Introduction
materials and Methods
Results
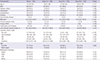
Table 1
Baseline characteristics of patients according to uric acid level
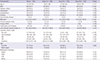
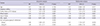
Table 2
Clinical outcomes of the total population according to uric acid level

Fig. 2

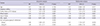
Table 3
Prognostic factors for MACEs
Journal List > J Korean Med Sci > v.32(8) > 1108455


Author Contributions
Conceptualization: Gwon HC, Choi SH.
Data curation: Gwag HB, Park TK, Song YB, Hahn JY, Choi JH, Lee SH, Gwon HC, Choi SH.
Formal analysis: Gwag HB, Yang JH.
Investigation: Gwag HB, Yang JH, Park TK, Song YB, Hahn JY, Choi JH, Lee SH.
Methodology: Gwag HB, Yang JH.
Project administration: Choi SH.
Resources: Gwag HB, Yang JH, Park TK, Song YB, Hahn JY, Choi JH, Lee SH, Gwon HC, Choi SH.
Software: Gwag HB, Yang JH.
Supervision: Gwon HC, Choi SH.
Validation: Yang JH, Choi SH, Gwon HC.
Visualization: Gwag HB, Yang JH.
Writing - original draft: Gwag HB, Yang JH.
Writing - review & editing: Lee SH, Gwon HC, Choi SH.
Hye Bin Gwag 
https://orcid.org/0000-0001-5610-2872
Jeong Hoon Yang 
https://orcid.org/0000-0001-8138-1367
Taek Kyu Park 
https://orcid.org/0000-0003-1440-3583
Young Bin Song 
https://orcid.org/0000-0002-2581-8891
Joo-Yong Hahn 
https://orcid.org/0000-0002-4412-377X
Jin-Ho Choi 
https://orcid.org/0000-0002-5421-793X
Sang Hoon Lee 
https://orcid.org/0000-0003-1202-917X
Hyeon-Cheol Gwon 
https://orcid.org/0000-0002-8967-4305
Seung-Hyuk Choi 
https://orcid.org/0000-0002-0304-6317