1. Bonomo RA, Burd EM, Conly J, Limbago BM, Poirel L, Segre JA, et al. Carbapenemase-producing organisms: a global scourge. Clin Infect Dis. 2018; 66(8):1290–1297.

2. van Duin D, Doi Y. The global epidemiology of carbapenemase-producing Enterobacteriaceae
. Virulence. 2017; 8(4):460–469.
3. Glasner C, Albiger B, Buist G, Tambić Andrasević A, Canton R, Carmeli Y, et al. Carbapenemase-producing
Enterobacteriaceae in Europe: a survey among national experts from 39 countries, February 2013. Euro Surveill. 2013; 18(28):20525.

4. Albiger B, Glasner C, Struelens MJ, Grundmann H, Monnet DL. European Survey of Carbapenemase-Producing
Enterobacteriaceae (EuSCAPE) working group. Carbapenemase-producing
Enterobacteriaceae in Europe: assessment by national experts from 38 countries, May 2015. Euro Surveill. 2015; 20(45):30062.

6. Papp-Wallace KM, Endimiani A, Taracila MA, Bonomo RA. Carbapenems: past, present, and future. Antimicrob Agents Chemother. 2011; 55(11):4943–4960.

8. Codjoe FS, Donkor ES. Carbapenem resistance: a review. Med Sci (Basel). 2017; 6(1):1–8.

9. Nordmann P, Cuzon G, Naas T. The real threat of Klebsiella pneumoniae carbapenemase-producing bacteria. Lancet Infect Dis. 2009; 9(4):228–236.
10. Cuzon G, Naas T, Truong H, Villegas MV, Wisell KT, Carmeli Y, et al. Worldwide diversity of Klebsiella pneumoniae that produce beta-lactamase blaKPC-2 gene. Emerg Infect Dis. 2010; 16(9):1349–1356.
11. Nordmann P, Naas T, Poirel L. Global spread of carbapenemase-producing Enterobacteriaceae
. Emerg Infect Dis. 2011; 17(10):1791–1798.
12. Evans BA, Amyes SG. OXA β-lactamases. Clin Microbiol Rev. 2014; 27(2):241–263.

13. Mathers AJ, Hazen KC, Carroll J, Yeh AJ, Cox HL, Bonomo RA, et al. First clinical cases of OXA-48-producing carbapenem-resistant Klebsiella pneumoniae in the United States: the “menace” arrives in the new world. J Clin Microbiol. 2013; 51(2):680–683.
14. Carrër A, Poirel L, Yilmaz M, Akan OA, Feriha C, Cuzon G, et al. Spread of OXA-48-encoding plasmid in Turkey and beyond. Antimicrob Agents Chemother. 2010; 54(3):1369–1373.

15. Ma L, Wang JT, Wu TL, Siu LK, Chuang YC, Lin JC, et al. Emergence of OXA-48-Producing Klebsiella pneumoniae in Taiwan. PLoS One. 2015; 10(9):e0139152.
16. Queenan AM, Bush K. Carbapenemases: the versatile beta-lactamases. Clin Microbiol Rev. 2007; 20(3):440–458.
17. Walsh TR, Toleman MA, Poirel L, Nordmann P. Metallo-beta-lactamases: the quiet before the storm? Clin Microbiol Rev. 2005; 18(2):306–325.
18. Jamal W, Rotimi VO, Albert MJ, Khodakhast F, Nordmann P, Poirel L. High prevalence of VIM-4 and NDM-1 metallo-β-lactamase among carbapenem-resistant Enterobacteriaceae. J Med Microbiol. 2013; 62(Pt 8):1239–1244.
19. Lee K, Yum JH, Yong D, Lee HM, Kim HD, Docquier JD, et al. Novel acquired metallo-beta-lactamase gene, bla(SIM-1), in a class 1 integron from Acinetobacter baumannii clinical isolates from Korea. Antimicrob Agents Chemother. 2005; 49(11):4485–4491.
20. Nordmann P, Poirel L. The difficult-to-control spread of carbapenemase producers among Enterobacteriaceae worldwide. Clin Microbiol Infect. 2014; 20(9):821–830.
21. Cuzon G, Naas T, Nordmann P. Functional characterization of Tn4401, a Tn3-based transposon involved in blaKPC gene mobilization. Antimicrob Agents Chemother. 2011; 55(11):5370–5373.
22. Berger S, Alauzet C, Aissa N, Hénard S, Rabaud C, Bonnet R, et al. Characterization of a new blaOXA-48-carrying plasmid in Enterobacteriaceae
. Antimicrob Agents Chemother. 2013; 57(8):4064–4067.
23. Gasink LB, Edelstein PH, Lautenbach E, Synnestvedt M, Fishman NO. Risk factors and clinical impact of Klebsiella pneumoniae carbapenemase-producing K. pneumoniae. Infect Control Hosp Epidemiol. 2009; 30(12):1180–1185.
24. Xiao T, Yu W, Niu T, Huang C, Xiao Y. A retrospective, comparative analysis of risk factors and outcomes in carbapenem-susceptible and carbapenem-nonsusceptible Klebsiella pneumoniae bloodstream infections: tigecycline significantly increases the mortality. Infect Drug Resist. 2018; 11:595–606.
25. Zilberberg MD, Nathanson BH, Sulham K, Fan W, Shorr AF. Carbapenem resistance, inappropriate empiric treatment and outcomes among patients hospitalized with
Enterobacteriaceae urinary tract infection, pneumonia and sepsis. BMC Infect Dis. 2017; 17(1):279.

26. Wang Q, Zhang Y, Yao X, Xian H, Liu Y, Li H, et al. Risk factors and clinical outcomes for carbapenem-resistant Enterobacteriaceae nosocomial infections. Eur J Clin Microbiol Infect Dis. 2016; 35(10):1679–1689.
27. McConville TH, Sullivan SB, Gomez-Simmonds A, Whittier S, Uhlemann AC. Carbapenem-resistant Enterobacteriaceae colonization (CRE) and subsequent risk of infection and 90-day mortality in critically ill patients, an observational study. PLoS One. 2017; 12(10):e0186195.
28. van Duin D, Kaye KS, Neuner EA, Bonomo RA. Carbapenem-resistant Enterobacteriaceae: a review of treatment and outcomes. Diagn Microbiol Infect Dis. 2013; 75(2):115–120.
29. Patel G, Huprikar S, Factor SH, Jenkins SG, Calfee DP. Outcomes of carbapenem-resistant Klebsiella pneumoniae infection and the impact of antimicrobial and adjunctive therapies. Infect Control Hosp Epidemiol. 2008; 29(12):1099–1106.
30. Tamma PD, Goodman KE, Harris AD, Tekle T, Roberts A, Taiwo A, et al. Comparing the outcomes of patients with carbapenemase-producing and non-carbapenemase-producing carbapenem-resistant Enterobacteriaceae bacteremia. Clin Infect Dis. 2017; 64(3):257–264.
31. Seo YH, Jeong JH, Lee HT, Kwoun WJ, Park PW, Ahn JY, et al. Analysis of blood culture data at a tertiary university hospital, 2006–2015. Ann Clin Microbiol. 2017; 20(2):35–41.

32. Jeong SH, Kim HS, Kim JS, Shin DH, Kim HS, Park MJ, et al. Prevalence and molecular characteristics of carbapenemase-producing Enterobacteriaceae from five hospitals in Korea. Ann Lab Med. 2016; 36(6):529–535.
33. Yoon EJ, Kim JO, Kim D, Lee H, Yang JW, Lee KJ, et al.
Klebsiella pneumoniae carbapenemase producers in South Korea between 2013 and 2015. Front Microbiol. 2018; 9:56.

34. Yoo JH. Principle and perspective of healthcare-associated infection control. J Korean Med Assoc. 2018; 61(1):5–12.

35. Palmore TN, Henderson DK. Managing transmission of carbapenem-resistant Enterobacteriaceae in healthcare settings: a view from the trenches. Clin Infect Dis. 2013; 57(11):1593–1599.
36. van Duin D, Paterson DL. Multidrug-resistant bacteria in the community: trends and lessons learned. Infect Dis Clin North Am. 2016; 30(2):377–390.
37. Burnham JP, Kwon JH, Olsen MA, Babcock HM, Kollef MH. Readmissions with multidrug-resistant infection in patients with prior multidrug resistant infection. Infect Control Hosp Epidemiol. 2018; 39(1):12–19.

38. Magiorakos AP, Burns K, Rodríguez Baño J, Borg M, Daikos G, Dumpis U, et al. Infection prevention and control measures and tools for the prevention of entry of carbapenem-resistant
Enterobacteriaceae into healthcare settings: guidance from the European centre for disease prevention and control. Antimicrob Resist Infect Control. 2017; 6(1):113.

40. Zimmerman FS, Assous MV, Bdolah-Abram T, Lachish T, Yinnon AM, Wiener-Well Y. Duration of carriage of carbapenem-resistant Enterobacteriaceae following hospital discharge. Am J Infect Control. 2013; 41(3):190–194.
41. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. 27th ed. Wayne, PA, USA: Clinical and Laboratory Standards Institute;2017.
42. Aguirre-Quiñonero A, Martínez-Martínez L. Non-molecular detection of carbapenemases in Enterobacteriaceae clinical isolates. J Infect Chemother. 2017; 23(1):1–11.
43. Anderson KF, Lonsway DR, Rasheed JK, Biddle J, Jensen B, McDougal LK, et al. Evaluation of methods to identify the Klebsiella pneumoniae carbapenemase in Enterobacteriaceae
. J Clin Microbiol. 2007; 45(8):2723–2725.
44. Song W, Hong SG, Yong D, Jeong SH, Kim HS, Kim HS, et al. Combined use of the modified Hodge test and carbapenemase inhibition test for detection of carbapenemase-producing Enterobacteriaceae and metallo-β-lactamase-producing Pseudomonas spp. Ann Lab Med. 2015; 35(2):212–219.
45. Lee K, Chong Y, Shin HB, Kim YA, Yong D, Yum JH. Modified Hodge and EDTA-disk synergy tests to screen metallo-beta-lactamase-producing strains of Pseudomonas and Acinetobacter species. Clin Microbiol Infect. 2001; 7(2):88–91.
46. Poirel L, Walsh TR, Cuvillier V, Nordmann P. Multiplex PCR for detection of acquired carbapenemase genes. Diagn Microbiol Infect Dis. 2011; 70(1):119–123.

47. Wilson AP, Livermore DM, Otter JA, Warren RE, Jenks P, Enoch DA, et al. Prevention and control of multi-drug-resistant gram-negative bacteria: recommendations from a joint working party. J Hosp Infect. 2016; 92:Suppl 1. S1–44.
48. CDC. Facility Guidance for Control of Carbapenem-Resistant Enterobacteriaceae (CRE). Atlanta, GA: CDC;2015.
49. Banach DB, Bearman G, Barnden M, Hanrahan JA, Leekha S, Morgan DJ, et al. Duration of contact precautions for acute-care settings. Infect Control Hosp Epidemiol. 2018; 39(2):127–144.

50. Solter E, Adler A, Rubinovitch B, Temkin E, Schwartz D, Ben-David D, et al. Israeli national policy for carbapenem-resistant Enterobacteriaceae screening, carrier isolation and discontinuation of isolation. Infect Control Hosp Epidemiol. 2018; 39(1):85–89.
51. Adler A, Lifshitz Z, Gordon M, Ben-David D, Khabra E, Masarwa S, et al. Evolution and dissemination of the Klebsiella pneumoniae clonal group 258 throughout Israeli post-acute care hospitals, 2008–13. J Antimicrob Chemother. 2017; 72(8):2219–2224.
52. Bart Y, Paul M, Eluk O, Geffen Y, Rabino G, Hussein K. Risk factors for recurrence of carbapenem-resistant Enterobacteriaceae carriage: case-control study. Infect Control Hosp Epidemiol. 2015; 36(8):936–941.
53. Kotay S, Chai W, Guilford W, Barry K, Mathers AJ. Spread from the sink to the patient: in situ study using Green Fluorescent Protein (GFP)-expressing
Escherichia coli to model bacterial dispersion from hand-washing sink-trap reservoirs. Appl Environ Microbiol. 2017; 83(8):e03327-16.

54. Kizny Gordon AE, Mathers AJ, Cheong EY, Gottlieb T, Kotay S, Walker AS, et al. The hospital water environment as a reservoir for carbapenem-resistant organisms causing hospital-acquired infections-a systematic review of the literature. Clin Infect Dis. 2017; 64(10):1435–1444.

55. De Geyter D, Blommaert L, Verbraeken N, Sevenois M, Huyghens L, Martini H, et al. The sink as a potential source of transmission of carbapenemase-producing
Enterobacteriaceae in the intensive care unit. Antimicrob Resist Infect Control. 2017; 6(1):24.

56. Hocquet D, Muller A, Bertrand X. What happens in hospitals does not stay in hospitals: antibiotic-resistant bacteria in hospital wastewater systems. J Hosp Infect. 2016; 93(4):395–402.

57. Barnes SL, Rock C, Harris AD, Cosgrove SE, Morgan DJ, Thom KA. The impact of reducing antibiotics on the transmission of multidrug-resistant organisms. Infect Control Hosp Epidemiol. 2017; 38(6):663–669.

58. Almagor J, Temkin E, Benenson I, Fallach N, Carmeli Y. DRIVE-AB consortium. The impact of antibiotic use on transmission of resistant bacteria in hospitals: Insights from an agent-based model. PLoS One. 2018; 13(5):e0197111.

59. Bassetti M, Peghin M, Pecori D. The management of multidrug-resistant Enterobacteriaceae
. Curr Opin Infect Dis. 2016; 29(6):583–594.
60. Bal BS. An introduction to medical malpractice in the United States. Clin Orthop Relat Res. 2009; 467(2):339–347.

61. Yoo JH. Healthcare-associated infection control on the edge of a ‘carrot-and-stick’ and a ‘crime-and-punishment’ frame. J Korean Med Sci. 2018; 33(8):e83.

63. Gittler GJ, Goldstein EJ. The elements of medical malpractice: an overview. Clin Infect Dis. 1996; 23(5):1152–1155.

64. McQuoid-Mason D. Hospital-acquired infections - when are hospitals legally liable? S Afr Med J. 2012; 102(6 Pt 2):353–354.

65. Yoo HJ. Legislative study on the mitigation of the burden of proof in hospital infection cases - focusing on the revised burgerliches gesetzbuch. Korean Soc Law Med. 2015; 16(2):159–193.
67. Creighton H. Legal aspects of nosocomial infection. Nurs Clin North Am. 1980; 15(4):789–802.
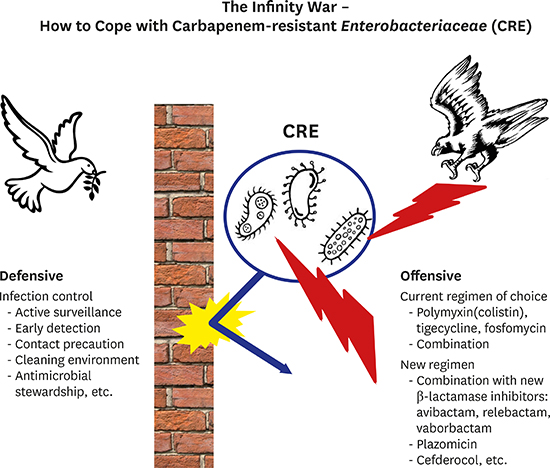
68. Falagas ME, Kasiakou SK, Saravolatz LD. Colistin: the revival of polymyxins for the management of multidrug-resistant gram-negative bacterial infections. Clin Infect Dis. 2005; 40(9):1333–1341.

69. Falagas ME, Kopterides P. Old antibiotics for infections in critically ill patients. Curr Opin Crit Care. 2007; 13(5):592–597.

70. Velkov T, Roberts KD, Nation RL, Thompson PE, Li J. Pharmacology of polymyxins: new insights into an ‘old’ class of antibiotics. Future Microbiol. 2013; 8(6):711–724.

71. Biswas S, Brunel JM, Dubus JC, Reynaud-Gaubert M, Rolain JM. Colistin: an update on the antibiotic of the 21st century. Expert Rev Anti Infect Ther. 2012; 10(8):917–934.

72. Peterson LR. A review of tigecycline--the first glycylcycline. Int J Antimicrob Agents. 2008; 32:Suppl 4. S215–S222.
73. Stein GE, Babinchak T. Tigecycline: an update. Diagn Microbiol Infect Dis. 2013; 75(4):331–336.

74. Sastry S, Doi Y. Fosfomycin: resurgence of an old companion. J Infect Chemother. 2016; 22(5):273–280.

75. Trecarichi EM, Tumbarello M. Therapeutic options for carbapenem-resistant Enterobacteriaceae infections. Virulence. 2017; 8(4):470–484.
76. Papst L, Beovic B, Pulcini C, Durante-Mangoni E, Rodriguez-Bano J, Kaye KS, et al. Antibiotic treatment of infections caused by carbapenem-resistant gram-negative bacilli: an international ESCMID cross-sectional survey among infectious diseases specialists practicing in large hospitals. Clin Microbiol Infect. 2018.
77. Rolinson GN, Geddes AM. The 50th anniversary of the discovery of 6-aminopenicillanic acid (6-APA). Int J Antimicrob Agents. 2007; 29(1):3–8.

78. Hamilton-Miller JM. Development of the semi-synthetic penicillins and cephalosporins. Int J Antimicrob Agents. 2008; 31(3):189–192.

79. Drawz SM, Bonomo RA. Three decades of beta-lactamase inhibitors. Clin Microbiol Rev. 2010; 23(1):160–201.
80. Rotondo CM, Wright GD. Inhibitors of metallo-β-lactamases. Curr Opin Microbiol. 2017; 39:96–105.

81. Wang DY, Abboud MI, Markoulides MS, Brem J, Schofield CJ. The road to avibactam: the first clinically useful non-β-lactam working somewhat like a β-lactam. Future Med Chem. 2016; 8(10):1063–1084.

82. Liscio JL, Mahoney MV, Hirsch EB. Ceftolozane/tazobactam and ceftazidime/avibactam: two novel β-lactam/β-lactamase inhibitor combination agents for the treatment of resistant Gram-negative bacterial infections. Int J Antimicrob Agents. 2015; 46(3):266–271.

83. Olsen I. New promising β-lactamase inhibitors for clinical use. Eur J Clin Microbiol Infect Dis. 2015; 34(7):1303–1308.

84. Papp-Wallace KM, Bonomo RA. New β-Lactamase inhibitors in the clinic. Infect Dis Clin North Am. 2016; 30(2):441–464.

85. Docquier JD, Mangani S. An update on β-lactamase inhibitor discovery and development. Drug Resist Updat. 2018; 36:13–29.

86. Drawz SM, Papp-Wallace KM, Bonomo RA. New β-lactamase inhibitors: a therapeutic renaissance in an MDR world. Antimicrob Agents Chemother. 2014; 58(4):1835–1846.

87. Cho JC, Zmarlicka MT, Shaeer KM, Pardo J. Meropenem/Vaborbactam, the first carbapenem/β-lactamase inhibitor combination. Ann Pharmacother. 2018; 52(8):769–779.

88. Zhanel GG, Lawrence CK, Adam H, Schweizer F, Zelenitsky S, Zhanel M, et al. Imipenem-relebactam and meropenem-vaborbactam: two novel carbapenem-β-lactamase inhibitor combinations. Drugs. 2018; 78(1):65–98.

89. Zhang Y, Kashikar A, Bush K. In vitro activity of plazomicin against β-lactamase-producing carbapenem-resistant Enterobacteriaceae (CRE). J Antimicrob Chemother. 2017; 72(10):2792–2795.
90. Martins AF, Bail L, Ito CA, da Silva Nogueira K, Dalmolin TV, Martins AS, et al. Antimicrobial activity of plazomicin against Enterobacteriaceae-producing carbapenemases from 50 Brazilian medical centers. Diagn Microbiol Infect Dis. 2018; 90(3):228–232.
91. Livermore DM, Mushtaq S, Warner M, Zhang JC, Maharjan S, Doumith M, et al. Activity of aminoglycosides, including ACHN-490, against carbapenem-resistant Enterobacteriaceae isolates. J Antimicrob Chemother. 2011; 66(1):48–53.
92. Galimand M, Courvalin P, Lambert T. Plasmid-mediated high-level resistance to aminoglycosides in Enterobacteriaceae due to 16S rRNA methylation. Antimicrob Agents Chemother. 2003; 47(8):2565–2571.
93. Zarubica T, Baker MR, Wright HT, Rife JP. The aminoglycoside resistance methyltransferases from the ArmA/Rmt family operate late in the 30S ribosomal biogenesis pathway. RNA. 2011; 17(2):346–355.

94. Doi Y, Wachino JI, Arakawa Y. Aminoglycoside resistance: the emergence of acquired 16S ribosomal RNA methyltransferases. Infect Dis Clin North Am. 2016; 30(2):523–537.
95. Choi JJ, McCarthy MW. Cefiderocol: a novel siderophore cephalosporin. Expert Opin Investig Drugs. 2018; 27(2):193–197.

96. Ito A, Sato T, Ota M, Takemura M, Nishikawa T, Toba S, et al. In vitro antibacterial properties of cefiderocol, a novel siderophore cephalosporin, against gram-negative bacteria. Antimicrob Agents Chemother. 2017; 62(1):e01454–17.

97. Aoki T, Yoshizawa H, Yamawaki K, Yokoo K, Sato J, Hisakawa S, et al. Cefiderocol (S-649266), a new siderophore cephalosporin exhibiting potent activities against Pseudomonas aeruginosa and other gram-negative pathogens including multi-drug resistant bacteria: structure activity relationship. Eur J Med Chem. 2018; 155:847–868.








 PDF
PDF Citation
Citation Print
Print






 XML Download
XML Download