1. Keates RH, Pearce JL, Schneider RT. Clinical results of the multifocal lens. J Cataract Refract Surg. 1987; 13(5):557–560.

2. Calladine D, Evans JR, Shah S, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Sao Paulo Med J. 2015; 133(1):68.

3. Shah S, Peris-Martinez C, Reinhard T, Vinciguerra P. Visual outcomes after cataract surgery: multifocal versus monofocal intraocular lenses. J Refract Surg. 2015; 31(10):658–666.

4. Lane SS, Morris M, Nordan L, Packer M, Tarantino N, Wallace RB 3rd. Multifocal intraocular lenses. Ophthalmol Clin North Am. 2006; 19(1):89–105.
5. Voskresenskaya A, Pozdeyeva N, Pashtaev N, Batkov Y, Treushnicov V, Cherednik V. Initial results of trifocal diffractive IOL implantation. Graefes Arch Clin Exp Ophthalmol. 2010; 248(9):1299–1306.

6. Gatinel D, Pagnoulle C, Houbrechts Y, Gobin L. Design and qualification of a diffractive trifocal optical profile for intraocular lenses. J Cataract Refract Surg. 2011; 37(11):2060–2067.

7. Montés-Micó R, Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, Pons AM. In vitro optical quality differences between multifocal apodized diffractive intraocular lenses. J Cataract Refract Surg. 2013; 39(6):928–936.

8. Madrid-Costa D, Ruiz-Alcocer J, Ferrer-Blasco T, García-Lázaro S, Montés-Micó R. Optical quality differences between three multifocal intraocular lenses: bifocal low add, bifocal moderate add, and trifocal. J Refract Surg. 2013; 29(11):749–754.

9. Papadatou E, Del Águila-Carrasco AJ, Esteve-Taboada JJ, Madrid-Costa D, Montés-Micó R. Assessing the in vitro optical quality of presbyopic solutions based on the axial modulation transfer function. J Cataract Refract Surg. 2016; 42(5):780–787.

10. Brito P, Salgado-Borges J, Neves H, Gonzalez-Meijome J, Monteiro M. Light-distortion analysis as a possible indicator of visual quality after refractive lens exchange with diffractive multifocal intraocular lenses. J Cataract Refract Surg. 2015; 41(3):613–622.

11. Jonker SM, Bauer NJ, Makhotkina NY, Berendschot TT, van den Biggelaar FJ, Nuijts RM. Comparison of a trifocal intraocular lens with a +3.0 D bifocal IOL: results of a prospective randomized clinical trial. J Cataract Refract Surg. 2015; 41(8):1631–1640.

12. Gundersen KG, Potvin R. Comparison of visual outcomes after implantation of diffractive trifocal toric intraocular lens and a diffractive apodized bifocal toric intraocular lens. Clin Ophthalmol. 2016; 10:455–461.
13. Mojzis P, Kukuckova L, Majerova K, Liehneova K, Piñero DP. Comparative analysis of the visual performance after cataract surgery with implantation of a bifocal or trifocal diffractive IOL. J Refract Surg. 2014; 30(10):666–672.

14. Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014; 14(1):135.

15. Sistrom CL, Mergo PJ. A simple method for obtaining original data from published graphs and plots. AJR Am J Roentgenol. 2000; 174(5):1241–1244.

16. Shinichi A. Cochrane handbook for systematic reviews of interventions. Online Kensaku. 2014; 35(3):154–155.
18. Chinn S. A simple method for converting an odds ratio to effect size for use in meta-analysis. Stat Med. 2000; 19(22):3127–3131.

19. Postolache C, Postolache O. Comparation of refractive results with bifocal implants at Lisa 809 and trifocal at Lisa tri839. Rom J Ophthalmol. 2015; 59(2):100–102.
20. Alió JL, Kaymak H, Breyer D, Cochener B, Plaza-Puche AB. Quality of life related variables measured for three multifocal diffractive intraocular lenses: a prospective randomised clinical trial. Clin Exp Ophthalmol. 2018; 46(4):380–388.

21. Kaymak H, Breyer D, Alió JL, Cochener B. Visual performance with bifocal and trifocal diffractive intraocular lenses: a prospective three-armed randomized multicenter clinical trial. J Refract Surg. 2017; 33(10):655–662.

22. Mojzis P, Kukuckova L, Majerova K, Ziak P, Piñero DP. Postoperative visual performance with a bifocal and trifocal diffractive intraocular lens during a 1-year follow-up. Int J Ophthalmol. 2017; 10(10):1528–1533.

23. Bilbao-Calabuig R, González-López F, Amparo F, Alvarez G, Patel SR, Llovet-Osuna F. Comparison between mix-and-match implantation of bifocal intraocular lenses and bilateral implantation of trifocal intraocular lenses. J Refract Surg. 2016; 32(10):659–663.

24. Cochener B. Prospective clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses. J Refract Surg. 2016; 32(3):146–151.

25. Plaza-Puche AB, Alio JL. Analysis of defocus curves of different modern multifocal intraocular lenses. Eur J Ophthalmol. 2016; 26(5):412–417.

26. Vilar C, Hida WT, de Medeiros AL, Magalhães KRP, de Moraes Tzelikis PF, Chaves MAPD, et al. Comparison between bilateral implantation of a trifocal intraocular lens and blended implantation of two bifocal intraocular lenses. Clin Ophthalmol. 2017; 11:1393–1397.
27. Gundersen KG, Potvin R. Comparison of visual outcomes and subjective visual quality after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of apodized diffractive bifocal intraocular lenses. Clin Ophthalmol. 2016; 10:805–811.
28. Plaza-Puche AB, Alio JL, Sala E, Mojzis P. Impact of low mesopic contrast sensitivity outcomes in different types of modern multifocal intraocular lenses. Eur J Ophthalmol. 2016; 26(6):612–617.

29. Liu JW, Haw WW. Optimizing outcomes of multifocal intraocular lenses. Curr Opin Ophthalmol. 2014; 25(1):44–48.

30. de Vries NE, Webers CA, Montés-Micó R, Ferrer-Blasco T, Nuijts RM. Visual outcomes after cataract surgery with implantation of a +3.00 D or +4.00 D aspheric diffractive multifocal intraocular lens: comparative study. J Cataract Refract Surg. 2010; 36(8):1316–1322.

31. Cochener B, Vryghem J, Rozot P, Lesieur G, Heireman S, Blanckaert JA, et al. Visual and refractive outcomes after implantation of a fully diffractive trifocal lens. Clin Ophthalmol. 2012; 6:1421–1427.

32. Marques EF, Ferreira TB. Comparison of visual outcomes of 2 diffractive trifocal intraocular lenses. J Cataract Refract Surg. 2015; 41(2):354–363.

33. Vinas M, Gonzalez-Ramos A, Dorronsoro C, Akondi V, Garzon N, Poyales F, et al. In vivo measurement of longitudinal chromatic aberration in patients implanted with trifocal diffractive intraocular lenses. J Refract Surg. 2017; 33(11):736–742.

34. Millán MS, Vega F, Ríos-López I. Polychromatic image performance of diffractive bifocal intraocular lenses: longitudinal chromatic aberration and energy efficiency. Invest Ophthalmol Vis Sci. 2016; 57(4):2021–2028.

35. Millán MS, Vega F. Extended depth of focus intraocular lens: chromatic performance. Biomed Opt Express. 2017; 8(9):4294–4309.

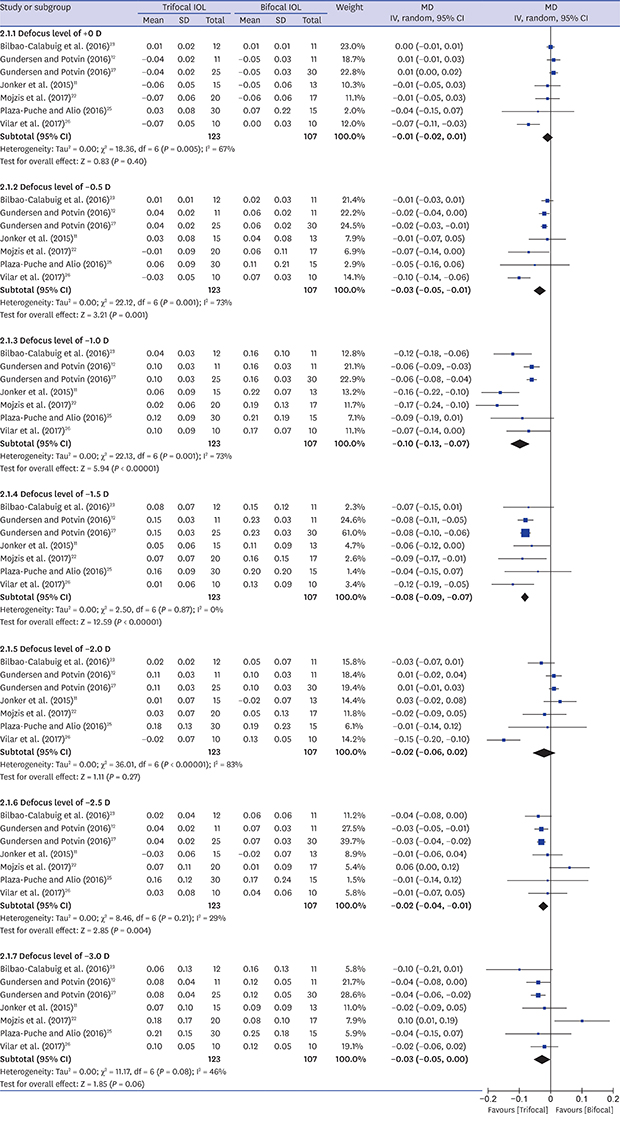
36. Shen Z, Lin Y, Zhu Y, Liu X, Yan J, Yao K. Clinical comparison of patient outcomes following implantation of trifocal or bifocal intraocular lenses: a systematic review and meta-analysis. Sci Rep. 2017; 7(1):45337.

37. de Silva SR, Evans JR, Kirthi V, Ziaei M, Leyland M. Multifocal versus monofocal intraocular lenses after cataract extraction. Cochrane Database Syst Rev. 2016; 12:CD003169.

38. Chiam PJ, Chan JH, Aggarwal RK, Kasaby S. ReSTOR intraocular lens implantation in cataract surgery: quality of vision. J Cataract Refract Surg. 2006; 32(9):1459–1463.

39. de Vries NE, Webers CA, Touwslager WR, Bauer NJ, de Brabander J, Berendschot TT, et al. Dissatisfaction after implantation of multifocal intraocular lenses. J Cataract Refract Surg. 2011; 37(5):859–865.

40. Cetinkaya S, Dadaci Z, Acir NO, Cetinkaya YF, Yener HI, Ozcimen M. Visual outcomes of multifocal intraocular lens implantation in patients with cataract and high hyperopia and patient selection. Int J Ophthalmol. 2015; 8(6):1258–1260.
41. Xu Z, Cao D, Chen X, Wu S, Wang X, Wu Q. Comparison of clinical performance between trifocal and bifocal intraocular lenses: a meta-analysis. PLoS One. 2017; 12(10):e0186522.









 PDF
PDF Citation
Citation Print
Print




 XML Download
XML Download