1. Lee SH, Chai JY, Seo BS, Cho SY. Two cases of human infection by adult of Spirometra erinacei. Korean J Parasitol. 1984; 22(1):66–71.
2. Weinstein PP, Krawczyk HJ, Peers JH. Sparganosis in Korea. Am J Trop Med Hyg. 1954; 3(1):112–129. PMID:
13114596.

3. Cho SY, Bae JH, Seo BS. Some aspects of human sparganosis in Korea. Korean J Parasitol. 1975; 13(1):60–77.

4. Liu Q, Li MW, Wang ZD, Zhao GH, Zhu XQ. Human sparganosis, a neglected food borne zoonosis. Lancet Infect Dis. 2015; 15(10):1226–1235. PMID:
26364132.

5. Bowman DD, Hendrix CM, Lindsay DS, Barr SC. Feline Clinical Parasitology. 1st ed. Ames, IA: Iowa State University Press;2002.
6. Jeon HK, Park H, Lee D, Choe S, Kim KH, Huh S, et al. Human infections with
Spirometra decipiens plerocercoids identified by morphologic and genetic analyses in Korea. Korean J Parasitol. 2015; 53(3):299–305. PMID:
26174823.
7. Kong Y, Cho SY, Kang WS. Sparganum infections in normal adult population and epileptic patients in Korea: a seroepidemiologic observation. Korean J Parasitol. 1994; 32(2):85–92. PMID:
8025037.

8. Lee KJ, Bae YT, Kim DH, Deung YK, Ryang YS. A seroepidemiologic survey for human sparganosis in Gangweon-do. Korean J Parasitol. 2002; 40(4):177–180. PMID:
12509101.

9. Kim H, Kim SI, Cho SY. Serological diagnosis of human sparganosis by means of micro-ELISA. Korean J Parasitol. 1984; 22(2):222–228.

10. Doi T, Boku S. The first case of Sparganum mansoni from a Korean and three cases from Japanese. J Chosen Med Ass. 1924; 50:47–51.
11. Min DY. Cestode infections in Korea. Korean J Parasitol. 1990; 28(Suppl):123–144.

12. Chang KH, Cho SY, Chi JG, Kim WS, Han MC, Kim CW, et al. Cerebral sparganosis: CT characteristics. Radiology. 1987; 165(2):505–510. PMID:
3659374.

13. Chung SY, Park KS, Lee Y, Park CK. Breast sparganosis: mammographic and ultrasound features. J Clin Ultrasound. 1995; 23(7):447–451. PMID:
7560161.

14. Cho SY, Kang SY, Kong Y. Purification of antigenic protein of sparganum by immunoaffinity chromatography using a monoclonal antibody. Korean J Parasitol. 1990; 28(3):135–142.

15. Morakote N, Kong Y. Antigen specificity of 36 and 31 kDa proteins of
Spirometra erinacei plerocercoid in tissue invading nematodiasis. Korean J Parasitol. 1993; 31(2):169–171. PMID:
7688246.
16. Kobayashi H. On the animal parasites in Korea. Jpn Med World. 1925; 5(1):9–16.
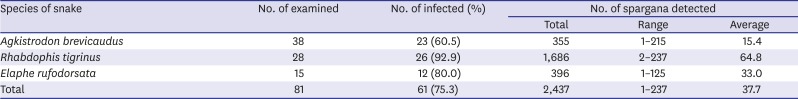
17. Cho SY, Hwang KI, Seo BS. On the Sparganum mansoni infection in some Korean terrestrial snakes. Korean J Parasitol. 1973; 11(2):87–94.
18. Kim CH. The infection status of sparganum and Gnathostoma in frogs of southern part of Korea. Korean J Parasitol. 1983; 21(1):83–86.
19. Mitchell A, Scheithauer BW, Kelly PJ, Forbes GS, Rosenblatt JE. Cerebral sparganosis. Case report. J Neurosurg. 1990; 73(1):147–150. PMID:
2191089.
20. Anantaphruti MT, Nawa Y, Vanvanitchai Y. Human sparganosis in Thailand: an overview. Acta Trop. 2011; 118(3):171–176. PMID:
21459073.

21. Lo Presti A, Aguirre DT, De Andrés P, Daoud L, Fortes J, Muñiz J. Cerebral sparganosis: case report and review of the European cases. Acta Neurochir (Wien). 2015; 157(8):1339–1343. PMID:
26085111.

22. Koo M, Kim JH, Kim JS, Lee JE, Nam SJ, Yang JH. Cases and literature review of breast sparganosis. World J Surg. 2011; 35(3):573–579. PMID:
21203758.

23. Lee EG, Kim WJ, Lee HJ, Lee SE, Yoon MS. Sparganosis in a child. Korean J Dermatol. 2012; 50(12):1087–1088.
24. Lim D, Kim CS, Kim SI. Sparganosis presenting as spermatic cord hydrocele in six-year-old boy. Urology. 2007; 70(6):1223.e1–1223.e2.

25. Kim HY, Kang CH, Kim JH, Lee SH, Park SY, Cho SW. Intramuscular and subcutaneous sparganosis: sonographic findings. J Clin Ultrasound. 2008; 36(9):570–572. PMID:
18431747.

26. Choi SJ, Park SH, Kim MJ, Jung M, Ko BH. Sparganosis of the breast and lower extremities: sonographic appearance. J Clin Ultrasound. 2014; 42(7):436–438. PMID:
24633936.

27. Cho JH, Lee KB, Yong TS, Kim BS, Park HB, Ryu KN, et al. Subcutaneous and musculoskeletal sparganosis: imaging characteristics and pathologic correlation. Skeletal Radiol. 2000; 29(7):402–408. PMID:
10963426.

28. Ha S, Oh SW, Kim YK, Yi A, Ahn YJ. Breast sparganosis incidentally detected by FDG PET/CT. Nucl Med Mol Imaging. 2013; 47(2):130–133. PMID:
24900094.

29. Yoo H, Kim DG. Sparganosis of brain and lumbar spinal canal. J Korean Neurosurg Soc. 1999; 28(7):1027–1031.
30. Chang KH, Chi JG, Cho SY, Han MH, Han DH, Han MC. Cerebral sparganosis: analysis of 34 cases with emphasis on CT features. Neuroradiology. 1992; 34(1):1–8. PMID:
1553030.

31. Moon WK, Chang KH, Cho SY, Han MH, Cha SH, Chi JG, et al. Cerebral sparganosis: MR imaging versus CT features. Radiology. 1993; 188(3):751–757. PMID:
8351344.

32. Kim HW, Kim JH. A case of sparganosis infesting with stone in human ureter. Korean J Urol. 1970; 11(1):23–26.
33. Kim DH, Yi IH, Youn HC, Kim SC, Kim BS, Cho KS, et al. Pleural sparganosis: a case report. Korean J Thorac Cardiovasc Surg. 2006; 39(6):502–503.
34. Lee JH, Yu JS, Park MS, Lee SI, Yang SW. Abdominal sparganosis presenting as an abscess with fistulous communication to the bowel. AJR Am J Roentgenol. 2005; 185(4):1084–1085. PMID:
16177444.

35. Park WH, Shin TY, Yoon SM, Park SH, Kang YJ, Kim DK, et al. A case report of testicular sparganosis misdiagnosed as testicular tumor. J Korean Med Sci. 2014; 29(7):1018–1020. PMID:
25045238.

36. Lee JH, Kim GH, Kim SM, Lee SY, Lee WY, Bae JW, et al. A case of sparganosis that presented as a recurrent pericardial effusion. Korean Circ J. 2011; 41(1):38–42. PMID:
21359068.

37. Shin JH, Chung JK, Kim WB, Kim DJ, Ok YC, Lee KW. A case report of sparganosis of the orbit. J Korean Neurosurg Soc. 1975; 4(2):409–412.
38. Song EJ, Sohn YM, Ryu KN, Min SY, Shin SH, Park YK. Breast sparganosis and incidentally detected subcutaneous and intramuscular sparganosis at several sites: case report and literature review. Jpn J Radiol. 2015; 33(4):225–228. PMID:
25725936.

39. Connor DH, Sparks AK, Strano AJ, Neafie RC, Juvelier B. Disseminated parasitosis in an immunosuppressed patient. Possibly a mutated sparganum. Arch Pathol Lab Med. 1976; 100(2):65–68. PMID:
803199.
40. Olson PD, Yoder K, Fajardo L-G LF, Marty AM, van de Pas S, Olivier C, et al. Lethal invasive cestodiasis in immunosuppressed patients. J Infect Dis. 2003; 187(12):1962–1966. PMID:
12792874.

41. Meric R, Ilie MI, Hofman V, Rioux-Leclercq N, Michot L, Haffaf Y, et al. Disseminated infection caused by
Sparganum proliferum in an AIDS patient. Histopathology. 2010; 56(6):824–828. PMID:
20546351.
42. Lee YJ, Choo KS, Bae YT, Kim JY. A case report of breast sparganosis in a patient with ipsilateral breast cancer: MRI and ultrasonographic findings. J Korean Soc Radiol. 2010; 63(6):569–575.

43. Yeo JY, Han JY, Lee JH, Park YH, Lim JH, Lee MH, et al. A case of inguinal sparganosis mimicking myeloid sarcoma. Korean J Parasitol. 2012; 50(4):353–355. PMID:
23230335.

44. Chun SM, Yun SJ, Lee JB, Lee SC, Won YH, Kim SJ. A case of sparganosis in a patient with rectal cancer. Korean J Dermatol. 2012; 50(4):332–336.
45. Roh SY, Lee JY, Park KW, Jung SN. Sparganosis in a patient with diffuse large B cell lymphoma. J Cancer Res Ther. 2013; 9(4):712–714. PMID:
24518723.

46. Lee JS, Park SJ, Park MI, Kim KJ, Moon W, Shin EK, et al. A case of sparganosis mimicking a skin metastasis in a patient with stomach cancer. Korean J Med. 2009; 77(6):755–758.
47. Lee EK, Yoo YB. Axillary sparganosis which was misunderstood lymph node metastasis during neoadjuvant chemotheraphy in a breast cancer patient. Ann Surg Treat Res. 2014; 87(6):336–339. PMID:
25485243.

48. Kong Y, Chung YB, Cho SY, Choi SH, Kang SY. Characterization of three neutral proteases of
Spirometra mansoni plerocercoid. Parasitology. 1994; 108(Pt 3):359–368. PMID:
8022661.
49. Kong Y, Chung YB, Cho SY, Kang SY. Cleavage of immunoglobulin G by excretory-secretory cathepsin S-like protease of
Spirometra mansoni plerocercoid. Parasitology. 1994; 109(Pt 5):611–621. PMID:
7831096.
50. Cho BK, Chun CS, Choi WY, Cho SY. A case of unusual sparganosis. Korean J Dermatol. 1985; 23(5):672–677.
51. Torres JR, Noya OO, Noya BA, Mouliniere R, Martinez E. Treatment of proliferative sparganosis with mebendazole and praziquantel. Trans R Soc Trop Med Hyg. 1981; 75(6):846–847. PMID:
7330947.

52. Moulinier R, Martinez E, Torres J, Noya O, de NOya BA, Reyes O. Human proliferative sparganosis in Venezuela: report of a case. Am J Trop Med Hyg. 1982; 31(2):358–363. PMID:
7072899.
53. Lo YK, Chao D, Yan SH, Liu HC, Chu FL, Huang CI, et al. Spinal cord proliferative sparganosis in Taiwan: a case report. Neurosurgery. 1987; 21(2):235–238. PMID:
3309711.

54. Nakamura T, Hara M, Matsuoka M, Kawabata M, Tsuji M. Human proliferative sparganosis. A new Japanese case. Am J Clin Pathol. 1990; 94(2):224–228. PMID:
2196778.

55. Jeon HK, Park H, Lee D, Choe S, Sohn WM, Eom KS. Molecular detection of
Spirometra decipiens in the United States. Korean J Parasitol. 2016; 54(4):503–507. PMID:
27658603.
56. Jeon HK, Park H, Lee D, Choe S, Kim KH, Sohn WM, et al. Genetic identification of
Spirometra decipiens plerocercoids in terrestrial snakes from Korea and China. Korean J Parasitol. 2016; 54(2):181–185. PMID:
27180576.
57. Faust EC, Campbell HE, Kellogg CR. Morphological and biological studies on the species of Diphyllobothrium in China. Am J Hyg. 1929; 9(3):560–583.
58. Wittner M, Tanowitz HB. Other cestode infection. In : Guerrant RL, Walker DH, Weller PF, editors. Essentials of Tropical Infectious Disease. New York, NY: Churchill Livingstone;2001. p. 490–491.




 PDF
PDF Citation
Citation Print
Print



 XML Download
XML Download