. Diagnosis and treatment of latent tuberculosis infection due to initiation of anti-TNF therapy. Tuberc Respir Dis (Seoul). 2014; 76(6):261–268.

3. British Thoracic Society Standards of Care Committee. BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-alpha treatment. Thorax. 2005; 60(10):800–805.
4. Rampton DS. Preventing TB in patients with Crohn's disease needing infliximab or other anti-TNF therapy. Gut. 2005; 54(10):1360–1362.

5. Carmona L, Gómez-Reino JJ, Rodríguez-Valverde V, Montero D, Pascual-Gómez E, Mola EM, et al. Effectiveness of recommendations to prevent reactivation of latent tuberculosis infection in patients treated with tumor necrosis factor antagonists. Arthritis Rheum. 2005; 52(6):1766–1772.

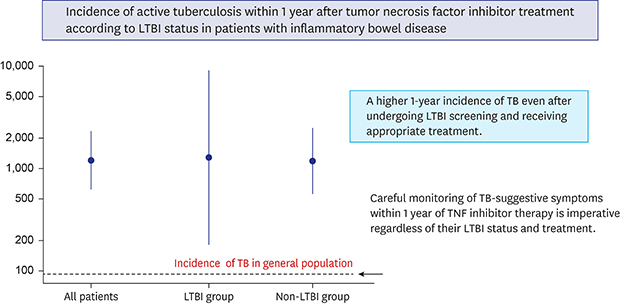
6. Lee EH, Kang YA, Leem AY, Park MS, Kim YS, Kim SK, et al. Active tuberculosis incidence and characteristics in patients treated with tumor necrosis factor antagonists according to latent tuberculosis infection. Sci Rep. 2017; 7(1):6473.

7. Byun JM, Lee CK, Rhee SY, Kim HJ, Kim JW, Shim JJ, et al. The risk of tuberculosis in Korean patients with inflammatory bowel disease receiving tumor necrosis factor-α blockers. J Korean Med Sci. 2015; 30(2):173–179.

8. Lee JW, Choi CH, Park JH, Kim JW, Kang SB, Koo JS, et al. Clinical features of active tuberculosis that developed during anti-tumor necrosis factor therapy in patients with inflammatory bowel disease. Intest Res. 2016; 14(2):146–151.

9. Jung YJ, Lee JY, Jo KW, Yoo B, Lee CK, Kim YG, et al. The ‘either test positive’ strategy for latent tuberculous infection before anti-tumour necrosis factor treatment. Int J Tuberc Lung Dis. 2014; 18(4):428–434.

10. Kim JH, Yim JJ. Achievements in and challenges of tuberculosis control in South Korea. Emerg Infect Dis. 2015; 21(11):1913–1920.

11. Lee SH. Diagnosis and treatment of latent tuberculosis infection. Tuberc Respir Dis (Seoul). 2015; 78(2):56–63.

12. Mori T, Sakatani M, Yamagishi F, Takashima T, Kawabe Y, Nagao K, et al. Specific detection of tuberculosis infection: an interferon-gamma-based assay using new antigens. Am J Respir Crit Care Med. 2004; 170(1):59–64.
13. Park SJ, Jo KW, Yoo B, Lee CK, Kim YG, Yang SK, et al. Comparison of LTBI treatment regimens for patients receiving anti-tumour necrosis factor therapy. Int J Tuberc Lung Dis. 2015; 19(3):342–348.

14. Galloway JB, Hyrich KL, Mercer LK, Dixon WG, Fu B, Ustianowski AP, et al. Anti-TNF therapy is associated with an increased risk of serious infections in patients with rheumatoid arthritis especially in the first 6 months of treatment: updated results from the British Society for Rheumatology Biologics Register with special emphasis on risks in the elderly. Rheumatology (Oxford). 2011; 50(1):124–131.

15. Scrivo R, Armignacco O. Tuberculosis risk and anti-tumour necrosis factor agents in rheumatoid arthritis: a critical appraisal of national registry data. Int J Rheum Dis. 2014; 17(7):716–724.

16. Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis in Korea 2014. Updated 2015. Accessed October 30, 2017.
http://tbzero.cdc.go.kr/tbzero/main.do.
17. St-Pierre J, Chadee K. How the discovery of TNF-α has advanced gastrointestinal diseases and treatment regimes. Dig Dis Sci. 2014; 59(4):712–715.

18. Mañosa M, Domènech E, Cabré E. Current incidence of active tuberculosis in IBD patients treated with anti-TNF agents: still room for improvement. J Crohns Colitis. 2013; 7(10):e499–e500.

19. Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD, et al. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001; 345(15):1098–1104.
20. Askling J, Fored CM, Brandt L, Baecklund E, Bertilsson L, Cöster L, et al. Risk and case characteristics of tuberculosis in rheumatoid arthritis associated with tumor necrosis factor antagonists in Sweden. Arthritis Rheum. 2005; 52(7):1986–1992.

21. Chen DY, Shen GH, Chen YM, Chen HH, Hsieh CW, Lan JL. Biphasic emergence of active tuberculosis in rheumatoid arthritis patients receiving TNFα inhibitors: the utility of IFNγ assay. Ann Rheum Dis. 2012; 71(2):231–237.

22. Lee SK, Kim SY, Kim EY, Jung JY, Park MS, Kim YS, et al. Mycobacterial infections in patients treated with tumor necrosis factor antagonists in South Korea. Lung. 2013; 191(5):565–571.

23. Sichletidis L, Settas L, Spyratos D, Chloros D, Patakas D. Tuberculosis in patients receiving anti-TNF agents despite chemoprophylaxis. Int J Tuberc Lung Dis. 2006; 10(10):1127–1132.
24. Parra Ruiz J, Ortego Centeno N, Raya Alvarez E. Development of tuberculosis in a patient treated with infliximab who had received prophylactic therapy with isoniazid. J Rheumatol. 2003; 30(7):1657–1658.
25. Keane J. TNF-blocking agents and tuberculosis: new drugs illuminate an old topic. Rheumatology (Oxford). 2005; 44(6):714–720.

26. Erkens CG, Slump E, Verhagen M, Schimmel H, de Vries G, Cobelens F, et al. Monitoring latent tuberculosis infection diagnosis and management in the Netherlands. Eur Respir J. 2016; 47(5):1492–1501.

27. Debeuckelaere C, De Munter P, Van Bleyenbergh P, De Wever W, Van Assche G, Rutgeerts P, et al. Tuberculosis infection following anti-TNF therapy in inflammatory bowel disease, despite negative screening. J Crohns Colitis. 2014; 8(6):550–557.

28. Goletti D, Sanduzzi A, Delogu G. Performance of the tuberculin skin test and interferon-γ release assays: an update on the accuracy, cutoff stratification, and new potential immune-based approaches. J Rheumatol Suppl. 2014; 91:24–31.

29. Wong SH, Gao Q, Tsoi KK, Wu WK, Tam LS, Lee N, et al. Effect of immunosuppressive therapy on interferon γ release assay for latent tuberculosis screening in patients with autoimmune diseases: a systematic review and meta-analysis. Thorax. 2016; 71(1):64–72.

30. Edwards A, Gao Y, Allan RN, Ball D, de Graaf H, Coelho T, et al. Corticosteroids and infliximab impair the performance of interferon-γ release assays used for diagnosis of latent tuberculosis. Thorax. 2017; 72(10):946–949.

31. Pai M, Denkinger CM, Kik SV, Rangaka MX, Zwerling A, Oxlade O, et al. Gamma interferon release assays for detection of Mycobacterium tuberculosis infection. Clin Microbiol Rev. 2014; 27(1):3–20.
32. Taxonera C, Ponferrada Á, Bermejo F, Riestra S, Saro C, Martín-Arranz MD, et al. Early tuberculin skin test for the diagnosis of latent tuberculosis infection in patients with inflammatory bowel disease. J Crohns Colitis. 2017; 11(7):792–800.
33. Cantini F, Niccoli L, Goletti D. Adalimumab, etanercept, infliximab, and the risk of tuberculosis: data from clinical trials, national registries, and postmarketing surveillance. J Rheumatol Suppl. 2014; 91:47–55.






 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download