This article has been
cited by other articles in ScienceCentral.
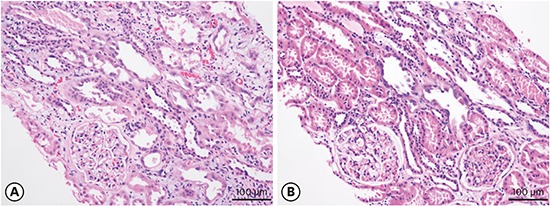

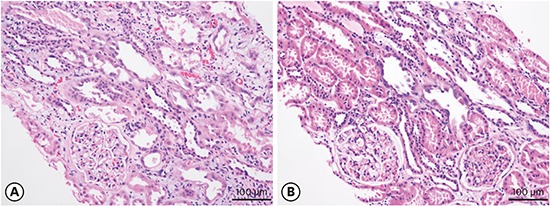
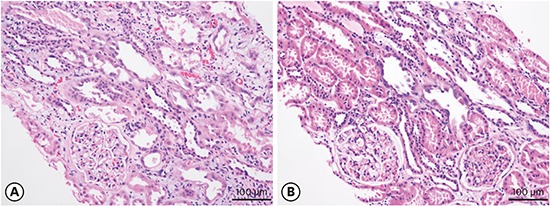
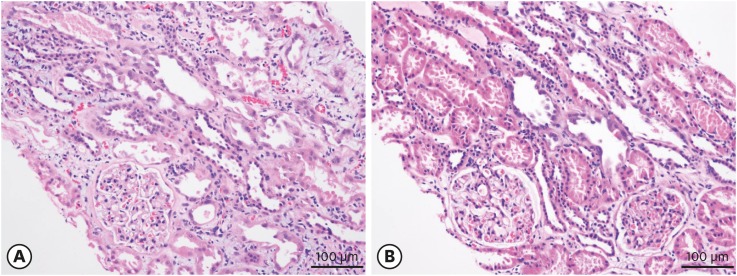
A 67-year-old man and his wife, a 63-year-old woman, were referred with elevated serum creatinine (s-Cr) levels. He had no known underlying disease and she had pre-existing hypertension and dyslipidemia, for which she was taking amlodipine 5 mg/day and rosuvastatin 10 mg/day. Three days prior, they ate wild mushrooms that looked like
Tricholoma matsutake, which is very expensive in Korea. The next day, they developed generalized weakness, nausea, and loose stools. They firstly visited private clinics and received symptomatic treatment. However, the creatinine level of the couple was increased to 9.79 mg/dL in the man (normal range: 0.8–1.2 mg/dL) and 3.06 mg/dL in the woman. They did not complain of fever, chills, abdominal pain, or anuria. Acute kidney injury (AKI) was suspicious on ultrasonography findings in both. We performed renal biopsy and revealed tubular dilatation with tubular epithelial flattening, coagulative necrosis of the tubular epithelial cells with an intraluminal granular cast, and extensive regenerative changes (
Fig. 1A) in the man. His wife's renal biopsy also showed acute tubular necrosis (ATN) with epithelial cell regeneration (
Fig. 1B). Therefore, conservative treatment without RRT was continued with crystalloids 1–2 mL/kg/hr. On hospital day (HD) 4, s-Cr elevated at 11.4 mg/dL. After HD 4, his urine output increased to 3,000–4,000 mL/day and on HD 14, his creatinine level had improved to 2.4 mg/dL. His wife's lab values also normalized on HD 8. We asked a mycologist to get mushrooms from the mountains which the couple took the mushrooms and the leftover mushrooms in the patients' refrigerator. She identified them with Melzer's reagent and morphology as
Amanita neoovoidea (
Fig. 2).
The fungal genus
Amanita is divided into seven sections.
1
A. neoovoidea, like
Amanita ovoidea, are grouped in the section
Amidella within the species
Amanita. It is found in areas from middle Japan to China and Nepal.
2 The genus
Amanita contains both edible and inedible forms, including dangerous and sometimes even deadly ones. Despite the number of studies performed on this genus, the toxicity of some species, such as the group of white fungi, remains indeterminate.
3 According to previous reports,
Amanita virosa, Amanita verna, and
Amanita subjunquillea are leading causes of mushroom poisoning in Korea.
4 Thirty-five patients showed marked elevations in alanine aminotransferase (ALT), and 7 patients died because of AKI and hepatic failure.
Amanita punctata has been reported as a cause of acute renal failure in Korea.
5 The clinical symptoms in this case resemble the course observed with
Amanita smithiana poisoning in Western North America.
6 These findings are similar with cases of poisoning due to the
A. smithiana toxin, the same toxic agent found in
A. neoovoidea, which caused several cases of poisoning in the United States from 1986.
78 The
A. smithiana was ingested raw or after cooking. Symptoms appeared in 4 to 10 hours, including vomiting, diarrhea, and abdominal pain, and after 2 to 3 days complete, but reversible, renal failure occurred.
78
Amanita nephrotoxic syndrome refers to mushroom poisoning characterized by early onset of gastrointestinal symptoms, mild ALT elevation, and AKI with acute interstitial nephritis.
1 Our patients had ATN rather than acute interstitial nephritis with regenerating epithelial cells. This suggests that it is a direct toxin effect rather than an immunologic response.
In conclusion, A. neoovoidea might induce AKI and it would be wise not to ingest wild mushrooms except after proper identification by a trained mycologist.
Fig. 1
Attenuation of tubular epithelial cells with intraluminal proteinaceous cellular debris is noted. Regenerative changes, such as pleomorphic hyperchromatic nuclei, basophilic cytoplasm, and occasional mitotic figures, are also noted. Intraluminal granular casts, interstitial inflammatory cells, and red blood cells extravasation is also present. (A) Husband's kidney biopsy and (B) his wife's kidney biopsy (magnification × 200).
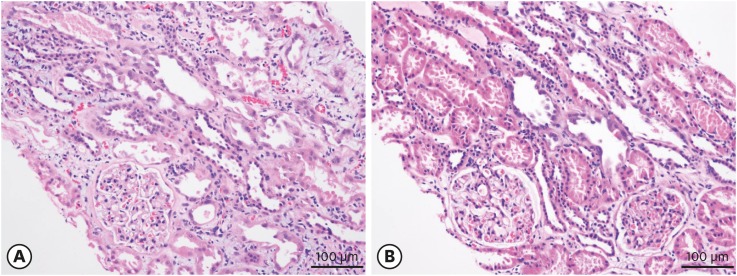
Fig. 2
Amanita neoovoidea eaten by patients. (A) Gross image of the A. neoovoidea. (B) Carpophores of A. neoovoidea, cause amyloid reaction in Melzer's reagent (magnification × 100).