1. Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004; 351(13):1296–1305.

2. Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV, et al. Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. 2006; 7(9):735–740.

3. Campbell SC, Novick AC, Belldegrun A, Blute ML, Chow GK, Derweesh IH, et al. Guideline for management of the clinical T1 renal mass. J Urol. 2009; 182(4):1271–1279.

4. Ljungberg B, Cowan NC, Hanbury DC, Hora M, Kuczyk MA, Merseburger AS, et al. EAU guidelines on renal cell carcinoma: the 2010 update. Eur Urol. 2010; 58(3):398–406.

5. Motzer RJ, Agarwal N, Beard C, Bolger GB, Boston B, Carducci MA, et al. NCCN clinical practice guidelines in oncology: kidney cancer. J Natl Compr Canc Netw. 2009; 7(6):618–630.
6. Huang WC, Elkin EB, Levey AS, Jang TL, Russo P. Partial nephrectomy versus radical nephrectomy in patients with small renal tumors--is there a difference in mortality and cardiovascular outcomes? J Urol. 2009; 181(1):55–61.

7. Sun M, Trinh QD, Bianchi M, Hansen J, Hanna N, Abdollah F, et al. A non-cancer-related survival benefit is associated with partial nephrectomy. Eur Urol. 2012; 61(4):725–731.

8. Kim SP, Thompson RH, Boorjian SA, Weight CJ, Han LC, Murad MH, et al. Comparative effectiveness for survival and renal function of partial and radical nephrectomy for localized renal tumors: a systematic review and meta-analysis. J Urol. 2012; 188(1):51–57.

9. Zini L, Perrotte P, Capitanio U, Jeldres C, Shariat SF, Antebi E, et al. Radical versus partial nephrectomy: effect on overall and noncancer mortality. Cancer. 2009; 115(7):1465–1471.
10. Tan HJ, Norton EC, Ye Z, Hafez KS, Gore JL, Miller DC. Long-term survival following partial vs radical nephrectomy among older patients with early-stage kidney cancer. JAMA. 2012; 307(15):1629–1635.

11. Capitanio U, Terrone C, Antonelli A, Minervini A, Volpe A, Furlan M, et al. Nephron-sparing techniques independently decrease the risk of cardiovascular events relative to radical nephrectomy in patients with a T1a-T1b renal mass and normal preoperative renal function. Eur Urol. 2015; 67(4):683–689.

12. Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H. Renal function after nephron-sparing surgery versus radical nephrectomy: results from EORTC randomized trial 30904. Eur Urol. 2014; 65(2):372–377.

13. Shuch B, Hanley J, Lai J, Vourganti S, Kim SP, Setodji CM, et al. Overall survival advantage with partial nephrectomy: a bias of observational data? Cancer. 2013; 119(16):2981–2989.

14. Lane BR, Campbell SC, Demirjian S, Fergany AF. Surgically induced chronic kidney disease may be associated with a lower risk of progression and mortality than medical chronic kidney disease. J Urol. 2013; 189(5):1649–1655.

15. Van Poppel H, Da Pozzo L, Albrecht W, Matveev V, Bono A, Borkowski A, et al. A prospective, randomised EORTC intergroup phase 3 study comparing the oncologic outcome of elective nephron-sparing surgery and radical nephrectomy for low-stage renal cell carcinoma. Eur Urol. 2011; 59(4):543–552.

16. Byun SS, Hong SK, Lee S, Kook HR, Lee E, Kim HH, et al. The establishment of KORCC (KOrean Renal Cell Carcinoma) database. Investig Clin Urol. 2016; 57(1):50–57.

17. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D, et al. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med. 1999; 130(6):461–470.

18. Chung JS, Son NH, Byun SS, Lee SE, Hong SK, Jeong CW, et al. Trends in renal function after radical nephrectomy: a multicentre analysis. BJU Int. 2014; 113(3):408–415.

19. Woldu SL, Weinberg AC, Korets R, Ghandour R, Danzig MR, RoyChoudhury A, et al. Who really benefits from nephron-sparing surgery? Urology. 2014; 84(4):860–867.

20. Sun M, Bianchi M, Trinh QD, Hansen J, Abdollah F, Hanna N, et al. Comparison of partial vs radical nephrectomy with regard to other-cause mortality in T1 renal cell carcinoma among patients aged ≥75 years with multiple comorbidities. BJU Int. 2013; 111(1):67–73.

21. Larcher A, Capitanio U, Terrone C, Volpe A, De Angelis P, Dehó F, et al. Elective nephron sparing surgery decreases other cause mortality relative to radical nephrectomy only in specific subgroups of patients with renal cell carcinoma. J Urol. 2016; 196(4):1008–1013.

22. An JY, Ball MW, Gorin MA, Hong JJ, Johnson MH, Pavlovich CP, et al. Partial vs radical nephrectomy for T1-T2 renal masses in the elderly: comparison of complications, renal function, and oncologic outcomes. Urology. 2017; 100:151–157.

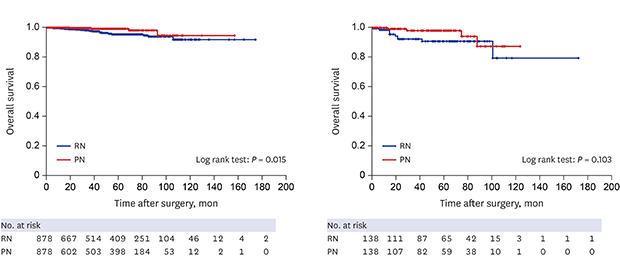
23. Chung JS, Son NH, Lee SE, Hong SK, Lee SC, Kwak C, et al. Overall survival and renal function after partial and radical nephrectomy among older patients with localised renal cell carcinoma: a propensity-matched multicentre study. Eur J Cancer. 2015; 51(4):489–497.

24. Kopp RP, Mehrazin R, Palazzi KL, Liss MA, Jabaji R, Mirheydar HS, et al. Survival outcomes after radical and partial nephrectomy for clinical T2 renal tumours categorised by R.E.N.A.L. nephrometry score. BJU Int. 2014; 114(5):708–718.

25. Badalato GM, Kates M, Wisnivesky JP, Choudhury AR, McKiernan JM. Survival after partial and radical nephrectomy for the treatment of stage T1bN0M0 renal cell carcinoma (RCC) in the USA: a propensity scoring approach. BJU Int. 2012; 109(10):1457–1462.







 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download