INTRODUCTION
It is apparent that voiding dysfunction, including benign prostatic hyperplasia (BPH)/lower urinary tract symptoms (LUTS) and neurogenic bladder, shows a higher prevalence with age.
12 Due to high prevalence of these types of voiding dysfunction, especially considering the shift of society to an old-aged society, they are becoming important social health problems.
1
Among the medical expenses for voiding dysfunction, the examination fees account for a large portion because evaluation is important during both screening and monitoring. Uroflowmetry, urodynamic study and cystoscopy are important examination tools during both initial evaluation of LUTS and monitoring after medication or surgical procedures. It is very important to predict the exact medical expenses for voiding dysfunction because in the future with an increase in the population of aged society, the medical expenses could increase due to rapid shift to an old aged society or could diminish due to increasing aged subject with limitative income.
However, rarely, studies have reported the trend of these examination tools including uroflowmetry, urodynamic study and cystoscopy. To date, there are several important studies that have reported the national trend for urodynamic study.
34 In these reports, unlike the regular mere expectation that urodynamic study would show a pattern of an increasing trend due to increasing prevalence of voiding dysfunction according to the increase in aged population, the recent trend showed a sharp decreasing pattern.
34 With respect to uroflowmetry and cystoscopy, there are no studies showing the trend of their performance. Considering the increasing prevalence of bladder cancers as well as voiding dysfunction,
56 cystoscopy might show an increasing pattern.
Considering the unique characteristics of demographic phenomena in our era, the rapidly aging society warrants that the clinicians should urgently understand the interaction between aging and medical consumption or provision pattern.
7 Moreover, according to the global aging phenomenon, the medical cost related to screening and monitoring of LUTS will increase continuously.
8
Korea is one of the countries with a rapidly aging society. Moreover, population growth and birth rate in Korea are extremely low compared with other countries, and also the economic entity has aged at a rapid speed. Hence, considering the global aging shift, performing research on the Korean society would be a good sample to predict the future medical consumption pattern.
We hypothesized that national trend of uroflowmetry, urodynamic study and cystoscopy would show either an increasing or a decreasing pattern after adjustment for the aging shift. To validate this hypothesis, we used national health data. The National Health Insurance (NHI) program in Korea was initiated in 1977 and it achieved universal coverage of the population by 1989. The Health Insurance Review and Assessment (HIRA) service covers the claims of 99.0% of the population in Korea; those of the remaining 3% of the population are covered by the Medical Aid Program. Accordingly, the HIRA database contains information on almost the entirety of the insurance claims, including prescribed medications and procedures, for the Korean population of approximately 50 million.
9
METHODS
Data collection
We used HIRA data recorded between January 1st, 2010 to December 30th, 2015. The HIRA database contains information on all insurance claims for about 99.0% of the population in Korea.
9 The HIRA service provided the data after de-identification, and the data included age, gender, diagnosis, date of hospital visits, drug prescriptions received during inpatient and outpatient visits, hospital admissions, medical procedures, and emergency department visits. Diagnoses were coded according to the International Classification of Diseases, 10th revision (ICD-10). To investigate the true annual frequency rate of uroflowmetry, urodynamic study and cystoscopy, we counted the number of patients in whom the relevant procedure was performed.
We used the Healthcare Common Procedure Coding System codes provided by the HIRA service to identify the associated procedure or surgery. The codes related to the procedure or surgery were uroflowmetry (EY521), urodynamic study (E6560), cystoscopy (E7730). Cystometry (E6561) and urethral pressure measurement (EX751) were included in urodynamic study (E6560). Matching ICD-10 codes such as those for BPH or neurogenic bladder with procedural codes was not necessary. Repeated claim codes in the same patients were only regarded as a single frequency of performance of each procedure.
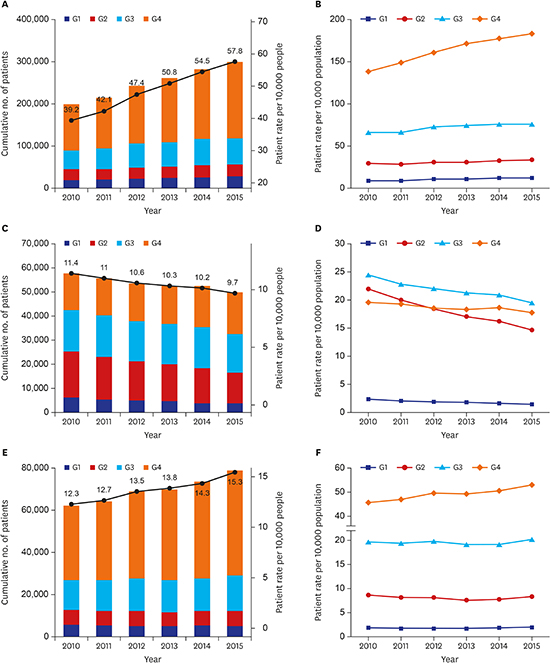
Measurement outcomes
There were three main measurement outcomes including cumulative number of patients per year (model 1: patient rate per 10,000 people), cumulative age-standardized patient rate per 10,000 people (model 2: to investigate the annual frequency rate after adjustment for age and age groups), and correlation between the number of patients per year and the percentage of population per year (model 3: to investigate the impact of population structure change on frequency of procedures). For age-standardization, we used the following formula: number of patients (for the year) × 10,000/total population (for the year). For model 3, we used a formula to describe the age groups as follows: the total number of patients in the age group (for the year) × 100/ (for the year).
Data analysis
Population data was obtained from Survey Management Bureau, National Statistical Office. Data synthesis and analysis were performed as described below. First, calculation of the total population per year for all Koreans was performed using data of National Statistical Office. Second, calculation of total patient number per year was performed for the relevant procedure code using HIRA data. Third, analysis was performed for cumulative patient rates per 10,000 people according to the year (model 1). Fourth, analysis was performed for cumulative age-standardized patient rate per 10,000 people according to the year and age group (model 2). During this analysis, generalized linear model (GLM) was used and the results were displayed as the estimate with standard error (SE) and plotted as a line graph. Finally, analysis was performed for correlation coefficients between patient rates per 10,000 people and percentage of population (model 3) using Pearson correlation analysis. We considered P value < 0.05 to be “statistically significant” and all data were analyzed using R (v3.1.2; R Foundation, Vienna, Austria).
DISCUSSION
This investigation shows the result of national trend of uroflowmetry, urodynamic study and cystoscopy, considering age shifting over the last 5 years. To date, this is the first report to consider the age shifting phenomenon in urologic disease. Moreover, this study includes detailed analysis regarding the association between change of age structure and cumulative frequencies of each procedures, which could reflect the aging structural change. However, considering the large impact of this result, interpretation of this result should be performed with caution and two points have to be considered. This result could reflect the preference and compliance of patients or it could reflect the power of recommendation made by clinicians.
The possible reasons according to the results of tendency for uroflowmetry, urodynamic and cystoscopy will be discussed in this section. First, uroflowmetry, contrary to the decreasing trend of urodynamic study, shows a significantly increasing pattern over the years and also according to age shifting. To date, there is controversy regarding the validity and reproducibility of uroflowmetry to predict bladder outlet obstruction or detrusor underactivity.
10
Besides the controversy about the validity and reproducibility, the current trend of uroflowmetry is increasing according to both years and adjustment of age shifting. Possible reasons for the occurrence of this phenomenon include simplicity and rapidity in both performance and interpretation. It is also true that its installation cost is relatively low.
For urodynamic test, the current trend of decreasing pattern according to age and age shifting is ironic. In the aged population, the prevalence of voiding dysfunction is high in both men and women.
34 Moreover, urodynamic test is the gold standard test for evaluating BPH/LUTS, stress urinary incontinence (SUI) and neurogenic bladder.
311
It is a coincidence that the US National data about this urodynamic study also shows a recent sharp decrease.
34 Due to possible reasons in men, BPH guidelines do not support the routine use of urodynamic study unless the patients have obstructive symptoms and urinary flow rate < 10 mL/s.
2 Moreover, urodynamic study leads to secondary urinary tract infections and other adverse events including hematuria, irritative symptoms and urethral stricture.
2
Due to possible reasons in women, there is a controversy about performance of urodynamic study for making a confirmative diagnosis and cost-effectiveness.
1213 The current trend of recommendations is turning negative with respect to performance of urodynamic study in women with SUI. In women undergoing primary surgery for SUI or stress-predominant mixed urinary incontinence (MUI) without voiding difficulties, urodynamics does not improve outcomes — as long as the women undergo careful office evaluation.
Considering the most frequent performance of urodynamic study for SUI or MUI among women in the US,
3 we have to think about the recent prevalence of SUI or the frequency of operation for SUI. In Korea, the performance of urodynamic study while preparing for the operation for SUI is obligatory; hence, the result of our study could reflect the current trend of decreasing rate of operation for SUI (
Supplementary Table 1). Recently, Cho et al.
14 reported that the number of surgical cases of SUI decreased continuously from 2008 to 2011. Besides these reasons, there may be more possible reasons in both men and women such as urodynamic test has a relatively high cost for equipment and skillful training for a long time is required for its performance and interpretation.
For cystoscopy, the trend is increasing with age and age shifting. Cystoscopy, especially flexible cystoscopy is an effective, well-tolerated and easy way of detecting lower urinary tract findings including those in the urethra, prostate and bladder.
2 Especially the trend of cystoscopy correlates significantly with age shifting over 60 years, which implies that cystoscopy is usually performed in the aged population and its frequency is increasing in this population. This is attributable to the wide indications of cystoscopy, although it is not routine recommended test for LUTS, which are not confined to only voiding dysfunction but also include hematuria and bladder tumor.
This pioneer investigation has several limitations. First, although the national health data was used, a more detailed approach including defining the disease cohort is needed. However, this is not easy, and for considering the national trend, defining an intentional cohort does not guarantee a more high quality study. Moreover, subgroup analysis according to sex, surgery types, emergency or outpatient department visiting, and the category of hospital including primary or tertiary (academic) hospital were not performed in this study. The aim of this study was to investigate the general trend and age impact on the trend. Due to the short period, multi-variable analysis was impossible. According to the category of hospital, the general trend was also similar (
Supplementary Table 2). Second, we could not consider sociodemographic factors and hence, we could not investigate their relationship with the preference and compliance of patients. Third, five years could be not enough to investigate a national trend. Fourth, a cost-effectiveness analysis or a cost burden study using this National Health Data is necessary to investigate the potential impact of this result on future medical care circumstances. Lastly, due to not defining each disease cohort, this study could not provide which procedures were done in each specific urologic disease.
In conclusion, national trend of urologic procedures for assessing voiding dysfunction shows different trends among uroflowmetry, urodynamic test and cystoscopy. Considering that Korea is one of the top countries with a rapidly aging society, this tendency could reflect the current pattern for diagnostic procedures for voiding dysfunction. Future studies are needed to investigate the correlation between decreasing pattern of urodynamic study and BPH surgery or surgery for SUI.






 PDF
PDF Citation
Citation Print
Print





 XML Download
XML Download