This article has been
cited by other articles in ScienceCentral.
Abstract
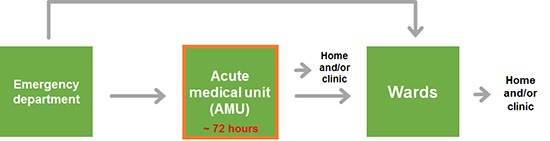
A hospitalist-run acute medical unit (AMU) opened at a tertiary care hospital on August 2015 for the first time in Korea. Patients visiting the emergency department (ED) with acute medical problems are admitted to the AMU. They stay in that unit for less than 72 hours and are discharged or transferred to specialty wards if longer treatment is necessary. We reviewed 19,450 medical admissions through the ED from January 2014 to September 2016. The median length of stay (LOS) significantly decreased from 10.0 days (interquartile range [IQR], 5.5–16.7) to 9.1 days (IQR, 5.1–15.0) (P < 0.001) after the establishment of the AMU. The median waiting time in the ED significantly shortened by 40% (P < 0.001). Future studies on the impact of AMU on in-patient morbidity, mortality, re-admission rate, and patient or staff satisfaction are necessary.
Keywords: Hospital Medicine, Length of Stay, Hospitalists, Emergency Service, Hospital
INTRODUCTION
Recently, the necessity of hospital medicine has been thoroughly discussed in Korea to improve the quality of inpatient care and to solve the shortage of medical residents with the reduced duration of medical residency train programs to three years (
123). The hospitalist, or hospital-based general physician, is specialized in inpatient care, and there are now over 50,000 hospitalists in the United States (
45). The hospitalist care model has reduced healthcare costs and improved the safety and quality of patient care (
67).
On the other hand, in the United Kingdom, acute medicine emerged to improve the early management of acutely ill hospitalized patients (
89). Acute physicians focus on the first few days of inpatient care, and they usually manage patients within an acute medical unit (AMU). Patients not discharged within 48–72 hours from the AMU are routinely transferred to the most suitable specialty ward. Acute medicine is the fastest growing specialty in the UK, and the field grew by 63% with respect to the number of acute physicians between 2002 and 2007 (
10).
Both hospitalists and acute physicians are generalists who take care of inpatients, and they developed with different social backgrounds and national policies in the two countries (
11). At our hospital, we adopted the acute medicine model and started an AMU with 20 beds in August 2015, which was expanded to 28 beds in July 2016. In the present study, we analyzed the impact of the AMU on the length of stay (LOS) and waiting time in the emergency department (ED) before admission.
MATERIALS AND METHODS
Patients with acute medical conditions are admitted to the AMU or specialty wards through the ED. According to our AMU admission policy, any patients referred from the ED with acute medical conditions are admitted to the AMU except those with any of the following contraindications: hemodynamic instability requiring invasive monitoring and/or critical care facilities; patients with cancer who require only palliative or end-of-life care. When patients are admitted to the AMU, they stay for ≤ 72 hours before they are discharged directly from the AMU or transferred to a specialty ward if further care is necessary. The AMU is operational 24 hours a day and 7 days a week. Two hospitalists are present for 13 hours per day, from 8 AM to 9 PM. They are given the full authority regarding the operation policies of the AMU and the decision on admissions to the AMU and specialty wards. Close communication with subspecialty faculties is maintained by written consultation or direct phone call.
The LOS is defined as the duration of a single episode of hospitalization, and it is calculated by subtracting the day of admission from the day of discharge. The data on the LOS of admissions to internal medicine wards through the ED from January 2014 to September 2016 were retrieved from the clinical data warehouse (CDW) of our electronic health records system. Data related to the waiting time in the ED before admission to internal medicine wards from July 2014 until September 2016 were also retrieved from CDW. As the LOS and waiting time in the ED had a skewed distribution, they were fitted to a gamma distribution, and median and interquartile ranges (IQRs) were calculated. The statistical significance in the differences in the LOS and waiting times in the ED between groups was calculated using the Mann-Whitney U test. Statistical data analyses were performed with the R statistics package (R Foundation, Vienna, Austria;
https://www.r-project.org).
Ethics statement
The study protocol was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No. B-1511/324-302). Written informed consent was waived because data were collected by retrospective record review.
RESULTS
We analyzed 19,450 admissions to internal medicine wards through the ED from January 2014 to September 2016. After establishing the AMU in August 2015, there were 9,514 admissions to internal medicine wards and 3,141 admissions to the AMU until September 2016. Of the 3,141 admissions, 694 (22%) patients were discharged from the AMU without transfer to specialty wards. Patients who were directly discharged from the AMU after a short stay had diagnoses like neutropenic fever, acute pyelonephritis, asthma exacerbation, peptic ulcer bleeding, acute kidney injury, etc.
The median LOS significantly shortened from 10.0 days (IQR, 5.5–16.7) to 9.1 days (IQR, 5.1–15.0) (
P < 0.001) after the introduction of the AMU in August 2015 (
P < 0.001).
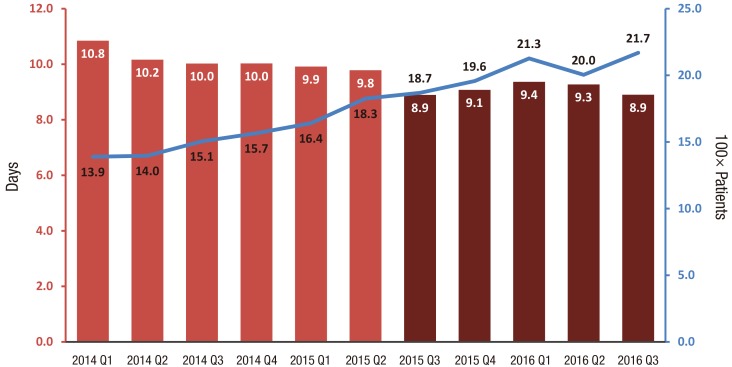
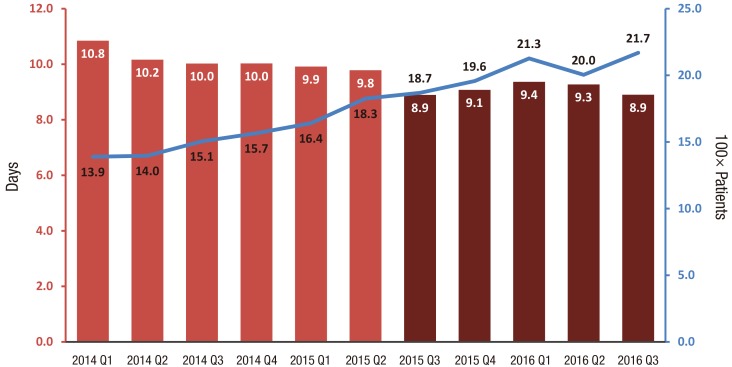
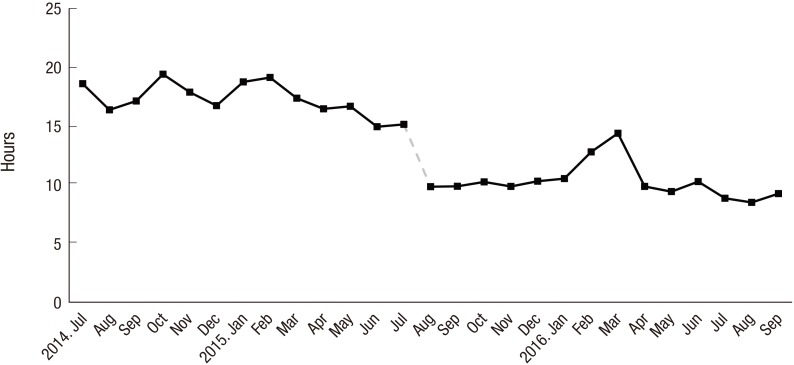
Fig. 1 shows the quarterly change in the LOS during the 33-month period. The median LOS begins to decrease from the third quarter of 2015 when the AMU was introduced. With the decrease in the LOS, there was a concomitant increase in the number of admissions to internal medicine wards through the ED (
Fig. 1).
Fig. 1
The quarterly change in the median LOS and the number of admissions to internal medicine wards through the ED. The number in each bar indicates the median LOS in each quarter before (red bars) and after (dark red bars) the introduction of the AMU. With a reduction in the LOS, there was a concomitant rise in the number of admissions to the internal medicine wards through the ED (blue line and right axis).
LOS = length of stay, ED = emergency department, AMU = acute medical unit.
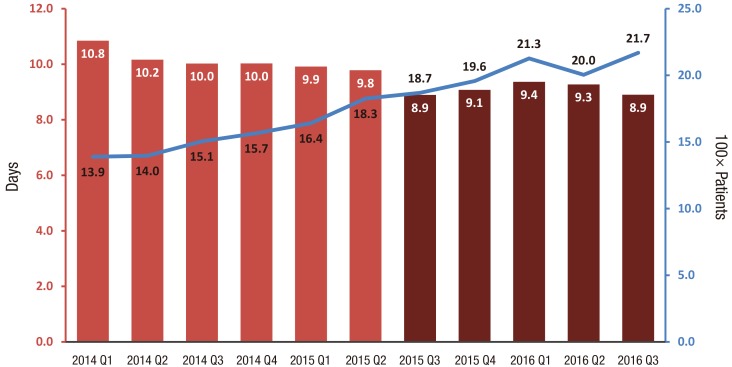
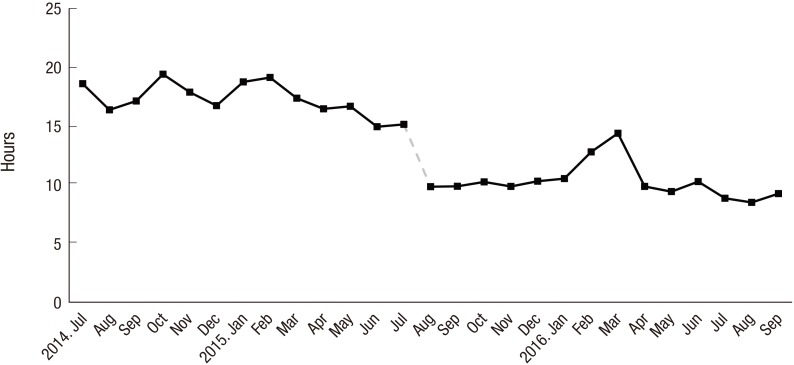
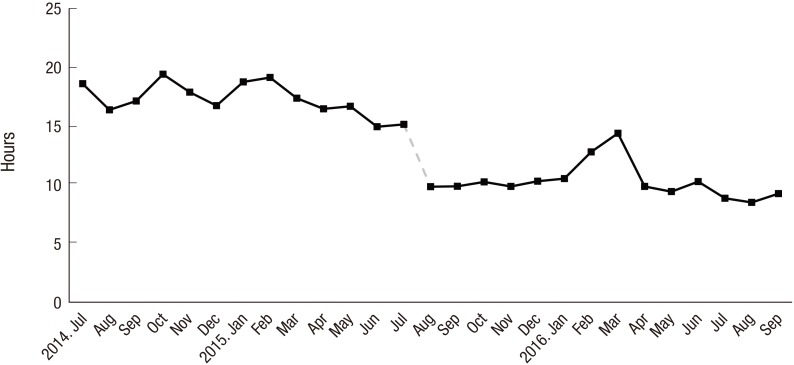
In
Fig. 2, the median waiting time in the ED before admission to internal medicine wards was 17.1 (IQR, 8.4–30.6) hours between July 2014 and July 2015. It significantly decreased to 10.2 (IQR, 5.9–16.3) hours by 40% after the AMU was introduced in August 2015 (
P < 0.001). The waiting time in the ED decreased despite the increased number of admissions to internal medicine wards, as is shown in
Fig. 1. The proportion of patients who stayed longer than 24 hours in the ED before admission was 40% before August 2015, and it was reduced to less than 5% after the opening of the AMU.
Fig. 2
The median waiting time in the ED before admission to internal medicine wards. After the AMU was introduced in August 2015, the waiting time decreased from 17.1 (IQR, 8.4–30.6) to 10.2 (IQR, 5.9–16.3) hours (by 40%), which persisted to September 2016.
ED = emergency department, AMU = acute medical unit, IQR = interquartile range.
DISCUSSION
This is the first study to show that the introduction of the AMU in a Korean tertiary care hospital decreased the median LOS and shortened the waiting time in the ED. The median LOS significantly decreased by one day, which suggests that adequate and rapid management by hospitalists in the early phase of acute illness and their efficient operation of the AMU have contributed to reduce the total LOS. The waiting time in the ED was reduced by 40%, which persisted until the end of the observation period.
Previous studies suggested that AMUs reduce the waiting time for transfer from the ED to wards, length of admission, and in-patient mortality without increasing the readmission rates (
1213141516). Additionally, they improve patient and staff satisfaction. The establishment of the AMU at St. James's Hospital, in a retrospective study of 10,566 admissions over 2 years, was associated with a significant reduction in the median LOS for medical admissions from 6 to 5 days (
12). In a retrospective study of 3,163 medical admissions to Chelsea and Westminster Hospital, the average LOS significantly decreased from 9.3 to 7.8 days after 4 months of the AMU operation (
17). A similar result was reported at Stobhill Hospital in Scotland, where the average length of hospital stay decreased from 7.0 to 4.5 days (
18). Consistent with previous studies, the operation of the AMU in a Korean tertiary care hospital also reduced the LOS.
The AMU of our study is distinguished from other emergency short stay units in Korea, commonly known as Emergency Wards which are usually run by emergency physicians as a part of the ED and mainly admit patients who are overflowing in the ED. Patients are actively admitted to the AMU in the early phase of illness and receive rapid assessment and management by internists who are experienced in the care of patients with acute medial illnesses.
Our AMU began with three internists with subspecialty board-certification in infection, pulmonology and critical care, and endocrinology. A strength of the program is the direct, real-time communication among team members with diverse specialty training, which helps to make appropriate, rapid care decisions for acutely ill patients.
Beyond providing timely and adequate care for patients with acute illness, hospitalists actively participate in educating medical residents and performing research. A daily case conference is held in the morning, and it is discussed with medical residents with a focus on how to assess and make plans for patients staying in the AMU and ED. The acute medicine team also shares interesting and educational cases as well as provides staff lectures in the department of medicine.
When we reviewed the trend in ED waiting times, the waiting time began to decrease in March 2015, which was before the AMU was established (
Fig. 2). The median waiting time decreased from 17.9 hours to 16.1 hours (by 10%) from March 2015 when two medical board-certified physicians started to work in the ED. The rapid assessment and decision for admission by the experienced internists, rather than by medical residents, may have contributed to reducing the waiting time in the ED. Additionally, there was a transient increase in the ED waiting time from February to March 2016 (
Fig. 2). One of the contributing factors seems to be the decrease in discharges from medical beds as first-year medical residents started to work in March. This suggests that maintaining an adequate bed turnover rate is crucial to controlling the ED waiting time even when the AMU operates within a hospital.
This study is limited by the observational study design, and we could not correct for other factors that could have affected the LOS and waiting time in the ED. Additionally, other quality indicators, such as the morbidity, mortality, re-admission rate, and patient or staff satisfaction, were not included in the present study.
In summary, we provide evidence that the AMU in a Korean tertiary care hospital reduces the LOS and shortens the ED waiting time. Future study is necessary if the introduction of the AMU will improve the quality of inpatient care with respect to outcomes, such as the morbidity, mortality, re-admission rate, and patient or staff satisfaction.